Abstract
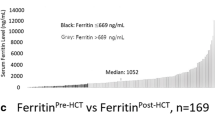
Serum ferritin, a marker of systemic iron status, is considered a prognostic factor for patients with myelodysplastic syndromes (MDS), despite the lack of supporting evidence. We investigated the association between serum ferritin levels at diagnosis and the prognoses of Japanese MDS patients with bone marrow blasts < 5% and peripheral blood blasts < 2%. Three hundred and ninety patients with cytopenia were registered prospectively in the multicenter database, among whom 107 patients with MDS (72 males and 35 females, with a median age of 70 years) met the eligibility criteria. The median serum ferritin level at diagnosis was 204 ng/mL; we divided the cohort into low (n = 56) and high (n = 51) ferritin groups using a cutoff of 210 ng/mL. Kaplan–Meier analyses revealed that the 3-year overall survival (OS) of the high ferritin group was significantly shorter than that of the low ferritin group (66% and 79%, respectively). The cumulative incidences of leukemic progression were similar between the groups. On multivariate analysis, age, blast percentage, cytogenetic abnormalities, and serum ferritin levels at diagnosis were independently associated with OS in our patients. Thus, modest elevations of ferritin levels at diagnosis may influence the prognoses of patients with MDS who have low blast counts.


Similar content being viewed by others
References
Ades L, Itzykson R, Fenaux P. Myelodysplastic syndromes. Lancet. 2014;383:2239–52.
Greenberg P, Cox C, LeBeau MM, Fenaux P, Morel P, Sanz G, et al. International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood. 1997;89:2079–88.
Balduini CL, Guarnone R, Pecci A, Centenara E, Ascari E. International prognostic scoring system and other prognostic systems for myelodysplastic syndromes. Blood. 1997;90:4232–4.
Malcovati L, Germing U, Kuendgen A, Della Porta MG, Pascutto C, Invernizzi R, et al. Time-dependent prognostic scoring system for predicting survival and leukemic evolution in myelodysplastic syndromes. J Clin Oncol. 2007;25:3503–10.
Kantarjian H, O’Brien S, Ravandi F, Cortes J, Shan J, Bennett JM, et al. Proposal for a new risk model in myelodysplastic syndrome that accounts for events not considered in the original International Prognostic Scoring System. Cancer. 2008;113:1351–61.
Greenberg PL, Tuechler H, Schanz J, Sanz G, Garcia-Manero G, Sole F, et al. Revised international prognostic scoring system for myelodysplastic syndromes. Blood. 2012;120:2454–65.
Cohen LA, Gutierrez L, Weiss A, Leichtmann-Bardoogo Y, Dl Zhang, Crooks DR, et al. Serum ferritin is derived primarily from macrophages through a nonclassical secretory pathway. Blood. 2010;116:1574–84
Pileggi C, Di Sanzo M, Mascaro V, Marafioti MG, Costanzo FS, Pavia M. Role of serum ferritin level on overall survival in patients with myelodysplastic syndromes: results of a meta-analysis of observational studies. PLoS ONE. 2017;12:e0179016.
Lim ZY, Fiaccadori V, Gandhi S, Hayden J, Kenyon M, Ireland R, et al. Impact of pre-transplant serum ferritin on outcomes of patients with myelodysplastic syndromes or secondary acute myeloid leukaemia receiving reduced intensity conditioning allogeneic haematopoietic stem cell transplantation. Leuk Res. 2010;34:723–7.
Armand P, Kim HT, Cutler CS, Ho VT, Koreth J, Alyea EP, et al. Prognostic impact of elevated pretransplantation serum ferritin in patients undergoing myeloablative stem cell transplantation. Blood. 2007;109:4586–8.
Sakamoto S, Kawabata H, Kanda J, Uchiyama T, Mizumoto C, Kondo T, et al. Differing impacts of pretransplant serum ferritin and C-reactive protein levels on the incidence of chronic graft-versus-host disease after allogeneic hematopoietic stem cell transplantation. Int J Hematol. 2013;97:109–16.
