Abstract
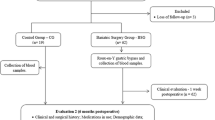
Matrix metalloproteinases (MMPs) are enzymes involved in the modulation of extracellular matrix (ECM) and adipocytes and preadipocyte differentiation. The pathophysiology of obesity has characterized by many cellular and molecular processes such as inflammatory processes, macrophage infiltration of adipose tissue, and remodeling of ECM via MMP. The purpose of the study was to determine if we can consider MMPs as a marker of effectiveness in bariatric surgery and if sulodexide administration pre- and postoperative has a benefit in terms of tissue remodeling of weight loss. An experimental study has performed using 40 obese Wistar rats (10 rats in the control group and 30 obese rats in study groups). Those in the study group were divided into three groups and underwent gastric bypass (B group), sulodexide administration (S group), gastric bypass, and sulodexide administration (BS group). Sulodexide was administered because of its antithrombotic effect in the procoagulant status of obese subjects. The pre- and postoperative weight, glucose level, cholesterol, triglycerides, MMP-2, and MMP-9 were analyzed. We compared the results to see if bariatric surgery modifies the MMPs status and if there is a correlation between the weight loss and the other parameters and also if sulodexide has any contribution to the results. The MMP-2 and MMP-9 activities were detectable, but MMP-2 was significantly higher than MMP-9. MMP-2 correlates with body weight parameters before surgery and after surgery, after significant bodyweight reduction as a result of bariatric surgery (r = 0.478, p = 0.017). There is a strong correlation between the weight loss, glucose level, and cholesterol and the values of MMP-2 (r = 0.92, p = 0.022, respectively, r = 0.759, p = 0.033). MMP-9 is correlated with weight loss and triglycerides level. But it was not as sensitive as MMP-2. Sulodexide administration in group S had a positive influence on the MMP-2 and MMP-9 compared with the values of groups B and C but without statistical significance. MMP-2 and MMP-9 are the two most important ECM enzymes involved in adipose tissue remodeling after bariatric surgery. The correlations between cholesterol, triglycerides, glucose, weight loss, excess weight, and body mass index (BMI) parameters and MMPs level demonstrate the direct relationship of these enzymes in obesity. Although we believe that more in-depth studies are required, MMPs may be considered a marker of the effectiveness of bariatric surgery.



Similar content being viewed by others
References
Sternlicht M, Werb Z (2009) How matrix metalloproteinases regulate cell behavior. Annu Rev Cell Biol 17:463–516. https://doi.org/10.1146/annurev.cellbio.17.1.463
Deng ZB, Liu YLC et al (2009) Immature myeloid cells induced by a high-fat diet contribute to liver inflammation. Hepatology 50(5):1412–1420. https://doi.org/10.1002/hep.23148
de Meijer VE, Sverdlov DY, Le HD, Popov Y, Puder M (2012) Tissue-specific differences in inflammatory infiltrate and MMP expression in adipose tissue and liver of mice with diet-induced obesity. Hepatol Res 42(6):601–610
Choe SS, Huh JY, Hwang IJ, Kim JI, Kim JB (2016) Adipose tissue remodeling: its role in energy metabolism and metabolic disorders. Front Endocrinol 7:30. https://doi.org/10.3389/fendo.2016.00030
Lee YJ, Heo YS, Park HS, Lee SH, Lee SK, Jang YJ (2014) Serum SPARC and MMP-2 and MMP-9 concentrations after metabolic surgery in obese adults. Obes Surg 24(4):604–610
Yang Z, Strickland DKBP (2001) Extracellular MMP2 levels are regulated by the low-density lipoprotein-related-scavenger receptor and thrombospondin2. J Biol Chem 276:8403–8408
Yamashita Y, Nakada S, Yoshihara T, Nara T, Furuya N, Miida T, Hattori N, Arikawa-Hirasawa E (2018) Perlecan, a heparan sulfate proteoglycan, regulates systemic metabolism with dynamic changes in adipose tissue and skeletal muscle. Sci Rep 8:7766
Mannello F, Medda V, Ligi D, Raffetto JD (2013) Glycosaminoglycan sulodexide inhibition of MMP-9 gelatinase secretion and activity: possible pharmacological role against collagen degradation in vascular chronic diseases. Curr Vasc Pharmacol 11(3):354–365
Mannello F, Raffetto JD (2011) MMP activity and glycosaminoglycans in chronic venous disease: the linkage among cell biology, pathology, and translational research. Am J Transl Res 3(2):149–158
Bonnans C, Chou J, Werb Z (2014) Remodelling the extracellular matrix in development and disease. Nat Rev Mol Cell Biol 15:786–801
Paiva KBS, Granjeiro JM (2017) Chapter six - matrix metalloproteinases in bone resorption, remodeling, and repair. In: Raouf AK (ed) Progress in molecular biology and translational science. Academic Press, Cambridge, pp 203–303
Yamashita Y, Hatano T, Ogawa T, Daida K, Motoi Y, Hattori N (2020) Steroid-responsive parkinsonism caused by cerebral amyloid angiopathy-related inflammation. Mov Disord Clin Pract 7(3):329–331
