Abstract
Background
To clarify the clinicopathological features of breast cancer in young females, surveillance data of the Registration Committee of the Japanese Breast Cancer Society were analyzed.
Methods
The clinicopathological characteristics were compared between young (<35) patients and non-young (≥35) patients among 109,617 records registered between 2004 and 2009.
Results
The numbers of young and non-young patients were 2,982 (2.7 %) and 106,295 (97.0 %), respectively. The young patients had more cases of a familial history of breast cancer, more subjective symptoms, fewer bilateral tumors, lower BMIs, larger tumors, more positive lymph nodes, fewer instances of an ER-positive status, more instances of an HER2-positive status, more triple-negative tumors and more advanced TNM stages. The young patients more frequently received neoadjuvant chemotherapy and breast-conserving therapy (BCT) compared with the non-young patients. Eighty percent of all patients received adjuvant therapy. The young patients were more frequently treated with chemotherapy, molecular targeted therapy and radiation therapy than the non-young patients.
Conclusions
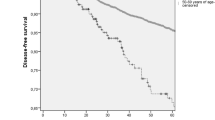
In this study, young patients with breast cancer were diagnosed at more advanced stages and had more endocrine-unresponsive tumors than non-young patients. Further prognostic analyses should be conducted in this cohort.


Similar content being viewed by others
References
Matsuda T, Marugame T, Kamo KI, Katanoda K, Ajiki W, Sobue T. Cancer incidence and incidence rates in Japan in 2006: based on data from 15 population-based cancer registries in the monitoring of cancer incidence in Japan (MCIJ) project. Jpn J Clin Oncol. 2012;42:139–47.
Anders CK, Hsu DS, Broadwater G, Acharya CR, Foekens JA, Zhang Y, et al. Young age at diagnosis correlates with worse prognosis and defines a subset of breast cancers with shared patterns of gene expression. J Clin Oncol. 2008;26(20):3324–30.
Gonzalez-Angulo AM, Broglio K, Kau SW, Eralp Y, Erlichman J, Valero V, et al. Women age <35 years with primary breast carcinoma disease features at presentation. Cancer. 2005;103:2466–72.
Ahn SH, Son BH, Kim SW, Kim SI, Jeong J, Ko SS, et al. Poor outcome of hormone receptor positive breast cancer at very young age is due to tamoxifen resistance: nationwide survival data in Korea-A report from the Korean Breast Cancer Society. J Clin Oncol. 2007;25:2360–8.
Aebi S, Gelber S, Castiglione-Gertsch M, Gelber RD, Collins J, Thürlimann B, et al. Is chemotherapy alone adequate for young women with oestrogen-receptor-positive breast cancer? Lancet. 2000;27:1869–74.
Colleoni M, Rotmensz N, Robertson C, Orlando L, Viale G, Renne G, et al. Very young women (<35 years) with operable breast cancer: features of disease at presentation. Ann Oncol. 2002;13(2):273–9.
Pronzato P, Mustacchi G, DeMatteis A, Di Costanzo F, Rulli E, Floriani I, et al. Biological characteristics and medical treatment of breast cancer in young women—a featured population: results from the nora study. Int J Breast Cancer. 2011, Article ID 534256, doi:10.4061/2011/534256.
Pagani O, O’Neill A, Castiglione M, et al. Prognostic impact of amenorrhoea after adjuvant chemotherapy in premenopausal breast cancer patients with axillary node involvement: results of the International Breast Cancer Study Group (IBCSG) Trial VI. Eur J Cancer. 1998;34:632–40.
The Japanese breast cancer society. General roles for clinical and pathological recording of breast cancer.16th ed. Histological Classification of breast tumors. Tokyo: The Japanese breast cancer society; 2008. 18–59.
The World Health Organization. World Health Organization histological typing of breast tumors. Am J Clin Pathol. 1982;78:806–16.
Harvey JM, Clark GM, Osborne CK, Allred DC. Estrogen receptor status by immunohistochemistry is superior to the ligand-binding assay for predicting response to adjuvant endocrine therapy in breast cancer. J Clin Oncol. 1999;17:1474–81.
Umemura S, Kurosumi M, Moriya T, Oyama T, Arihiro K, Yamashita H, et al. Immunohistochemical evaluation for hormone receptors in breast cancer: a practically useful evaluation system and handling protocol. Breast cancer. 2006;13:232–5.