Kikuchi S, Kobune M, Iyama S, Sato T, Murase K, Kawano Y, et al. Prognostic significance of serum ferritin level at diagnosis in myelodysplastic syndrome. Int J Hematol. 2012;95:527–34.
Laribi K, Bolle D, Alani M, Ghnaya H, Le Bourdelles S, Besancon A, et al. Prognostic impact of elevated pretreatment serum ferritin in patients with high-risk MDS treated with azacitidine. Exp Hematol. 2018;65:34–7.
Sotirova T, Stojanovic A, Genadieva-Stavric S, Krstevska S, Spasovski D, Balkanov T. Influence of prognostic factors on overall survival in myelodysplastic syndromes. Mater Sociomed. 2014;26:292–6.
Kerkhofs H, Hermans J, Haak HL, Leeksma CH. Utility of the FAB classification for myelodysplastic syndromes: investigation of prognostic factors in 237 cases. Br J Haematol. 1987;65:73–81.
Kawabata H, Tohyama K, Matsuda A, Araseki K, Hata T, Suzuki T, et al. Validation of the revised International Prognostic Scoring System in patients with myelodysplastic syndrome in Japan: results from a prospective multicenter registry. Int J Hematol. 2017;106:375–84.
Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton DA, Gralnick HR, et al. Proposals for the classification of the myelodysplastic syndromes. Br J Haematol. 1982;51:189–99.
Goasguen JE, Bennett JM, Bain BJ, Brunning R, Vallespi MT, Tomonaga M, et al. Proposal for refining the definition of dysgranulopoiesis in acute myeloid leukemia and myelodysplastic syndromes. Leuk Res. 2014;38:447–53.
Mufti GJ, Bennett JM, Goasguen J, Bain BJ, Baumann I, Brunning R, et al. Diagnosis and classification of myelodysplastic syndrome: International Working Group on Morphology of myelodysplastic syndrome (IWGM-MDS) consensus proposals for the definition and enumeration of myeloblasts and ring sideroblasts. Haematologica. 2008;93:1712–7.
Gray RJ. A class of k-sample tests for comparing the cumulative incidence of a competing risk. Ann Stat. 1988;16:1141–54.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, et al. editors. WHO classification of tumours of haematopoietic and lymphoid tissues. Lyon: International Agency for Research on Cancer (IARC); 2017.
Shenoy N, Vallumsetla N, Rachmilewitz E, Verma A, Ginzburg Y. Impact of iron overload and potential benefit from iron chelation in low-risk myelodysplastic syndrome. Blood. 2014;124:873–81.
Srai SK, Bomford A, McArdle HJ. Iron transport across cell membranes: molecular understanding of duodenal and placental iron uptake. Best Pract Res Clin Haematol. 2002;15:243–59.
Cui R, Gale RP, Zhu G, Xu Z, Qin T, Zhang Y, et al. Serum iron metabolism and erythropoiesis in patients with myelodysplastic syndrome not receiving RBC transfusions. Leuk Res. 2014;38:545–50.
Camaschella C, Nai A. Ineffective erythropoiesis and regulation of iron status in iron loading anaemias. Br J Haematol. 2016;172:512–23.
Gattermann N. Iron overload in myelodysplastic syndromes (MDS). Int J Hematol. 2018;107:55–63.
Kikuchi S, Kobune M, Iyama S, Sato T, Murase K, Kawano Y, et al. Improvement of iron-mediated oxidative DNA damage in patients with transfusion-dependent myelodysplastic syndrome by treatment with deferasirox. Free Radic Biol Med. 2012;53:643–8.
Moukalled NM, El Rassi FA, Temraz SN, Taher AT. Iron overload in patients with myelodysplastic syndromes: an updated overview. Cancer. 2018;124:3979–89.
