Abstract
Mammographically-detected breast arterial calcifications (BAC) are considered to be an incidental finding without clinical importance since they are not associated with increased risk of breast cancer. The goal of this article is to review existing evidence that the presence of BAC on mammography correlates with several (but not all) traditional cardiovascular disease (CVD) risk factors and with prevalent and incident CVD. Thus, BAC detected during routine mammography is a noteworthy finding that could be valuable in identifying asymptomatic women at increased future CVD risk that may be candidates for more aggressive management. In addition, there are notable differences in measures of subclinical atherosclerosis burden in women (ie, coronary artery calcification) by race/ethnic background, and the same appears to be true for BAC, although data are very limited. Another noteworthy limitation of prior research on BAC is the reliance on absence vs presence of BAC; no study to date has determined gradation of BAC. Further research is thus required to elucidate the role of BAC gradation in the prediction of CVD outcomes and to determine whether adding BAC gradation to prediction models based on traditional risk factors improves classification of CVD risk.
Similar content being viewed by others
Introduction
Although the value of mammographic screening before age 50 and after age 74 has recently been called into question by the US Preventive Services Task Force [1] current clinical practice guidelines recommend annual mammographic screening of all women aged 40 years or older for early detection of breast cancer. However, important information about the presence and severity of subclinical atherosclerosis that is available in mammograms is presently ignored during mammographic assessments. Specifically, this information includes the presence of breast arterial calcification (BAC), which has been shown to be associated with risk of cardiovascular disease (CVD) morbidity, and mortality. Such information may be useful for improvement of CVD risk stratification in a similar manner that coronary artery calcification (CAC) has been shown in numerous prospective studies. Data from CARDIA [2], MESA [3], and other population-based studies indicate that the extent of CAC in women differs importantly by ethnic background, and the same appears to be true for calcification in other vascular beds including the breast, but the data available are very limited.
The leading causes of death among women in the US are heart disease, cancer, and stroke [4]. Even though remarkable advances have been made in the field of CVD prevention, for many asymptomatic individuals the first manifestation of underlying disease is an unexpected acute myocardial infarction or sudden death [5, 6]. Furthermore, prior studies have shown that women with obstructive coronary disease have worse prognosis after acute myocardial infarction compared with men [7–11]. A widespread tool for CVD risk stratification is the Framingham risk score, which classifies patients into low (10–year CVD risk < 10 %), intermediate (10–year CVD risk 10 %–20 %) and high (10–year CVD risk > 20 %) risk groups based on traditional risk factors [12]. However, published data indicate that up to 20 % of all coronary events occur in the absence of these major risk factors and that 60 % of events are experienced by low-to-intermediate risk patients [13–15]. Therefore, there is great interest in developing new methods, including novel serum biomarkers and noninvasive imaging modalities, to better identify patients who may be appropriate candidates for more aggressive primary prevention [16, 17]. A new algorithm, the Reynolds Risk Score, has been recently developed and (internally) validated in the Women’s Health Study [18].
Several non-invasive imaging techniques have been evaluated [19–21]. While ultrasound- and MRI-based techniques rely primarily on images of abnormal vessel anatomy due to atherosclerosis, the CT-based approach is based on estimating vascular calcium deposition. Although all these imaging techniques, particularly CT, appear to predict CVD risk in multiple longitudinal cohort studies [22, 23], critical barriers for widespread use of these imaging modalities are high cost, need for specific types of equipment, and/or specially trained personnel. In addition, concerns have been raised about increased cancer risk following cardiac CT [24], although it should be pointed out that radiation concerns are mainly for higher dosage coronary CT angiography and that radiation from a mammogram vs coronary calcium scan are very similar (0.7–0.9 mSV). BAC detected by widely used mammography in women thus offer a potential new tool for detecting subclinical CVD which may add incremental prognostic value beyond the existing CVD risk classification schemes without additional radiation exposure and cost.
Mammographically-Detected Calcifications
Mammography is a proven tool for early detection of breast cancer that is associated with a decrease in mortality rates [25]. The American Cancer Society presently recommends that “all women age 40 and older should have a screening mammogram every year and should continue to do so for as long as they are in good health”. National data indicate that at least 75 % of women age 40 and over have attended a mammographic exam in the last 2 years and 50 % have had a mammogram in the past year [26]. This tallies up to 42 million women over the age of 50. Under managed care, mammography attendance is over 80 % [27]. The attendance to mammographic screening is lower among uninsured, low SES women compared with women in managed care, but mammography is the most common screening test in women, regardless of insurance status. In the 2005 National Health Interview Survey, the self-reported attendance for mammography was 66 % [28]. In the Pennsylvania Centers for Disease Control Behavioral Risk Factor Survey, 64 % of women with less than a high school education self-reported ever having a mammogram [29]. As established in legislation, Medicare and Medicaid provide conditions of coverage for both screening and diagnostic plain film and digital mammography services. Of note, up to 40 % of breast cancers detected by screening are manifested by microcalcifications as the sole mammographic lesion [30]. As a result, the modern mammographic equipment is designed specifically for the detection of microcalcifications [31]. Therefore, this routine screening tool provides a unique opportunity to detect BAC as a possible mammographic sign of atherosclerosis. BAC on the mammogram is identifiable as linear, parallel lines that resemble a railroad track (see Fig. 1).
