Abstract
Purpose of Review
The aim of this scoping review is to identify and summarize findings published in the literature over the past 5 years related to methods for assessment of bone loss in anterior shoulder instability.
Recent Findings
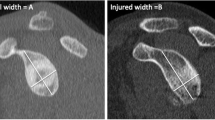
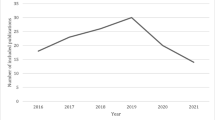
Of the 113 clinical studies included in this review, 76 reported a cutoff for glenoid bone loss when determining the patients indicated for one of the many stabilization procedures investigated. Bone loss on the glenoid side was evaluated most commonly with three-dimensional computed tomography (3D CT), and either linear or surface area–based methods were employed with the use of a best-fit circle. When combined with plain CT, the two methods comprise up to 70% of the reported measurement techniques for glenoid bone loss (79 of 113 studies). On the humeral side, Hill-Sachs lesions were assessed more heterogeneously, though plain CT or 3D CT remained the methods of choice in the majority of studies (43 of 68, 63.2%). Lastly, the glenoid track was assessed by 27 of 113 studies (23.9%), again most commonly with 3D CT (13 studies) and plain CT (seven studies).
Summary
The assessment of glenoid and humeral bone loss is essential to treatment decisions for patient with recurrent anterior shoulder instability. Glenoid bone loss is most commonly assessed using cross-sectional imaging, most often 3D CT, and some variation of a best-fit circle applied to the inferior portion of the glenoid. Hill-Sachs lesion assessment was also commonly done using three-dimensional imaging; however, there was more variability in assessment methods across studies and there is an obvious need to unify the approach to humeral bone loss assessment for the purposes of improving treatment decisions and to better assess on-track and off-track lesions.


Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Cutts S, Prempeh M, Drew S. Anterior shoulder disloctation. Ann R Coll Surg Engl. 2009;91:2–7.
Zacchilli MA, Owens BD. Epidemiology of shoulder dislocations presenting to emergency departments in the United States. J Bone Jt Surg - Ser A. 2010;92:542–9.
Pougès C, Hardy A, Vervoort T, Amouyel T, Duriez P, Lalanne C, Szymanski C, Deken V, Chantelot C, Upex P, Maynou C. Arthroscopic Bankart repair versus immobilization for first episode of anterior shoulder dislocation before the age of 25: a randomized controlled trial. Am J Sports Med. 2021;49:1166–74.
Leroux T, Wasserstein D, Veillette C, Khoshbin A, Henry P, Chahal J, Austin P, Mahomed N, Ogilvie-Harris D (2014) Epidemiology of primary anterior shoulder dislocation requiring closed reduction in Ontario, Canada. Am J Sports Med 42:442–450. Describes the epidemiology of anterior shoulder instability in a Canadian population.
Vermeiren J, Handelberg F, Casteleyn PP, Opdecam P. The rate of recurrence of traumatic anterior dislocation of the shoulder - a study of 154 cases and a review of the literature. Int Orthop. 1993;17:337–41.
Larrain MV, Botto GJ, Montenegro HJ, Mauas DM. Arthroscopic repair of acute traumatic anterior shoulder dislocation in young athletes. Arthroscopy. 2001;17:373–7.
Brophy RH, Marx RG. Osteoarthritis following shoulder instability. Clin Sports Med. 2005;24:47–56.
Ode GE, Ling D, Finocchiaro A, Lai EY, Taylor SA, Dines J, Dines D, Warren R, Gulotta L. Clinical characteristics and patient-reported outcomes of total shoulder arthroplasty after anterior stabilization: a retrospective matched control study. J Shoulder Elb Surg. 2020;29:S59–66.
Calandra JJ, Baker CL, Uribe J. The incidence of Hill-Sachs lesions in initial anterior shoulder dislocations. Arthrosc J Arthrosc Relat Surg. 1989;5:254–7.
Hill HA, Sachs MD (1940) The grooved defect of the humeral head. Radiology 35:690–700. Initial descripton of the Hill-Sachs lesion.
Spatschil A, Landsiedl F, Anderl W, Imhoff A, Seiler H, Vassilev I, Klein W, Boszotta H, Hoffmann F, Rupp S. Posttraumatic anterior-inferior instability of the shoulder: arthroscopic findings and clinical correlations. Arch Orthop Trauma Surg. 2006;126:217–22.
Edwards TB, Boulahia A, Walch G. Radiographic analysis of bone defects in chronic anterior shoulder instability. Arthrosc - J Arthrosc Relat Surg. 2003;19:732–9.
Čičak N, Bilić R, Delimar D. Hill-Sachs lesion in recurrent shoulder dislocation: sonographic detection. J Ultrasound Med. 1998;17:557–60.
Nakagawa S, Ozaki R, Take Y, Iuchi R, Mae T. Relationship between glenoid defects and Hill-Sachs lesions in shoulders with traumatic anterior instability. Am J Sports Med. 2015;43:2763–73.
Yiannakopoulos CK, Mataragas E, Antonogiannakis E. A comparison of the spectrum of intra-articular lesions in acute and chronic anterior shoulder instability. Arthrosc - J Arthrosc Relat Surg. 2007;23:985–90.
