Abstract
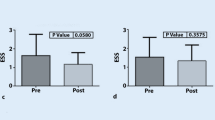
Biomechanical forces may play a key role in saphenous vein graft (SVG) disease after coronary artery bypass graft (CABG) surgery. Computed tomography angiography (CTA) of 430 post-CABG patients were evaluated and 15 patients were identified with both stenosed and healthy SVGs for paired analysis. The stenosis was virtually removed, and detailed 3D models were reconstructed to perform patient-specific computational fluid dynamic (CFD) simulations. Models were processed to compute anatomic parameters, and hemodynamic parameters such as local and vessel-averaged wall shear stress (WSS), normalized WSS (WSS*), low shear area (LSA), oscillatory shear index (OSI), and flow rate. WSS* was significantly lower in pre-diseased SVG segments compared to corresponding control segments without disease (1.22 vs. 1.73, p = 0.012) and the area under the ROC curve was 0.71. No differences were observed in vessel-averaged anatomic or hemodynamic parameters between pre-stenosed and control whole SVGs. There are currently no clinically available tools to predict SVG failure post-CABG. CFD modeling has the potential to identify high-risk CABG patients who may benefit from more aggressive medical therapy and closer surveillance.

Graphical Abstract






Similar content being viewed by others
References
D’Agostino, R. S., Jacobs, J. P., Badhwar, V., et al. (2019). The Society of Thoracic Surgeons Adult Cardiac Surgery Database: 2019 update on outcomes and quality. The Annals of Thoracic Surgery, 107(1), 24–32. https://doi.org/10.1016/j.athoracsur.2018.10.004.
Goldman, S., Zadina, K., Moritz, T., et al. (2004). Long-term patency of saphenous vein and left internal mammary artery grafts after coronary artery bypass surgery. Journal of the American College of Cardiology, 44(11), 2149–2156. https://doi.org/10.1016/j.jacc.2004.08.064.
Hess, C. N., Lopes, R. D., Gibson, C. M., et al. (2014). Saphenous vein graft failure after coronary artery bypass surgery insights from PREVENT IV. Circulation., 130(17), 1445–1451. https://doi.org/10.1161/CIRCULATIONAHA.113.008193.
Weintraub, W. S., Jones, E. L., Morris, D. C., King, S. B., Guyton, R. A., & Graver, J. M. (1997). Outcome of reoperative coronary bypass surgery versus coronary angioplasty after previous bypass surgery. Circulation., 95(4), 868–877. https://doi.org/10.1161/01.CIR.95.4.868.
De Vries, M. R., Simons, K. H., Jukema, J. W., Braun, J., & Quax, P. H. A. (2016). Vein graft failure: from pathophysiology to clinical outcomes. Nature Reviews Cardiology, 13(8), 451–470. https://doi.org/10.1038/nrcardio.2016.76.
Malek, A., Alpher, S., & Izumo, S. (1999). Hemodynamic shear stress and its role in atherosclerosis. Journal of American Medical Association, 282(21), 2035–2042.
Markl, M., Frydrychowicz, A., Kozerke, S., Hope, M., & Wieben, O. (2012). 4D flow MRI. Journal of Magnetic Resonance Imaging, 36, 1015–1036. https://doi.org/10.1002/jmri.23632.
Morris, P. D., Narracott, A., Von Tengg-Kobligk, H., et al. (2016). Computational fluid dynamics modelling in cardiovascular medicine. Heart, 102(1), 18–28. https://doi.org/10.1136/heartjnl-2015-308044.
Lu, M. T., Ferencik, M., Roberts, R. S., et al. (2017). Noninvasive FFR derived from coronary CT angiography—management and outcomes in the PROMISE trial. JACC: Cardiovascular Imaging, 10(11), 1350–1358. https://doi.org/10.1016/j.jcmg.2016.11.024.
Packard, R. R. S., Li, D., Budoff, M. J., & Karlsberg, R. P. (2017). Fractional flow reserve by computerized tomography and subsequent coronary revascularization. European Heart Journal Cardiovascular Imaging, 18(2), 145–152. https://doi.org/10.1093/ehjci/jew148.
Sankaran, S., Moghadam, M. E., Kahn, A. M., Tseng, E. E., Guccione, J. M., & Marsden, A. L. (2012). Patient-specific multiscale modeling of blood flow for coronary artery bypass graft surgery. Annals of Biomedical Engineering, 40(10), 2228–2242. https://doi.org/10.1007/s10439-012-0579-3.