Vascular Calcification Pathology: Medial vs Intimal
Calcification occurs at 2 anatomic sites within the vascular wall: the intima, where it is invariably associated with atherosclerosis, and the media. These different locations most likely represent 2 pathophysiologically different processes [32–34]. Intimal calcification is an active, regulated process that is similar to bone formation and involves expression of growth factors, matrix proteins, and other bone-related proteins [35], and has been associated with inflammatory cells, lipid deposits, and vascular smooth muscle cells. By contrast, medial arterial or Mönckeberg-type calcification occurs in the absence of macrophages or lipid deposits [36] and has been described in the context of aging, diabetes, end-stage renal disease, neuropathy, and a number of rare genetic syndromes [37–40]. A study of medial calcification among Pima Indians showed it to be significantly associated with type II diabetes and with increased CVD mortality [41]. Additional studies have confirmed that medial calcification is an independent predictor of CVD events in patients with diabetes or end-stage renal disease [42–44]. The proposed putative mechanism by which medial calcification may increase CVD risk is increased arterial stiffness. Consistent with this notion, elastin has been shown to have a strong affinity for calcium and it has been postulated that disruption of the elastic fibers promotes medial calcification [45]. In a pathology study, BAC were localized in the tunica media, but some arteries showed intimal thickening in some cases [46]. With conventional x-ray techniques or with modern digital mammography, it is not possible to differentiate with certainty between intimal and medial calcifications, although the appearance of medial calcifications is more fine and diffused in smaller vessels, compared with the large and discontinuous appearance of intimal calcifications in large and medium size arteries [47, 48]. BAC is mostly (but not entirely) medial, a non-obstructive condition leading to reduced arterial compliance.
Prevalence of BAC on Mammography
The prevalence of BAC in previously published studies varies from 1 % to 49 %. Such large differences may be explained by heterogeneity in the studied populations, variations in sensitivity of mammography equipment and reporting bias. Age is the most powerful factor influencing the prevalence of BAC [49, 50]. Pre-existing coronary artery disease is also related to higher prevalence of BAC [51]. Race/ethnicity is another significant factor in the prevalence of BAC. In a large cohort of women aged 32–92 years who attended routine mammography, Hispanic women had the highest prevalence (34 %), whereas Asian women had the lowest (7 %), vs 24 % in White women, and 25 % in African-American women [52].
Relation of BAC to Cardiovascular Risk Factors and Other Factors
Prior studies have reported associations of BAC presence with older age [49, 52–59], diabetes [55, 58–60], body mass index [61], hypertension [54, 61–63], albuminuria [61], triglycerides [64], homocysteine [64], and hs-CRP [64]. It has been postulated that hyperglycemia may induce medial calcium deposits by upregulating the production of osteogenic proteins such as matrix Gla protein, osteocalcin, and osteoprotegerin [65, 66]. A recent study demonstrated that BAC also correlates with the duration of diabetes [67]. Surprisingly, an inverse association between smoking and BAC has been found by several studies [55, 56, 61, 68]. Another study has also reported an association of BAC with spontaneous or artificial menopause [49]. In the European Prospective Investigation into Cancer and Nutrition Study among women aged 49–70 years, BAC was associated with greater parity and with a history of lactation [68]. The authors speculated that both pregnancy and breast feeding induce transient hypercalcemia to meet requirements for fetal growth and breast milk production [69]. Duration of lactation has been associated with lower prevalence of the metabolic syndrome in midlife, making the BAC-lactation relationship somewhat paradoxical [70]. A significant inverse association has been reported between menopausal hormonal therapy and BAC in 4 studies [55, 71–73]. These data underscore a resemblance between BAC and coronary atherosclerosis, since increased duration of hormonal therapy has been shown to be associated with lower prevalence of CAC [74]. Mild to moderate impairment of renal function has been associated with clinical CAD [75] and with coronary and peripheral atherosclerosis [76]. However, there are no studies that have examined the relationship between renal function and BAC. Although there is a growing recognition of the importance of sleep parameters in subclinical and clinical coronary disease [77–81], no study to date has examined the association of obstructive sleep apnea or sleep duration with BAC.
Recent studies indicate that vitamin D deficiency is associated with increased risk of CVD independently of established risk factors [82–84]. Vascular calcification, along with influences on blood pressure regulation, glycemic control, and inflammation has been proposed as one of the potential mechanisms behind the vitamin D-CVD relationship, yet evidence of an association between vitamin D status and vascular calcification, including BAC, is lacking. Elevated serum calcium (C) levels have been suggested to be a risk factor for atherosclerosis [85] and myocardial infarction [86]. In turn, high serum phosphorus (P), high serum C x P product, and hyperparathyroidism influence the prevalence of vascular calcification, particularly in end-stage renal disease patients [87]. However, the association between these mineral metabolism factors and BAC has never been investigated. Statins have been shown in observational studies to be associated with reduced progression of CAC [88, 89], but clinical trials addressing the question of whether statins retard CAC progression have been disappointing [90, 91]. Emerging evidence indicates that nitrogen-containing bisphosphonates exert beneficial pleiotropic effects in the CVD system including reduction of lipids [92], inflammation [93], and inhibition of vascular calcification [94].
Arterial calcification and osteoporosis commonly accompany one another in postmenopausal women. A recent study has demonstrated that BAC is associated with osteoporotic vertebral fractures in Japanese women [95]. The results suggest that BAC and osteoporotic fractures may share a common metabolic pathway in their pathogenesis. These finding are consistent with prior work demonstrating an association between reduced bone mineral density and BAC [96].