Balg F, Boileau P. The instability severity index score: a simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Jt Surg - Ser B. 2007;89:1470–7.
Lynch JR, Clinton JM, Dewing CB, Warme WJ, Matsen FA. Treatment of osseous defects associated with anterior shoulder instability. J Shoulder Elb Surg. 2009;18:317–28.
Lo IKY, Parten PM, Burkhart SS (2004) The inverted pear glenoid: an indicator of significant glenoid bone loss. Arthrosc - J Arthrosc Relat Surg 20:169–174. Describes an important concept in the recognition of significant glenoid bone loss.
Itoi E, Lee SB, Berglund LJ, Berge LL, An KN. The effect of a glenoid defect on anteroinferior stability of the shoulder after Bankart repair: a cadaveric study. J Bone Jt Surg - Ser A. 2000;82:35–46.
Yamamoto N, Itoi E, Abe H, Kikuchi K, Seki N, Minagawa H, Tuoheti Y. Effect of an anterior glenoid defect on anterior shoulder stability: a cadaveric study. Am J Sports Med. 2009;37:949–54.
Chen AL, Hunt SA, Hawkins RJ, Zuckerman JD. Management of bone loss associated with recurrent anterior glenohumeral instability. Am J Sports Med. 2005;33:912–25.
Shin SJ, Koh YW, Bui C, Jeong WK, Akeda M, Cho NS, McGarry MH, Lee TQ. What is the critical value of glenoid bone loss at which soft tissue bankart repair does not restore glenohumeral translation, restricts range of motion, and leads to abnormal humeral head position? Am J Sports Med. 2016;44:2784–91.
Shin SJ, Kim RG, Jeon YS, Kwon TH (2017) Critical value of anterior glenoid bone loss that leads to recurrent glenohumeral instability after arthroscopic bankart repair. Am J Sports Med 45:1975–1981. Reports 17.3% as a new cutoff for critical bone loss, lending support to the idea of subcritical bone loss amounts.
Shaha JS, Cook JB, Song DJ, Rowles DJ, Bottoni CR, Shaha SH, Tokish JM. “Subcritical” glenoid bone loss increases redislocation rates in primary arthroscopic bankart repair. Orthop J Sport Med. 2014. https://doi.org/10.1177/2325967114S00025.
Shaha JS, Cook JB, Song DJ, Rowles DJ, Bottoni CR, Shaha SH, Tokish JM. Redefining “critical” bone loss in shoulder instability. Am J Sports Med. 2015;43:1719–25.
Dickens JF, Owens BD, Cameron KL, DeBerardino TM, Masini BD, Peck KY, Svoboda SJ (2017) The effect of subcritical bone loss and exposure on recurrent instability after arthroscopic bankart repair in intercollegiate American football. Am J Sports Med 45:1769–1775. Reports 13.5% as a new cutoff for significant bone loss in collegiate football players, lending support to the idea of subcritical bone loss amounts.
Burkhart SS, De Beer JF (2000) Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: Significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 16:677–694. Description of bipolar lesions and their significance.
Di Giacomo G, Itoi E, Burkhart SS (2014) Evolving concept of bipolar bone loss and the Hill-Sachs lesion: from “engaging/non-engaging” lesion to “on-track/off-track” lesion. Arthrosc - J Arthrosc Relat Surg 30:90–98. Describes the assessment of bipolar lesions as on-track or off-track.
Arciero RA, Parrino A, Bernhardson AS, Diaz-Doran V, Obopilwe E, Cote MP, Golijanin P, Mazzocca AD, Provencher MT. The effect of a combined glenoid and Hill-Sachs defect on glenohumeral stability: a biomechanical cadaveric study using 3-dimensional modeling of 142 patients. Am J Sports Med. 2015;43:1422–9.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol Theory Pract. 2005;8:19–32.
Sugaya H, Moriishi J, Dohi M, Kon Y, Tsuchiya A (2003) Glenoid rim morphology in recurrent anterior glenohumeral instability. J Bone Jt Surg - Ser A 85:878–884. First description of one of the most common methods for assessing glenoid bone loss.
Baudi P, Righi P, Bolognesi D, Rivetta S, Rossi Urtoler E, Guicciardi N, Carrara M. How to identify and calculate glenoid bone deficit. Chir Organi Mov. 2005;90:145–52.
Hardy P, Lopes R, Bauer T, Conso C, Gaudin P, Sanghavi S. New quantitative measurement of the Hill-Sachs lesion: a prognostic factor for clinical results of arthroscopic glenohumeral stabilization. Eur J Orthop Surg Traumatol. 2012;22:541–7.
Nobuhara K. The shoulder: its function and clinical aspects. 2003. https://doi.org/10.1142/5412.
Yamamoto N, Itoi E, Abe H, Minagawa H, Seki N, Shimada Y, Okada K. Contact between the glenoid and the humeral head in abduction, external rotation, and horizontal extension: a new concept of glenoid track. J Shoulder Elb Surg. 2007;16:649–56.