Taoka K, Kumano K, Nakamura F, Hosoi M, Goyama S, Imai Y, et al. The effect of iron overload and chelation on erythroid differentiation. Int J Hematol. 2012;95:149–59.
Jin X, He X, Cao X, Xu P, Xing Y, Sui S, et al. Iron overload impairs normal hematopoietic stem and progenitor cells through reactive oxygen species and shortens survival in myelodysplastic syndrome mice. Haematologica. 2018;103:1627–34.
Zheng Q, Zhao Y, Guo J, Zhao S, Fei C, Xiao C, et al. Iron overload promotes mitochondrial fragmentation in mesenchymal stromal cells from myelodysplastic syndrome patients through activation of the AMPK/MFF/Drp1 pathway. Cell Death Dis. 2018;9:515.
Brittenham GM, Griffith PM, Nienhuis AW, McLaren CE, Young NS, Tucker EE, et al. Efficacy of deferoxamine in preventing complications of iron overload in patients with thalassemia major. N Engl J Med. 1994;331:567–73.
McLaren GD, Gordeuk VR. Hereditary hemochromatosis: insights from the Hemochromatosis and Iron Overload Screening (HEIRS) Study. Hematol Am Soc Hematol Educ Program. 2009;2009:195–206.
Nielsen P, Gunther U, Durken M, Fischer R, Dullmann J. Serum ferritin iron in iron overload and liver damage: correlation to body iron stores and diagnostic relevance. J Lab Clin Med. 2000;135:413–8.
Garcia-Manero G, Shan J, Faderl S, Cortes J, Ravandi F, Borthakur G, et al. A prognostic score for patients with lower risk myelodysplastic syndrome. Leukemia. 2008;22:538–43.
Li B, Xu Z, Gale RP, Qin T, Zhang Y, Xiao Z. Serum ferritin is an independent prognostic factor in Chinese with myelodysplastic syndromes classified as IPSS Intermediate-1. Acta Haematol. 2013;129:243–50.
Park S, Sapena R, Kelaidi C, Vassilieff D, Bordessoule D, Stamatoullas A, et al. Ferritin level at diagnosis is not correlated with poorer survival in non RBC transfusion dependent lower risk de novo MDS. Leuk Res. 2011;35:1530–3.
Park S, Hamel JF, Toma A, Kelaidi C, Thepot S, Campelo MD, et al. Outcome of lower-risk patients with myelodysplastic syndromes without 5q deletion after failure of erythropoiesis-stimulating agents. J Clin Oncol. 2017;35:1591–7.
Leitch HA, Parmar A, Wells RA, Chodirker L, Zhu N, Nevill TJ, et al. Overall survival in lower IPSS risk MDS by receipt of iron chelation therapy, adjusting for patient-related factors and measuring from time of first red blood cell transfusion dependence: an MDS-CAN analysis. Br J Haematol. 2017;179:83–97.
Zipperer E, Post JG, Herkert M, Kundgen A, Fox F, Haas R, et al. Serum hepcidin measured with an improved ELISA correlates with parameters of iron metabolism in patients with myelodysplastic syndrome. Ann Hematol. 2013;92:1617–23.
Oguma S, Yoshida Y, Uchino H, Maekawa T, Nomura T, Mizoguchi H. Clinical characteristics of Japanese patients with primary myelodysplastic syndromes: a co-operative study based on 838 cases. Anemia Study Group of the Ministry of Health and Welfare. Leuk Res. 1995;19:219–25.
Germing U, Strupp C, Kuendgen A, Isa S, Knipp S, Hildebrandt B, et al. Prospective validation of the WHO proposals for the classification of myelodysplastic syndromes. Haematologica. 2006;91:1596–604.