Association of BAC with Clinical and Sub-clinical CVD Outcomes
To date, 17 studies (4 prospective and 13 cross-sectional) have been published relating BAC to clinical or subclinical CVD (Table 1). The 4 cohort studies in Dutch [61, 72] and US populations [55, 97] show consistent associations of moderate strength between BAC presence and incident non-fatal and fatal CVD. Adjusted odds ratios for cross-sectional studies of the relationship between BAC presence and prevalent CHD/CVD or angiographic coronary disease are more heterogeneous, ranging from 1.0 to 8.1 [54, 98–102]. Of note, 1 study found no independent association between BAC and angiographically-defined coronary disease [54]. Recently, Abi Rafeh et al. have published a meta-analysis of previous studies evaluating BAC as a risk marker for coronary artery disease that included 927 patients. There was a 1.59 (95 % confidence interval [CI] 1–21–2.09) increased odds of angiographically defined CAD in patients with BAC seen on mammography [103••]. To date, 1 study has demonstrated significant associations of BAC presence with CAC [57], 2 with carotid intimal-media thickness (C-IMT) [63, 104•], and 1 with positive brain MRI findings [105••]. In the Maas et al. study among 499 women aged 49–70 years, BAC was associated with coronary arterial calcifications after 9 years follow-up (OR 2.1, 95 % CI 1.10–4.23 after adjustment for age at baseline duration of follow-up) [57]. In the Sedighi et al. study, compared with women with C-IMT < 0.6 mm, women with 0.6 mm ≤ C-IMT ≤0.8 mm, and with C-IMT > 0.8 mm had multivariate odds ratios (95 % CI) of 4.88 (1.47–16.16) and 23.36 (4.54–120.14) of having any BAC, respectively [63]. The covariates in the model included age, parity, menopausal status, history of CAD, hypertension, diabetes, and smoking. Yildiz et al. reported that BAC on mammography was associated with C-IMT independently of age, parity, postmenopausal duration, diabetes, systolic blood pressure, fasting glucose, and triglyceride levels [104•]. Taken together, these studies highlight the potential of BAC for predicting clinical and sub-clinical CVD.
Multiethnic Study of Breast Arterial Calcium Gradation and Cardiovascular Risk (MINERVA)
Researchers at the Kaiser Permanente Division of Research in Northern California and at the University of California at Irvine have recently launched MINERVA, a new prospective 5-year cohort study funded by the National Heart, Lung, and Blood Institute (RO1HL106-043) that will yield novel insights into ethnic differences in BAC presence and gradation as well as into factors associated with BAC. But more importantly, MINERVA will shed light on the potential value of BAC gradation as a new tool for CVD risk stratification and thus for CVD prevention. Hence, MINERVA’s findings will break new ground and could have considerable clinical and public health significance for the millions of women who routinely undergo mammographic screening. MINERVA was designed with 3 specific aims in mind:
-
(1)
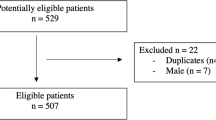
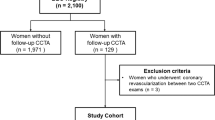
To establish a multi-ethnic cohort (n = 5400) of women between the ages of 60 and 79 years with equal representation of Caucasian (n = 1350; 25 %), African-American (n = 1350; 25 %), Asian (n = 1350; 25 %), and Hispanic/Latina (n = 1350; 25 %) females. All participants will be recruited at the time of their regular mammography screening over a period of 2 years at 3 Kaiser Permanente of Northern California (KPNC) medical centers and will have no history of prior clinical CVD. A new, but rigorously validated densitometry method will be used to estimate BAC mass (in milligrams [mg]) using digital mammograms.
-
(2)
To assess associations of BAC mass with age, race/ethnicity, family history of CVD, traditional and novel CVD risk factors, renal function, reproductive health factors, psychosocial factors, selected mineral metabolism factors, selected medication use (statins and nitrogen-containing bisphosphonates), breast size, and sleep-related factors.
-
(3)
To elucidate the role of BAC mass in the prediction of coronary heart disease (CHD), cerebrovascular disease (transient ischemic attack [TIA], hemorrhagic stroke, and ischemic stroke), heart failure, peripheral vascular disease, and total CVD and to determine whether adding BAC mass to prediction model based on traditional risk factors improves classification of risk for total CVD and its components.
Despite existing evidence suggesting that BAC is a risk factor for subclinical and clinical CVD, it is important to note that all prior studies have relied on conventional (ie, screen film) mammography. Further research is therefore needed to examine the association of BAC with CVD risk factors and CVD events using modern (ie, digital) mammographic techniques that have a much greater sensitivity level. Furthermore, the BAC literature is based on the crude assessment of absence vs presence of BAC and, to date, no study has quantified BAC mass and its relationship with CVD risk factors and events. In addition, there are significant gaps in knowledge including the association of BAC mass with other markers of subclinical CVD (ie, ankle-brachial index), other breast characteristics (ie, breast volume), renal function, preventative medications that may affect calcification (eg, statins or nitrogen-containing bisphosphonate), psychosocial factors, mineral metabolism factors (serum calcium, phosphorus, parathyroid hormone, 25-hydroxy-vitamin D concentrations), and sleep-related factors. Finally, studies like this one are needed to clarify the potential incremental prognostic value of BAC presence and BAC mass for CVD and its components in a contemporary era where widespread preventive efforts are already underway.
The densitometry technique that will be used in the MINERVA study to estimate calcium mass in mammograms is described elsewhere [106••]. In brief, anthropomorphic breast and vessel calcification phantoms were imaged using a full-field digital mammography system. A calcium calibration measurement was performed at each phantom thickness and beam energy. The known (K) and measured (M) calcium mass on phantoms 5 cm and 9 cm thick were tightly related (M = 0.964 K − 0.288 mg; r = 0.997, and M = 1.004 K + 0.324 mg; r = 0.994, respectively). The results indicate that accurate calcium mass measurements can be made without correcting for scatter glare as long as careful calcium calibrations are made for each breast thickness. The uncertainty in magnification is expected to cause up to 5 % and 15 % error in calcium mass for 5 cm and 9 cm breast thicknesses, respectively. These results demonstrate the feasibility and potential utility of our technique for accurate BAC quantification in digital mammograms. In a second study, we have demonstrated adequate reproducibility and inter-reader agreement of the BAC mass measurement [107]. Standard full-field digital mammograms were acquired from medial lateral oblique (MLO) and craniocaudal (CC) projections. Calcium mass was measured in each projection using the technique developed in the previously described phantom study (depicted in Fig. 2). In order to assess the reproducibility of calcium measurement without added radiation exposure, we compared calcium mass from 2 different projections (Fig. 3a). The measured calcium masses in MLO (MMLO) and CC (MCC) projections were highly correlated (r = 0.95). A plot of BAC mass measurements (average of MLO and CC projections for right and left breasts) performed by the 2 observers is shown in Fig. 3b. These results indicate excellent inter-reader agreement (intra-class r = 0.94) and demonstrate that our densitometry technique for quantifying BAC mass using standard full-view digital mammography is highly reproducible.