Bakshi NK, Cibulas GA, Sekiya JK, Bedi A (2018) A clinical comparison of linear- and surface area–based methods of measuring glenoid bone loss. Am J Sports Med 46:2472–2477. Compares surface area-based and linear measurement techniques.
Frank RM, Golijanin P, Vopat BG, Gross DJ, Chauhan V, Romeo AA, Provencher MT. Impact of sagittal rotation on axial glenoid width measurement in the setting of glenoid bone loss. Am J Orthop (Belle Mead NJ). 2018;47. https://doi.org/10.12788/ajo.2018.0041.
Lacheta L, Herbst E, Voss A, Braun S, Jungmann P, Millett PJ, Imhoff A, Martetschläger F. Insufficient consensus regarding circle size and bone loss width using the ratio—“best fit circle”—method even with three-dimensional computed tomography. Knee Surgery, Sport Traumatol Arthrosc. 2019;27:3222–9.
Rossi LA, Frank RM, Wilke D, et al (2021) Evaluation and management of glenohumeral instability with associated bone loss: an expert consensus statement using the modified delphi technique. Arthrosc - J Arthrosc Relat Surg 37:1719–1728. Expert consensus on evaluating bone loss in shoulder instability.
Milano G, Saccomanno MF, Magarelli N, Bonomo L. Analysis of agreement between computed tomography measurements of glenoid bone defects in anterior shoulder instability with and without comparison with the contralateral shoulder. Am J Sports Med. 2015;43:2918–26.
Lansdown DA, Cvetanovich GL, Verma NN, Cole BJ, Bach BR, Nicholson G, Romeo A, Dawe R, Yanke AB. Automated 3-dimensional magnetic resonance imaging allows for accurate evaluation of glenoid bone loss compared with 3-dimensional computed tomography. Arthrosc - J Arthrosc Relat Surg. 2019;35:734–40.
Assunção JH, Gracitelli MEC, Borgo GD, Malavolta EA, Bordalo-Rodrigues M, Ferreira Neto AA. Tomographic evaluation of Hill-Sachs lesions: is there a correlation between different methods of measurement? Acta radiol. 2017;58:77–83.
Schneider AK, Hoy GA, Ek ET, Rotstein AH, Tate J, Taylor DMD, Evans MC. Interobserver and intraobserver variability of glenoid track measurements. J Shoulder Elb Surg. 2017;26:573–9.
Gowd AK, Liu JN, Cabarcas BC, Garcia GH, Cvetanovich GL, Provencher MT, Verma NN. Management of recurrent anterior shoulder instability with bipolar bone loss: a systematic review to assess critical bone loss amounts. Am J Sports Med. 2019;47:2484–93.
Gyftopoulos S, Beltran LS, Bookman J, Rokito A (2015) MRI evaluation of bipolar bone loss using the on-track off-track method: a feasibility study. Am J Roentgenol 205:848–852. MRI validation of the on-track/off-track assessment.
Di Giacomo G, De Gasperis N. Measuring bone loss in the unstable shoulder: understanding and applying the track concept. Sports Med Arthrosc. 2020;28:153–8.
Boileau P, Villalba M, Héry JY, Balg F, Ahrens P, Neyton L. Risk factors for recurrence of shoulder instability after arthroscopic bankart repair. J Bone Jt Surg - Ser A. 2006;88:1755–63.
Cavalier M, Johnston TR, Tran L, Gauci MO, Boileau P. Glenoid erosion is a risk factor for recurrent instability after Hill-Sachs remplissage. Bone Jt J. 2021;103(B):718–24.
Yang JS, Mehran N, Mazzocca AD, Pearl ML, Chen VW, Arciero RA. Remplissage versus modified Latarjet for off-track Hill-Sachs lesions with subcritical glenoid bone loss. Am J Sports Med. 2018;46:1885–91.
Kho J, Kholinne E, Lim S, Hong H, Kwak JM, Sun Y, Koh KH, Jeon IH. Arthroscopic bare spot method underestimates true bone defect in bony Bankart lesion. Arch Orthop Trauma Surg. 2019;139:1269–75.
Ramos MRF, San Junior YAC, Alves LHP, Cruz FC, Mansur H. Is the bare spot reliable for the bone loss measurement? Shoulder Elb. 2019;11:106–12.
Khan M, Bedi A, Degen R, Warner J, Bhandari M, Khan M (2022) A pilot multicenter randomized controlled trial comparing Bankart repair and remplissage with the Latarjet procedure in patients with subcritical bone loss (STABLE): study protocol. Pilot Feasibility Stud 8:1–9. Protocol for ongoing RCT comparing remplissage and Latarjet for patients with subcritical bone loss.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no existing conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Outcomes Research in Orthopedics
Supplementary information
Appendix Table 1
(DOCX 45.9 kb)
Appendix Fig. 3
(DOCX 142 kb)
Rights and permissions
About this article
Cite this article
Gouveia, K., Rizvi, S.H., Dagher, D. et al. Assessing Bone Loss in the Unstable Shoulder: a Scoping Review. Curr Rev Musculoskelet Med 15, 369–376 (2022). https://doi.org/10.1007/s12178-022-09773-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12178-022-09773-4