Tran, J. S., Schiavazzi, D. E., Ramachandra, A. B., Kahn, A. M., & Marsden, A. L. (2016). Automated tuning for parameter identification and uncertainty quantification in multi-scale coronary simulations. Computers and Fluids, 142, 128–138. https://doi.org/10.1016/j.compfluid.2016.05.015.
Ramachandra, A. B., Kahn, A. M., & Marsden, A. L. (2016). Patient-specific simulations reveal significant differences in mechanical stimuli in venous and arterial coronary grafts. Journal of Cardiovascular Translational Research, 9(4), 279–290. https://doi.org/10.1007/s12265-016-9706-0.
Gaudino, M., Antoniades, C., Benedetto, U., et al. (2017). Mechanisms, consequences, and prevention of coronary graft failure. Circulation, 136(18), 1749–1764. https://doi.org/10.1161/CIRCULATIONAHA.117.027597.
Podesser, B. K., Neumann, F., Neumann, M., Schreiner, W., Wollenek, G., & Mallinger, R. (1998). Outer radius-wall thickness ratio, a postmortem quantitative histology in human coronary arteries. Acta Anatomica (Basel), 163(2), 63–68.
Johnson, K., Sharma, P., & Oshinski, J. (2008). Coronary artery flow measurement using navigator echo gated phase contrast magnetic resonance velocity mapping at 3.0 T. Journal of Biomechanics, 41(3), 595–602. https://doi.org/10.1016/j.jbiomech.2007.10.010.
Zamir, M., Sinclair, P., & Wonnacott, T. H. (1992). Relation between diameter and flow in major branches of the arch of the aorta. Journal of Biomechanics, 25(11), 1303–1310. https://doi.org/10.1016/0021-9290(92)90285-9.
Changizi, M. A., & Cherniak, C. (2000). Modeling the large-scale geometry of human coronary arteries. Canadian Journal of Physiology and Pharmacology, 78(8), 603–611.
Zhao, X., Liu, Y., Li, L., Wang, W., Xie, J., & Zhao, Z. (2016). Hemodynamics of the string phenomenon in the internal thoracic artery grafted to the left anterior descending artery with moderate stenosis. Journal of Biomechanics, 49(7), 983–991. https://doi.org/10.1016/j.jbiomech.2015.11.044.
Zhao, Z., Mao, B., Liu, Y., Yang, H., & Chen, Y. (2018). The study of the graft hemodynamics with different instant patency in coronary artery bypassing grafting. Computer Modeling in Engineering and Sciences, 116(2), 229–245. https://doi.org/10.31614/cmes.2018.04192.
Dur, O., Coskun, S. T., Coskun, K. O., Frakes, D., Kara, L. B., & Pekkan, K. (2011). Computer-aided patient-specific coronary artery graft design improvements using CFD coupled shape optimizer. Cardiovascular Engineering and Technology, 2(1), 35–47. https://doi.org/10.1007/s13239-010-0029-z.
Meirson, T., Orion, E., Di Mario, C., et al. (2015). Flow patterns in externally stented saphenous vein grafts and development of intimal hyperplasia. The Journal of Thoracic and Cardiovascular Surgery, 150(4), 871–878. https://doi.org/10.1016/j.jtcvs.2015.04.061.
Fan, T., Feng, Y., Feng, F., et al. (2017). A comparison of postoperative morphometric and hemodynamic changes between saphenous vein and left internal mammary artery grafts. Physiological Reports, 5(21), 1–12. https://doi.org/10.14814/phy2.13487.
Ballarin, F., Faggiano, E., Manzoni, A., et al. (2017). Numerical modeling of hemodynamics scenarios of patient-specific coronary artery bypass grafts. Biomechanics and Modeling in Mechanobiology, 16(4), 1373–1399.
Khan, M., Valen-Sendstad, K., & Steinman, D. (2015). Narrowing the expertise gap for predicting intracranial aneurysm hemodynamics: impact of solver numerics versus mesh and time-step resolution. AJNR. American Journal of Neuroradiology, 36, 1310–1316. https://doi.org/10.3174/ajnr.A4263.
Xiang, J., Natarajan, S., Tremmel, M., et al. (2011). Hemodynamic-morphologic discriminants for intracranial aneurysm rupture. Stroke, 42(1), 144–152. https://doi.org/10.1161/STROKEAHA.110.592923.
Khan, M. O., Arana, V. T., Rubbert, C., et al. (2020). Association between aneurysm hemodynamics and wall enhancement on 3D vessel wall MRI. Journal of Neurosurgery, 1–11. https://doi.org/10.3171/2019.10.JNS191251.
Koszegi, Z., Kiss, B., Sipos, D., et al. (2018). Comparing the shear stress in degenerated and intact venous grafts from the same patients. European Heart Journal, 39(Suppl_1), ehy565–eP2695.