Wada H (2013) Domain shuffling and the evolution of vertebrate extracellular matrix. In: Keeley F, Mecham R (eds) Evolution of extracellular matrix. Biology of Extracellular Matrix. Springer, Berlin, Heidelberg
Chen Y, Peng W, Raffetto JD, Khalil RA (2017) Chapter Eight - Matrix Metalloproteinases in Remodeling of Lower Extremity Veins and Chronic Venous Disease. Prog Mol Biol Transl Sci 147:267–299
Hanusch-Enserer U, Zorn G, Wojta J et al (2009) Non-conventional markers of atherosclerosis before and after LGB. Eur Heart J 30(12):1516–1524. https://doi.org/10.1093/eurheartj/ehp108
Domienik-Karłowicz J, Rymarczyk Z, Dzikowska-Diduch O, Lisik W, Chmura A, Demkow U, Pruszczyk P (2015) Emerging markers of atherosclerosis before and after metabolic surgery. Obes Surg 25(3):486–493
Scholtz S, Miras AD, Chhina N, Prechtl CG, Sleeth ML, Daud NM et al (2014) Obese patients after gastric by-pass surgery have lower brain-hedonic responses to food than after gastric banding. Gut 63(6):891–902. https://doi.org/10.1136/gutjnl-2013-305008
Maquoi E, Munaut C, Colige A, Collen D, Roger LH (2002) Modulation of adipose tissue expression of murine MMP and their TIMP with obesity. Diabetes. 51(4):1093–1101
Chavey C, Mari B, Monthouel MN, Bonnafous S, Anglard P, Van Obberghen E et al (2003) MMP differentially expressed in adipose tissue during obesity and modulate adipocyte differentiation. J Biol Chem 278(14):11888–11896
Wood L, Roelofs K, Koch LG, Britton SL, Sandoval DA (2018) Vertical sleeve gastrectomy corrects metabolic perturbations in a low-exercise capacity rat model. Mol Metab 11:189–196. https://doi.org/10.1016/j.molmet.2018.02.009
Joy K. Saha, Jinqi Xia, Janet M. Grondin, Steven K. Engle, Joseph A. Jakubowski (2018) Acute hyperglycemia induced by Ketamine Xylazine anesthesia in rats: mechanisms and implications for preclinical models biotechnology discovery research, Lilly Research Laboratories, Eli Lilly and Company, Lilly Corporate Center, Indianapolis, IN 46285
Kalaivani A, Uddandrao VVS, Parim B, Ganapathy S, Nivedha PR, Kancharla SC et al (2018) Reversal of high fat diet-induced obesity through modulating lipid metabolic enzymes and inflammatory markers expressions in rats. Arch Physiol Biochem 125(3):228–234. https://doi.org/10.1080/13813455.2018.1452036
Mu S, Liu J, Guo W, Zhang S, Xiao X, Wang Z, Zhang J (2017) RYGB improves hepatic glucose metabolism involving down-regulation of protein tyrosine phosphatase 1B in obese rats. Obes Facts 10(3):191–206
Ye M, Huang R, Min Z, Zhang P, Wang T, Yu B (2017) Comparison of the effect by which gastric plication and sleeve gastrectomy procedures alter metabolic and physical parameters in an obese type 2 diabetes rodent model. Surg Obes Relat Dis 13(11):1819–1828
Haare J, Kooi ME, Teeffelen JWGE, Vink H, Slenter J, Cobelens H et al (2017) Metformin and sulodexide restore cardiac microvascular perfusion capacity in obese rats. Cardiovasc Diabetol 16:47 (2017). https://doi.org/10.1186/s12933-017-0525-7
Ribaric G, Buchwald JN, McGlennon TW (2014) Diabetes and weight in comparative studies of bariatric surgery vs. conventional therapy: a review and meta-analysis. Obes Surg 24(3):437–455
Jaoude J, Koh Y (2016) Matrix metalloproteinases in exercise and obesity. Vasc Health Risk Manag 12:287–295
Mirica RM, Ionescu M, Mirica A, Ginghina O, Iosifescu R, Rosca A, Munteanu R, Iordache N, Zagrean L (2018) Quality of life assessment after bariatric surgery—a single-center experience. Indian J Surg 80:435–441. https://doi.org/10.1007/s12262-017-1624-0
Mirica RM, Ionescu M, Mirica A, Ginghina O, Iosifescu R, Rosca A, Iordache N (2017) The important roles of matrix metalloproteinases in the pathophysiology of obesity. Rev Chim 68(7):1481
Tchernof A, Despres J-P (2013) Pathophysiology of visceral obesity: an update. Physiol Rev 93(1):359–404
Acknowledgments
This study acknowledges Mioara Paraschiv and Dr. Bogdan Marinescu from the University of Agronomic Sciences and Veterinary Medicine, Faculty of Veterinary Medicine, Bucharest, who assured the care and supervision of rats during the experiments.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study presents the written agreement of the ethics committee of the University of Medicine and Pharmacy “Carol Davila” Bucharest to complete the Ph.D. thesis.
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
All applicable institutional and/or national guidelines for the care and use of animals were followed.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mirica, R.M., Ionescu, M., Mirica, A. et al. Matrix Metalloproteinases in Obesity After Gastric Bypass Surgery—an Experimental Study. Indian J Surg 86 (Suppl 3), 550–556 (2024). https://doi.org/10.1007/s12262-020-02462-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-020-02462-x