Komrokji RS, Corrales-Yepez M, Kharfan-Dabaja MA, Al Ali NH, Padron E, Rollison DE, et al. Hypoalbuminemia is an independent prognostic factor for overall survival in myelodysplastic syndromes. Am J Hematol. 2012;87:1006–9.
Chee CE, Steensma DP, Wu W, Hanson CA, Tefferi A. Neither serum ferritin nor the number of red blood cell transfusions affect overall survival in refractory anemia with ringed sideroblasts. Am J Hematol. 2008;83:611–3.
Roudot-Thoraval F, Halphen M, Larde D, Galliot M, Rymer JC, Galacteros F, et al. Evaluation of liver iron content by computed tomography: its value in the follow-up of treatment in patients with idiopathic hemochromatosis. Hepatology. 1983;3:974–9.
Roy NB, Myerson S, Schuh AH, Bignell P, Patel R, Wainscoat JS, et al. Cardiac iron overload in transfusion-dependent patients with myelodysplastic syndromes. Br J Haematol. 2011;154:521–4.
Feelders RA, Vreugdenhil G, Eggermont AM, Kuiper-Kramer PA, van Eijk HG, Swaak AJ. Regulation of iron metabolism in the acute-phase response: interferon gamma and tumour necrosis factor alpha induce hypoferraemia, ferritin production and a decrease in circulating transferrin receptors in cancer patients. Eur J Clin Invest. 1998;28:520–7.
Park S, Kosmider O, Maloisel F, Drenou B, Chapuis N, Lefebvre T, et al. Dyserythropoiesis evaluated by the RED score and hepcidin:ferritin ratio predicts response to erythropoietin in lower-risk myelodysplastic syndromes. Haematologica. 2019;104:497–504.
Cazzola M, Della Porta MG, Malcovati L. Clinical relevance of anemia and transfusion iron overload in myelodysplastic syndromes. Hematol Am Soc Hematol Educ Program. 2008;2008:166–75.
Du Y, Long Z, Chen M, Han B, Hou B, Feng F. Observational monitoring of patients with aplastic anemia and low/intermediate-1 risk of myelodysplastic syndromes complicated with iron overload. Acta Haematol. 2017;138:119–28.
Acknowledgements
The authors thank the patients, their families, all the investigators including Drs. Yukiharu Nakabo (The Center for Hematological Diseases, Takeda General Hospital), Takahiko Utsumi (Department of Hematology and Oncology, Shiga General Hospital), Tatsuo Ichinohe (Department of Hematology and Oncology, Research Institute for Radiation Biology and Medicine, Hiroshima University), Hirohiko Shibayama (Department of Hematology and Oncology, Osaka University Graduate School of Medicine), Yasuyoshi Morita (Division of Hematology and Rheumatology, Department of Internal Medicine, Kindai University Faculty of Medicine), Masayuki Shiseki (Department of Hematology, Tokyo Women’s Medical University), Masayoshi Kobune (Department of Hematology, Sapporo Medical University School of Medicine), Naoshi Obara (Department of Hematology, Graduate School of Comprehensive Human Sciences, Tsukuba University), Wataru Takahashi (Department of Hematology and Oncology, Dokkyo Medical University Hospital), and nurses in the participating institutions of this study. The authors also thank Dr. Keiya Ozawa (Institute of Medical Science, the University of Tokyo) for his mentorship; and Drs. Mizuki Watanabe, Kazue Miyamoto-Arimoto, and Tasuki Uchiyama, and Ms. Tomoko Okuda and Yukiko Takada (Department of Hematology and Oncology, Kyoto University) for their technical assistance with the construction of the database.