In this study, BAC was identified and regions of interest were drawn manually (Fig. 2). To make this methodology more easily adoptable by other groups and implemented in clinical settings, it is desirable to automate this process. In collaboration with 1 of the major manufacturers of mammography systems (Hologic, Inc., Bedford MA), we are in the process of evaluating a fully automated algorithm for BAC detection and extraction from mammograms. There are also other research groups pursuing a similar approach [108–110]. The automated technique will completely eliminate the inter-reader variability. It can be combined with our technique to automatically quantify calcium mass from mammograms in a clinical setting. However, the technique will require further optimization and validation before it can be used. The proposed study will provide us the opportunity to compare the results from readers and the fully automatic algorithm.
Potential Public Health and Clinical Contributions
A very large proportion of women undergo screening mammography on a regular basis after the age of 40. There are minimal costs associated with reading and grading BAC. MINERVA will shed light on the epidemiological associations between BAC mass and an extensive array of covariates. More importantly, it will establish (for the first time) the incremental utility of BAC mass for predicting clinical CHD, cerebrovascular disease, heart failure, peripheral vascular disease, and total CVD among women aged 60–79 years. While we recognize that the densitometry method to quantify BAC mass in digital mammograms that we have developed for this proposal is novel and not yet universally available, the transition to digital imaging is a reality in most major university and community hospitals. Our methodology to compute BAC mass can be easily adopted by other groups and medical centers. Furthermore, we are in the process of evaluating a fully automated algorithm for BAC detection from mammograms. The eventual automation of this technique will make its clinical implementation much easier.
What are the clinical implications? First, the discovery of BAC should trigger an investigation of risk factor levels and subsequent treatment as needed to reduce those found to be elevated. Second, a scenario where detecting extensive BAC may be particularly useful in women at moderate cardiovascular risk based on existing clinical risk algorithms. In this instance, BAC may be a useful tool for reclassifying them into the high risk group, where a more aggressive approach may be warranted.
This epidemiological study is a necessary, intermediate step to demonstrate clinical predictive utility of BAC mass. The utility of coronary calcium (which requires a separate CT scan of the heart) to significantly improve net reclassification for CHD has recently been demonstrated in the MESA study [111]. If we are able to demonstrate meaningful added risk assessment performance using BAC mass above and beyond conventional risk factors (ie, at least 10 % improvement in net reclassification with categories) [112], we would then proceed to develop new risk estimation systems for total CVD and for each of its components (CHD, cerebrovascular disease, peripheral vascular disease, and heart failure). First, we would incorporate the BAC mass score to traditional risk factors (the Framingham risk score) and second, we would add the BAC mass score to conventional risk factors plus hs-CRP and family history of CHD (the Reynolds risk score). After, we would seek collaborations to validate these new algorithms in other cohorts. Whether the provision of these new risk-estimation systems will result in benefits to healthcare providers and individual patients, in term of reductions of risk factors and/or clinical outcomes, would require further testing in clinical trials.
Assuming that BAC quantity is associated with an increased risk of CVD events, if a woman is found to have BAC, particularly highly elevated BAC mass, it should trigger an investigation of cardiovascular risk factor profile (diabetes, hypertension, lipid profile, inflammatory status) and this woman should be treated more aggressively if 1 or more of these risk factors are found to be present (in a similar fashion proposed for CAC [113, 114]. We do not advocate the reverse, that is, women presenting with risk factors being referred to mammography. The beauty of mammography is that the indication already exists for the early detection of breast cancer.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Screening for breast cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2009;151:716–26, W–236.
Bild DE, Folsom AR, Lowe LP, Sidney S, Kiefe C, Westfall AO, et al. Prevalence and correlates of coronary calcification in black and white young adults: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Arterioscler Thromb Vasc Biol. 2001;21:852–7.
Budoff MJ, Nasir K, Mao S, Tseng PH, Chau A, Liu ST, et al. Ethnic differences of the presence and severity of coronary atherosclerosis. Atherosclerosis. 2006;187:343–50.
Heron M, Sutton PD, Xu J, Ventura SJ, Strobino DM, Guyer B. Annual summary of vital statistics: 2007. Pediatrics. 2010;125:4–15.
Myerburg RJ. Scientific gaps in the prediction and prevention of sudden cardiac death. J Cardiovasc Electrophysiol. 2002;13:709–23.
Thaulow E, Erikssen J, Sandvik L, Erikssen G, Jorgensen L, Cohn PF. Initial clinical presentation of cardiac disease in asymptomatic men with silent myocardial ischemia and angiographically documented coronary artery disease (the Oslo Ischemia Study). Am J Cardiol. 1993;72:629–33.
Coronado BE, Griffith JL, Beshansky JR, Selker HP. Hospital mortality in women and men with acute cardiac ischemia: a prospective multicenter study. J Am Coll Cardiol. 1997;29:1490–6.
Tofler GH, Stone PH, Muller JE, Willich SN, Davis VG, Poole WK, et al. Effects of gender and race on prognosis after myocardial infarction: adverse prognosis for women, particularly black women. J Am Coll Cardiol. 1987;9:473–82.
Vaccarino V, Parsons L, Every NR, Barron HV, Krumholz HM. Sex-based differences in early mortality after myocardial infarction. National registry of myocardial infarction 2 participants. N Engl J Med. 1999;341:217–25.
Hasdai D, Porter A, Rosengren A, Behar S, Boyko V, Battler A. Effect of gender on outcomes of acute coronary syndromes. Am J Cardiol. 2003;91:1466–9, A1466.
Maynard C, Beshansky JR, Griffith JL, Selker HP. Influence of sex on the use of cardiac procedures in patients presenting to the emergency department. A prospective multicenter study. Circulation. 1996;94(9 Suppl):II93–8.
Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA. 2001;285:2486–97.
Khot UN, Khot MB, Bajzer CT, Sapp SK, Ohman EM, Brener SJ, et al. Prevalence of conventional risk factors in patients with coronary heart disease. JAMA. 2003;290:898–904.
Greenland P, Smith Jr SC, Grundy SM. Improving coronary heart disease risk assessment in asymptomatic people: role of traditional risk factors and noninvasive cardiovascular tests. Circulation. 2001;104:1863–7.
Naghavi M, Libby P, Falk E, Casscells SW, Litovsky S, Rumberger J, et al. From vulnerable plaque to vulnerable patient: a call for new definitions and risk assessment strategies: part II. Circulation. 2003;108:1772–8.
Greenland P, Abrams J, Aurigemma GP, Bond MG, Clark LT, Criqui MH, et al. Beyond secondary prevention: identifying the high-risk patient for primary prevention: noninvasive tests of atherosclerotic burden: writing group III. Circulation. 2000;101:E16–22.
Pearson TA. New tools for coronary risk assessment: what are their advantages and limitations? Circulation. 2002;105:886–92.
Ridker PM, Buring JE, Rifai N, Cook NR. Development and validation of improved algorithms for the assessment of global cardiovascular risk in women: the Reynolds Risk Score. JAMA. 2007;297:611–9.
Fayad ZA, Fuster V, Nikolaou K, Becker C. Computed tomography and magnetic resonance imaging for noninvasive coronary angiography and plaque imaging: current and potential future concepts. Circulation. 2002;106:2026–34.
Rajaram V, Pandhya S, Patel S, Meyer PM, Goldin M, Feinstein MJ, et al. Role of surrogate markers in assessing patients with diabetes mellitus and the metabolic syndrome and in evaluating lipid-lowering therapy. Am J Cardiol. 2004;93:32C–48C.
Taylor AJ. Atherosclerosis imaging to detect and monitor cardiovascular risk. Am J Cardiol. 2002;90:8L–11L.
Kondos GT, Hoff JA, Sevrukov A, Daviglus ML, Garside DB, Devries SS, et al. Electron-beam tomography coronary artery calcium and cardiac events: a 37-month follow-up of 5635 initially asymptomatic low- to intermediate-risk adults. Circulation. 2003;107:2571–6.
Lakoski SG, Greenland P, Wong ND, Schreiner PJ, Herrington DM, Kronmal RA, et al. Coronary artery calcium scores and risk for cardiovascular events in women classified as "low risk" based on Framingham risk score: the multi-ethnic study of atherosclerosis (MESA). Arch Intern Med. 2007;167:2437–42.
Kim KP, Einstein AJ, Berrington de Gonzalez A. Coronary artery calcification screening: estimated radiation dose and cancer risk. Arch Intern Med. 2009;169:1188–94.
US Preventive Services Task Force. Screening for breast cancer. Rockville: Agency for Healthcare Research and Quality; 2002.
Ostbye T, Greenberg GN, Taylor Jr DH, Lee AM. Screening mammography and Pap tests among older American women 1996–2000: results from the Health and Retirement Study (HRS) and Asset and Health Dynamics Among the Oldest Old (AHEAD). Ann Fam Med. 2003;1:209–17.
Adcock K. Initiative to improve mammogram interpretation. Permanente J. 2004;8:12–8.
Breen N, A Cronin K, Meissner HI, Taplin SH, Tangka FK, Tiro JA, et al. Reported drop in mammography: is this cause for concern? Cancer. 2007;109:2405–9.
Norman SA, Weinberg GB, Krampe BR, Finnegan ET. Benefits of collecting local data on breast cancer and mammography practices in northwestern Pennsylvania. Public Health Rep. 1993;108:395–401.
Orel SG, Kay N, Reynolds C, Sullivan DC. BI-RADS categorization as a predictor of malignancy. Radiology. 1999;211:845–50.
Shaw CC, Wang T, King JL, Breitenstein DS, Chang TS, Harris KM, et al. Computed radiography vs screen-film mammography in detection of simulated microcalcifications: a receiver operating characteristic study based on phantom images. Acad Radiol. 1998;5:173–80.
Chen NX, Moe SM. Arterial calcification in diabetes. Curr Diab Rep. 2003;3:28–32.
Shanahan CM, Proudfoot D, Tyson KL, Cary NR, Edmonds M, Weissberg PL. Expression of mineralization-regulating proteins in association with human vascular calcification. Z Kardiol. 2000;89 Suppl 2:63–8.
Wallin R, Wajih N, Greenwood GT, Sane DC. Arterial calcification: a review of mechanisms, animal models, and the prospects for therapy. Med Res Rev. 2001;21:274–301.
Trion A, van der Laarse A. Vascular smooth muscle cells and calcification in atherosclerosis. Am Heart J. 2004;147:808–14.
Shanahan CM, Cary NR, Salisbury JR, Proudfoot D, Weissberg PL, Edmonds ME. Medial localization of mineralization-regulating proteins in association with Monckeberg's sclerosis: evidence for smooth muscle cell-mediated vascular calcification. Circulation. 1999;100:2168–76.
Farzaneh-Far A, Proudfoot D, Shanahan C, Weissberg PL. Vascular and valvar calcification: recent advances. Heart. 2001;85:13–7.
Edmonds ME, Morrison N, Laws JW, Watkins PJ. Medial arterial calcification and diabetic neuropathy. Br Med J (Clin Res Ed). 1982;284:928–30.
Mönckeberg J. Uber die reine Mediaverkalkung der Extremitätenarterien und ihr Verhalten zur Arteriosklerose. Virchows Arch Pathol Anat. 1902;171:141–67.
Tomson C. Vascular calcification in chronic renal failure. Nephron Clin Pract. 2003;93:c124–30.