Akasaka, T., Yoshikawa, J., Yoshida, K., et al. (1995). Flow capacity of internal mammary artery grafts: Early restriction and later improvement assessed by Doppler guide wire. Comparison with saphenous vein grafts. Journal of the American College of Cardiology, 25(3), 640–647. https://doi.org/10.1016/0735-1097(94)00448-Y.
Shimizu, T., Ito, S., Kikuchi, Y., et al. (2004). Arterial conduit shear stress following bypass grafting for intermediate coronary artery stenosis: a comparative study with saphenous vein grafts. European Journal of Cardio-Thoracic Surgery, 25(4), 578–584. https://doi.org/10.1016/j.ejcts.2003.12.039.
Ramachandra, A., Kahn, A., & Marsden, A. (2016). Patient-specific simulations reveal significant differences in mechanical stimuli in venous and arterial coronary grafts. Journal of Cardiovascular Translational Research, 9(4), 279–290. https://doi.org/10.1007/s12265-016-9706-0.
Ku, D., Giddens, D., Zarins, C., & Glagov, S. (1985). Pulsatile flow and atherosclerosis in the human carotid bifurcation. Positive correlation between plaque location and low oscillating shear stress. Arteriosclerosis., 5(3), 293–302. https://doi.org/10.1161/01.ATV.5.3.293.
Hozumi, T., Yoshikawa, J., Yoshida, K., et al. (1996). Use of intravascular ultrasound for in vivo assessment of changes in intimal thickness of angiographically normal saphenous vein grafts one year after aortocoronary bypass surgery. Heart., 76(4), 317–320. https://doi.org/10.1136/hrt.76.4.317.
Motwani, J., & Topol, E. (1998). Aortocoronary saphenous vein graft disease. Pathogenesis, predisposition, and prevention. Circulation., 97(9), 916–931. https://doi.org/10.4324/9781315731964-2.
Khan M, Valen-Sendstad K, Steinman D. Direct numerical simulation of laminar-turbulent transition in a non-axisymmetric stenosis model for Newtonian vs. shear-thinning non-Newtonian rheologies. Flow Turbul Combust. 2018.
Chatzizisis, Y. S., Jonas, M., Coskun, A. U., et al. (2008). Prediction of the localization of high-risk coronary atherosclerotic plaques on the basis of low endothelial shear stress: an intravascular ultrasound and histopathology natural history study. Circulation., 117(8), 993–1002. https://doi.org/10.1161/CIRCULATIONAHA.107.695254.
Ramachandra, A. B., Humphrey, J. D., & Marsden, A. L. (2017). Gradual loading ameliorates maladaptation in computational simulations of vein graft growth and remodelling. Journal of the Royal Society Interface, 14(130), 20160995.
Shah, P. J., Gordon, I., Fuller, J., et al. (2003). Factors affecting saphenous vein graft patency: clinical and angiographic study in 1402 symptomatic patients operated on between 1977 and 1999. The Journal of Thoracic and Cardiovascular Surgery, 126(6), 1972–1977. https://doi.org/10.1016/S0022-5223(03)01276-5.
Acknowledgments
The authors wish to thank Derrick Laurel from the 3D and Quantitative Imaging Laboratory for his help in constructing models from CTA data, and Dr. Jin Long at the Quantitative Science Unit at the Stanford University School of Medicine for his help in statistical analysis.
Funding
This work was supported by NIH grant (NIH R01- RHL123689A), NSF CAREER Award OCI-1150184 to A. L. M., and a Burroughs Wellcome Fund Career Award at the Scientific Interface to A. L. M. Computational resources were provided by a grant to A. L. M (TG-CTS130034) through the Extreme Science and Engineering Discovery Environment (XSEDE). R.R.S.P. is supported by VA Merit BX004558. M. O. K. acknowledges funding support from the Natural Sciences and Engineering Research Council of Canada.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosures
None
Human Subjects/Informed Consent Statement
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5). Informed consent was obtained from all patients for being included in the study. No animal studies were carried out by the authors for this article. Patient recruitment and access to non-invasive clinical data (computer tomographic (CT) images, echocardiography data) was carried out according to protocols approved by the Stanford University Institutional Review Board.
Additional information
Editor-in-Chief Enrique Lara-Pezzi oversaw the review of this article
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Khan, M.O., Tran, J.S., Zhu, H. et al. Low Wall Shear Stress Is Associated with Saphenous Vein Graft Stenosis in Patients with Coronary Artery Bypass Grafting. J. of Cardiovasc. Trans. Res. 14, 770–781 (2021). https://doi.org/10.1007/s12265-020-09982-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-020-09982-7