Funding
This work was partially supported by the Research Program of Intractable Disease provided by the Ministry of Health, Labor, and Welfare (MHLW) of Japan (H20-Nanchi-Ippan-001, H23-Nanchi-Ippan-001, H26-Nanchi-Ippan-062, H27-Nanchi-Ippan-016, H29-Nanchi-Ippan-026).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
Dr. Kawabata reports personal fees from Nippon Shinyaku Co., Ltd. outside the submitted work. Dr. Tohyama reports personal fees from Celgene Corporation and SymBio Pharmaceuticals Ltd. outside the submitted work. Dr. Matsuda reports personal fees from Kyowa Hakko Kirin Co., Ltd., Nippon Shinyaku Co., Ltd., GlaxoSmithKline K. K., Celgene Corporation, Alexion Pharmaceuticals, Inc., Sanofi K. K., Beckman Coulter K. K., and Shire Japan K.K.; grants and personal fees from Sumitomo Dainippon Pharma Co., Ltd., Chugai Pharmaceutical Co., Ltd., and Novartis Pharma K. K.; and grants from Astellas Pharm Inc., Asahi Kasei Pharma Co., Ltd., Eisai Co., Ltd., Otsuka Pharmaceutical Co., Ltd., Boehringer Ingelheim Japan Inc., MSD K. K., Daiichi Sankyo Co., Ltd., Abbvie GK, and HUYA Bioscience International outside the submitted work. Dr. Suzuki reports personal fees from Novartis Pharma K.K., Nippon Shinyaku Co., Ltd., Celgene Corporation, and Kyowa Hakko Kirin Co., Ltd.; grants from Astellas Pharma Inc. outside the submitted work. Mr. Shimbo reports personal fees from Celgene Corporation, and Bristol-Myers Squibb outside the submitted work. Dr. Chiba reports grants from Kyowa Hakko Kirin Co., Ltd., Bristol-Myers Squibb, and Astellas Pharma Inc. outside the submitted work. Dr. Miyazaki reports personal fees from Novartis Pharma K.K., Dainippon Sumitomo Pharma Co., Ltd., Celgene Corporation, and SymBio Pharmaceuticals Ltd.; personal fees and grants from Kyowa Hakko Kirin Co., Ltd.; grants from Chugai Pharmaceutical Co., Ltd., Takeda Pharmaceutical Co., Ltd., and Pfizer Seiyaku K.K. outside the submitted work. Dr. Mitani reports grants and personal fees from Kyowa-Hakko Kirin Co., Ltd.; and grants from Chugai Pharmaceutical Co., Ltd., Novartis Pharma K.K., Teijin Pharma Ltd., Japan Blood Products Organization, Ono Pharmaceutical Co., Ltd., Takeda Pharmaceutical Co., Ltd., and Toyama Chemical Co., Ltd. outside the submitted work. Dr. Kurokawa reports personal fees from Shionogi & Co., Ltd. and Celgene Corporation; grants from Kyowa Hakko Kirin Co., Ltd., Nippon Shinyaku Co., Ltd., Astellas Pharma Inc., Ono Pharmaceutical Co., Ltd., Takeda Pharmaceutical Co., Ltd., Novartis Pharma K.K., Bristol-Myers Squibb, and Pfizer Seiyaku K.K. outside the submitted work. Dr. Takaori-Kondo reports personal fees from Yanssen Pharmaceutical K.K., Novartis Pharma K.K., and Bristol-Myers Squibb; personal fees and grants from Pfizer Seiyaku K.K. and Celgene Corporation; and grants from Chugai Pharmaceutical Co., Ltd., Takeda Pharmaceutical Co., Ltd., Kyowa Hakko Kirin Co., Ltd., Astellas Pharma Inc., Japan Blood Products Organization, Eisai Co., Ltd., Shionogi & Co., Ltd., Mochida Pharmaceutical Co., Ltd., and Otsuka Pharmaceutical Co., Ltd. outside the submitted work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Kawabata, H., Usuki, K., Shindo-Ueda, M. et al. Serum ferritin levels at diagnosis predict prognosis in patients with low blast count myelodysplastic syndromes. Int J Hematol 110, 533–542 (2019). https://doi.org/10.1007/s12185-019-02710-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-019-02710-1