Everhart JE, Pettitt DJ, Knowler WC, Rose FA, Bennett PH. Medial arterial calcification and its association with mortality and complications of diabetes. Diabetologia. 1988;31:16–23.
Chantelau E, Lee KM, Jungblut R. Association of below-knee atherosclerosis to medial arterial calcification in diabetes mellitus. Diabetes Res Clin Pract. 1995;29:169–72.
Lehto S, Niskanen L, Suhonen M, Ronnemaa T, Laakso M. Medial artery calcification. A neglected harbinger of cardiovascular complications in non-insulin-dependent diabetes mellitus. Arterioscler Thromb Vasc Biol. 1996;16:978–83.
London GM, Guerin AP, Marchais SJ, Metivier F, Pannier B, Adda H. Arterial media calcification in end-stage renal disease: impact on all-cause and cardiovascular mortality. Nephrol Dial Transplant. 2003;18:1731–40.
Sakata N, Noma A, Yamamoto Y, Okamoto K, Meng J, Takebayashi S, et al. Modification of elastin by pentosidine is associated with the calcification of aortic media in patients with end-stage renal disease. Nephrol Dial Transplant. 2003;18:1601–9.
Nielsen B, Holm N. Calcification in breast arteries. The frequency and severity of arterial calcification in female breast tissue without malignant changes. Acta Pathol Microbiol Immunol Scand. 1986;93:13–6.
Kim H, Greenberg JS, Javitt MC. Breast calcifications due to Monckeberg medial calcific sclerosis. Radiographics. 1999;19:1401–3.
Proudfoot D, Shanahan CM. Biology of calcification in vascular cells: intima vs media. Herz. 2001;26:245–51.
Leinster SJ, Whitehouse GH. Factors which influence the occurrence of vascular calcification in the breast. Br J Radiol. 1987;60:457–8.
Blackman GAL, Coughlin B, et al. Breast arterial calcifications on mammography: incidence in various age groups (Abstract). Radiology. 2002;225:553.
Dale PS, Mascarhenas C, Richards M, Mackie G. Mammography as a screening tool for coronary artery disease. J Surg Res. 2008;148:1–6.
Reddy J, Son H, Smith SJ, Paultre F, Mosca L. Prevalence of breast arterial calcifications in an ethnically diverse population of women. Ann Epidemiol. 2005;15:344–50.
Dale PS, Graham J, Nichols KW, Catchings T, Richards M. Mammography as a screening tool for peripheral vascular disease. Am J Surg. 2006;192:488–91.
Henkin Y, Abu-Ful A, Shai I, Crystal P. Lack of association between breast artery calcification seen on mammography and coronary artery disease on angiography. J Med Screen. 2003;10:139–42.
Iribarren C, Go AS, Tolstykh I, Sidney S, Johnston SC, Spring DB. Breast vascular calcification and risk of coronary heart disease, stroke, and heart failure. J Womens Health. 2004;13:381–9. discussion 390–382.
Kataoka M, Warren R, Luben R, Camus J, Denton E, Sala E, et al. How predictive is breast arterial calcification of cardiovascular disease and risk factors when found at screening mammography? Am J Roentgenol. 2006;187:73–80.
Maas AH, van der Schouw YT, Atsma F, Beijerinck D, Deurenberg JJ, Mali WP, et al. Breast arterial calcifications are correlated with subsequent development of coronary artery calcifications, but their etiology is predominantly different. Eur J Radiol. 2007;63:396–400.
Schmitt EL, Threatt BA. Relationship of mammographic intra-arterial calcifications and diabetes. South Med J. 1984;77:988–9.
Sickles EA, Galvin HB. Breast arterial calcification in association with diabetes mellitus: too weak a correlation to have clinical utility. Radiology. 1985;155:577–9.
Maas AH, van der Schouw YT, Mali WP, van der Graaf Y. Prevalence and determinants of breast arterial calcium in women at high risk of cardiovascular disease. Am J Cardiol. 2004;94:655–9.
van Noord PA, Beijerinck D, Kemmeren JM, van der Graaf Y. Mammograms may convey more than breast cancer risk: breast arterial calcification and arterio-sclerotic related diseases in women of the DOM cohort. Eur J Cancer Prev. 1996;5:483–7.
Cetin M, Cetin R, Tamer N. Prevalence of breast arterial calcification in hypertensive patients. Clin Radiol. 2004;59:92–5.
Sedighi N, Radmard AR, Radmehr A, Hashemi P, Hajizadeh A, Taheri AP. Breast arterial calcification and risk of carotid atherosclerosis: focusing on the preferentially affected layer of the vessel wall. Eur J Radiol. 2011;79:250–6.
Pidal D, Sanchez Vidal MT, Rodriguez JC, Corte MD, Pravia P, Guinea O, et al. Relationship between arterial vascular calcifications seen on screening mammograms and biochemical markers of endothelial injury. Eur J Radiol. 2009;69:87–92.
Vattikuti R, Towler DA. Osteogenic regulation of vascular calcification: an early perspective. Am J Physiol Endocrinol Metab. 2004;286:E686–96.
Browner WS, Lui LY, Cummings SR. Associations of serum osteoprotegerin levels with diabetes, stroke, bone density, fractures, and mortality in elderly women. J Clin Endocrinol Metab. 2001;86:631–7.
Fuster Selva MJ, Orozco Beltran D, Saez Castan J, Merino Sanchez J. Association between breast arterial calcifications and degree of control and severity of diabetes. Med Clin. 2004;122:329–33.
Maas AH, van der Schouw YT, Beijerinck D, Deurenberg JJ, Mali WP, van der Graaf Y. Arterial calcifications seen on mammograms: cardiovascular risk factors, pregnancy, and lactation. Radiology. 2006;240:33–8.
Prentice A. Maternal calcium metabolism and bone mineral status. Am J Clin Nutr. 2000;71(5 Suppl):1312S–6S.