Leong SP, Shen ZZ, Liu TJ, Agarwal G, Tajima T, Paik NS, et al. Is breast cancer the same disease in Asian and Western Countries? World J Surg. 2010;34(10):2308–24.
Howlader N, Noone AM, Krapcho M, Neyman N, Aminou R, Altekruse SF, et al. SEER cancer statistics review, 1975–2009 (Vintage 2009 Populations), National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2009_pops09/, based on November 2011 SEER data submission, posted to the SEER web site, 2012.
Yoshimoto M, Tada K, Hori H, Morota A, Tanabe M, Nishimura S, et al. Improvement in the prognosis of Japanese breast cancer patients from 1946 to 2001-an institutional review. Jpn J Clin Oncol. 2004;34(8):457–62.
Saeki T, Sano M, Komoike Y, Sonoo H, Honjyo H, Ochiai K, et al. No increase of breast cancer incidence in Japanese women who received hormone replacement therapy: overview of a case-control study of breast cancer risk in Japan. Int J Clin Oncol. 2008;13(1):8–11.
http://www.mhlw.go.jp/topics/bukyoku/kenkou/seikatu/himan/number.html.
Sugano K, Nakamura S, Ando J, Takayama S, Kamata H, Sekiguchi I, et al. Cross-sectional analysis of germline BRCA1 and BRCA2 mutations in Japanese patients suspected to have hereditary breast/ovarian cancer. Cancer Sci. 2008;99(10):1967–76.
Shi YX, Xia Q, Peng RJ, Yuan ZY, Wang SS, An X, et al. Comparison of clinicopathological characteristics and prognoses between bilateral and unilateral breast cancer. J Cancer Res Clin Oncol. 2012;138(4):705–14.
Iwase H, Kurebayashi J, Tsuda H, Ohta T, Kurosumi M, Miyamoto K, et al. Clinicopathological analyses of triple negative breast cancer using surveillance data from the Registration Committee of the Japanese Breast Cancer Society. Breast Cancer. 2010;17:118–24.
Anders CK, Fan C, Parker JS, Carey LA, Blackwell KL, Klauber-DeMore N, et al. Breast carcinomas arising at a young age: unique biology or a surrogate for aggressive intrinsic subtypes? J Clin Oncol. 2011;29(1):e18–20.
Saji S, Hiraoka M, Tokuda Y, Fukui N, Ikeda T. Trends in local therapy application for early breast cancer patients in the Japanese Breast Cancer Society Breast Cancer Registry during 2004–2009. Breast Cancer. 2012;19:1–3.
Freedman RA, Virgo KS, Labadie J, He Y, Partridge AH, Keating NL. Receipt of locoregional therapy among young women with breast cancer. Breast Cancer Res Treat. 2012;135(3):893–906.
Buzdar AU, Ibrahim NK, Francis D, Booser DJ, Thomas ES, Theriault RL, et al. Significantly higher pathologic complete remissionrate after neoadjuvant therapy with trastuzumab, paclitaxel, and epirubicin chemotherapy: results of a randomized trial in human epidermal growth factorreceptor 2-positive operable breast cancer. J Clin Oncol. 2005;23:3676–85.
Gianni L, Dafni U, Gelber RD, Azambuja E, Muehlbauer S, Goldhirsch A, et al. Treatment with trastuzumab for 1 year after adjuvant chemotherapy in patients with HER2-positive early breast cancer: a 4-year follow-up of a randomised controlled trial. Lancet Oncol. 2011;12(3):236–44.
Wong M, O’Neill S, Walsh G, Smith IE. Goserelin with chemotherapy to preserve ovarian function in pre-menopausal women with early breast cancer: menstruation and pregnancy outcomes. Ann Oncol. 2012;. doi:10.1093/annonc/mds250 (First published online: September 27).
Acknowledgments
We wish to thank Mr. Naohito Fukui, the NPO Japan Clinical Research Support Unit staff and the Japanese Breast Cancer Society for their collaboration on this study and their ongoing development, maintenance and improvement of this registry. This work was supported by a research fund from the Japanese Breast Cancer Society.
Conflict of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Special Feature organized by Dr. Chikako Shimizu.
About this article
Cite this article
Kataoka, A., Tokunaga, E., Masuda, N. et al. Clinicopathological features of young patients (<35 years of age) with breast cancer in a Japanese Breast Cancer Society supported study. Breast Cancer 21, 643–650 (2014). https://doi.org/10.1007/s12282-013-0466-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-013-0466-2