Ram KT, Bobby P, Hailpern SM, Lo JC, Schocken M, Skurnick J, et al. Duration of lactation is associated with lower prevalence of the metabolic syndrome in midlife–SWAN, the study of women's health across the nation. Am J Obstet Gynecol. 2008;198:268 e261–6.
Cox J, Simpson W, Walshaw D. An interesting byproduct of screening: assessing the effect of HRT on arterial calcification in the female breast. J Med Screen. 2002;9:38–9.
Kemmeren JM, van Noord PA, Beijerinck D, Fracheboud J, Banga JD, van der Graaf Y. Arterial calcification found on breast cancer screening mammograms and cardiovascular mortality in women: the DOM project. Doorlopend Onderzoek Morbiditeit en Mortaliteit. Am J Epidemiol. 1998;147:333–41.
Manson JE, Allison MA, Rossouw JE, Carr JJ, Langer RD, Hsia J, et al. Estrogen therapy and coronary-artery calcification. N Engl J Med. 2007;356:2591–602.
Akhrass F, Evans AT, Wang Y, Rich S, Kannan CR, Fogelfeld L, et al. Hormone replacement therapy is associated with less coronary atherosclerosis in postmenopausal women. J Clin Endocrinol Metab. 2003;88:5611–4.
Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351:1296–305.
Stamatelopoulos KS, Lekakis JP, Tseke P, Ikonomidis I, Kollias GE, Alevizaki M, et al. Differential associations of renal function with coronary and peripheral atherosclerosis. Int J Cardiol. 2009;135:162–4.
Sorajja D, Gami AS, Somers VK, Behrenbeck TR, Garcia-Touchard A, Lopez-Jimenez F. Independent association between obstructive sleep apnea and subclinical coronary artery disease. Chest. 2008;133:927–33.
Takama N, Kurabayashi M. Possibility of close relationship between sleep disorder breathing, and acute coronary syndrome. J Cardiol. 2007;49:171–7.
Lauderdale DS, Knutson KL, Yan LL, Rathouz PJ, Hulley SB, Sidney S, et al. Objectively measured sleep characteristics among early-middle-aged adults: the CARDIA study. Am J Epidemiol. 2006;164:5–16.
Peker Y, Carlson J, Hedner J. Increased incidence of coronary artery disease in sleep apnoea: a long-term follow-up. Eur Respir J. 2006;28:596–602.
King CR, Knutson KL, Rathouz PJ, Sidney S, Liu K, Lauderdale DS. Short sleep duration and incident coronary artery calcification. JAMA. 2008;300:2859–66.
Martins D, Wolf M, Pan D, Zadshir A, Tareen N, Thadhani R, et al. Prevalence of cardiovascular risk factors and the serum levels of 25-hydroxyvitamin D in the United States: data from the Third National Health and Nutrition Examination Survey. Arch Intern Med. 2007;167:1159–65.
Giovannucci E, Liu Y, Hollis BW, Rimm EB. 25-hydroxyvitamin D and risk of myocardial infarction in men: a prospective study. Arch Intern Med. 2008;168:1174–80.
Wang TJ, Pencina MJ, Booth SL, Jacques PF, Ingelsson E, Lanier K, et al. Vitamin D deficiency and risk of cardiovascular disease. Circulation. 2008;117:503–11.
Rubin MR, Rundek T, McMahon DJ, Lee HS, Sacco RL, Silverberg SJ. Carotid artery plaque thickness is associated with increased serum calcium levels: the Northern Manhattan study. Atherosclerosis. 2007;194:426–32.
Lind L, Skarfors E, Berglund L, Lithell H, Ljunghall S. Serum calcium: a new, independent, prospective risk factor for myocardial infarction in middle-aged men followed for 18 years. J Clin Epidemiol. 1997;50:967–73.
Wei M, Esbaei K, Bargman J, Oreopoulos DG. Relationship between serum magnesium, parathyroid hormone, and vascular calcification in patients on dialysis: a literature review. Perit Dial Int. 2006;26:366–73.
Budoff MJ, Raggi P. Coronary artery disease progression assessed by electron-beam computed tomography. Am J Cardiol. 2001;88:46E–50E.
Callister TQ, Raggi P, Cooil B, Lippolis NJ, Russo DJ. Effect of HMG-CoA reductase inhibitors on coronary artery disease as assessed by electron-beam computed tomography. N Engl J Med. 1998;339:1972–8.
Arad Y, Spadaro LA, Roth M, Newstein D, Guerci AD. Treatment of asymptomatic adults with elevated coronary calcium scores with atorvastatin, vitamin C, and vitamin E: the St. Francis Heart Study randomized clinical trial. J Am Coll Cardiol. 2005;46:166–72.
Raggi P, Davidson M, Callister TQ, Welty FK, Bachmann GA, Hecht H, et al. Aggressive vs moderate lipid-lowering therapy in hypercholesterolemic postmenopausal women: Beyond Endorsed Lipid Lowering with EBT Scanning (BELLES). Circulation. 2005;112:563–71.
Adami S, Braga V, Guidi G, Gatti D, Gerardi D, Fracassi E. Chronic intravenous aminobisphosphonate therapy increases high-density lipoprotein cholesterol and decreases low-density lipoprotein cholesterol. J Bone Miner Res. 2000;15:599–604.
Pennanen N, Lapinjoki S, Urtti A, Monkkonen J. Effect of liposomal and free bisphosphonates on the IL-1 beta, IL-6, and TNF alpha secretion from RAW 264 cells in vitro. Pharm Res. 1995;12:916–22.
Nitta K, Akiba T, Suzuki K, Uchida K, Watanabe R, Majima K, et al. Effects of cyclic intermittent etidronate therapy on coronary artery calcification in patients receiving long-term hemodialysis. Am J Kidney Dis. 2004;44:680–8.
Wada H, Hirano F, Kuroda T, Shiraki M. Breast arterial calcification and hypertension associated with vertebral fracture. Geriatr Gerontol Int. 2012;12:330–5.
Reddy J, Bilezikian JP, Smith SJ, Mosca L. Reduced bone mineral density is associated with breast arterial calcification. J Clin Endocrinol Metab. 2008;93:208–11.
Schnatz PF, Marakovits KA, O'Sullivan DM. The association of breast arterial calcification and coronary heart disease. Obstet Gynecol. 2011;117(2 Pt 1):233–41.
Doerger K, Whaley D, Berger P, et al. Breast arterial calcification detected on mammography is a risk factor for coronary artery disease (abstract). Radiology. 2002;225:553.
Fiuza Ferreira EM, Szejnfeld J, Faintuch S. Correlation between intramammary arterial calcifications and CAD. Acad Radiol. 2007;14:144–50.
Topal U, Kaderli A, Topal NB, Ozdemir B, Yesilbursa D, Cordan J, et al. Relationship between the arterial calcification detected in mammography and coronary artery disease. Eur J Radiol. 2007;63:391–5.
Ferreira JA, Pompei LM, Fernandes CE, Azevedo LH, Peixoto S. Breast arterial calcification is a predictive factor of cardiovascular disease in Brazilian postmenopausal women. Climacteric. 2009;12:439–44.
Oliveira EL, Freitas-Junior R, Afiune-Neto A, Murta EF, Ferro JE, Melo AF. Vascular calcifications seen on mammography: an independent factor indicating coronary artery disease. Clinics. 2009;64:763–7.
•• Abi Rafeh N, Castellanos MR, Khoueiry G, Meghani M, El-Sayegh S, Wetz RV, Lafferty JC, et al. Association between coronary artery disease diagnosed by coronary angiography and breast arterial calcifications on mammography: meta-analysis of the data. J Womens Health. 2012; [Epub 2012 Sep 20]. This article is a meta-analysis of previous studies evaluating BAC as a risk marker for coronary artery disease that included 927 patients. There was a 1.59 (95 % confidence interval [CI] 1-21-2.09) increased odds of angiographically defined CAD in patients with BAC seen on mammography.
• Yildiz S, Yildiz A, Ertug N, Kaya I, Yilmaz R, Yuksel E, et al. Association of breast arterial calcification and carotid intima-media thickness. Hear Vessel. 2008;23:376–82. Findings of this study show that BAC on mammography is independently associated with carotid IMT, another clinically useful surrogate of atherosclerosis.
•• Ahn KJ, Kim YJ, Cho HJ, Yim HW, Kang BJ, Kim SH, et al. Correlation between breast arterial calcification detected on mammography and cerebral artery disease. Arch Gynecol Obstet. 2011;284:957–64. This study demonstrates a strong correlation between BAC presence and positive MRI findings (specifically white matter and periventricular hyperintensity thus supporting the notion that BAC may be a useful marker of women at higher risk for stroke.
•• Molloi S, Xu T, Ducote J, Iribarren C. Quantification of breast arterial calcification using full field digital mammography. Med Phys. 2008;35:1428–39. This paper describes a new densitometry method to estimate BAC gradation in terms of vascular calcium inclusion in mg. This method will allow examining, for the first time, the dose-response relationship of BAC with clinical outcomes (as opposed to absence vs. presence of BAC).
Molloi S, Mehraien T, Iribarren C, Smith C, Ducote JL, Feig SA. Reproducibility of breast arterial calcium mass quantification using digital mammography. Acad Radiol. 2009;16:275–82.
Cheng J, Chen C, Cole E, Pisano E, Shen D. Automated delineation of calcified vessels in mammography by tracking with uncertainty and graphical linking techniques. IEEE Trans Med Imaging. 2012. doi:10.1109/TMI.2012.2215880.
Cheng JZ, Cole EB, Pisano ED, Shen D. Detection of arterial calcification in mammograms by random walks. Inf Process Med Imaging. 2009;21:713–24.
Ge J, Chan H-P, Sahiner B, Zhou C, Helvie MA, Wei J, et al. Automated detection of breast vascular calcification on full-field digital mammograms. Proc SPIE Med Img. 2008;691517:1–7.
Polonsky TS, McClelland RL, Jorgensen NW, Bild DE, Burke GL, Guerci AD, et al. Coronary artery calcium score and risk classification for coronary heart disease prediction. JAMA. 2010;303:1610–6.
Pencina MJ, D'Agostino RB, Vasan RS. Review: statistical methods for assessment of added usefulness of new biomarkers. Clin Chem Lab Med. 2010;48:1703–11.
Budoff MJ, Achenbach S, Blumenthal RS, Carr JJ, Goldin JG, Greenland P, et al. Assessment of coronary artery disease by cardiac computed tomography: a scientific statement from the American Heart Association Committee on Cardiovascular Imaging and Intervention, Council on Cardiovascular Radiology and Intervention, and Committee on Cardiac Imaging, Council on Clinical Cardiology. Circulation. 2006;114:1761–91.
Greenland P, Bonow RO, Brundage BH, Budoff MJ, Eisenberg MJ, Grundy SM, et al. ACCF/AHA 2007 clinical expert consensus document on coronary artery calcium scoring by computed tomography in global cardiovascular risk assessment and in evaluation of patients with chest pain: a report of the American College of Cardiology Foundation Clinical Expert Consensus Task Force (ACCF/AHA Writing Committee to Update the 2000 Expert Consensus Document on Electron Beam Computed Tomography) developed in collaboration with the Society of Atherosclerosis Imaging and Prevention and the Society of Cardiovascular Computed Tomography. J Am Coll Cardiol. 2007;49:378–402.
Disclosure
No potential conflicts of interest relevant to this article were reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Iribarren, C., Molloi, S. Breast Arterial Calcification: a New Marker of Cardiovascular Risk?. Curr Cardiovasc Risk Rep 7, 126–135 (2013). https://doi.org/10.1007/s12170-013-0290-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12170-013-0290-4