Abstract
Objective
123I metaiodobenzylguanidine (MIBG) scintigraphy is a useful tool for the diagnosis of pheochromocytomas (PHEOs), but some PHEOs are difficult to differentiate from cortical adenoma (CA) or normal adrenal uptake by visual evaluation alone. A new semi-quantitative analysis using 123I MIBG SPECT/CT is thus expected. Herein, we introduce the tumor-to-liver count ratio (T/L) and the tumor-to-muscle count ratio (T/M).
Methods
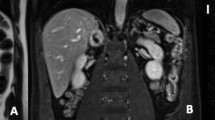
We examined the cases of 21 patients with PHEOs (10 males, 11 females; age 24–80, median 61 years) and 23 patients with CA (15 males and 8 females, age 30–78, median 58 years). The visual scoring based on 123I MIBG planar images (planar score) and SPECT images (SPECT score) was used as the conventional evaluation. Using 123I MIBG SPECT/CT findings, we calculated the semi-quantitative values of the count ratio using the maximum or mean count of the tumor and the liver or muscle as the reference organ (T/Lmax, T/Lmean, T/Mmax and T/Mmean). Each evaluation of the PHEOs and CAs was compared, and the diagnosing performance was evaluated based on an ROC analysis.
Results
The area under curve (AUC) values were as follows: the planar score, 0.833; SPECT score, 0.813; T/Lmax, 0.986; T/Lmean, 0.975; T/Mmax, 0.955; and T/Mmean, 0.933. The AUC for T/Mmax was significantly higher than those of the planar score, and SPECT score by ROC analysis (p < 0.01 each).
Conclusion
The semi-quantitative value of 123I MIBG SPECT/CT is more useful than the conventional visual evaluation for differentiating PHEOs from CAs.



Similar content being viewed by others
References
Amar L, Servais A, Roqueplo APG, Zinzindohoue F, Chatellier G, Plouin PF. Year of diagnosis, features at presentation, and risk of recurrence in patients with pheochromocytoma or secreting paraganglioma. J Clin Endocrinol Metab. 2005;90(4):2110–6.
Bessell-Brownel R, O’Malley EO. CT of pheochromocytoma and paraganglioma: risk of adverse events with i.v. administration of nonionic contrast material. Am J Roentgenol. 2007;188:970–4.
Varghese JC, Hahn PF, Papanicolaou N, Mayo-Smith WW, Gaa JA, Lee MJ. MR differentiation of phaeochromocytoma from other adrenal lesions based on qualitative analysis of T2 relaxation times. Clin Radiol. 1997;52:603–6.
Blake M, Kalra M, Maher M, Shani D, Sweeney A, Mueller P, et al. Pheochromocytoma: an imaging chameleon. Radiographics. 2004;24(Suppl. 1):S87–99.
Tenenbaum F, Lumbroso J, Schlumberger M, Mure A, Plouin P, Caillou B, et al. Comparison of radiolabeled octreotide and meta-iodobenzylguanidine (MIBG) scintigraphy in malignant pheochromocytoma. J Nucl Med. 1995;36:1–6.
Bomani J, Levison DA, Flagman WD, Home T, Bollox PM, Ross G, et al. Uptake of iodine-123 MIBG by pheochromocytomas, paragangliomas, and neuroblastomas: a histological comparison. J Nucl Med. 1987;28:973–8.
Havekes B, Lai EW, Corssmit EP, Romijn JA, Timmers HJ, Pacak K. Detection and treatment of pheochromocytomas and paragangliomas: current standing of MIBG scintigraphy and future role of PET imaging. Q J Nucl Med Mol Imaging. 2008;52:419–29.
Lumachi F, Tregnaghi A, Zucchetta P, Cristina MM, Cecchin D, Grassetto G, et al. Sensitivity and positive predictive value of CT, MRI and 123I-MIBG scintigraphy in localizing pheochromocytomas: a prospective study. Nucl Med Commun. 2006;27:583–7.
Cecchin D, Lumachi F, Marzola MC, Opocher G, Scaroni C, Zucchetta P, et al. A meta-iodobenzylguanidine scintigraphic scoring system increases accuracy in the diagnostic management of pheochromocytoma. Endocr Relat Cancer. 2006;13:525–33.
Yung B, Loke T, Tse T, Tsang M, Chang J. Sporadic MIBG bilateral adrenal medullary hyperplasia: apparent false positive MIBG scan and expected MRI findings. Eur J Radiol. 2000;36:28–31.
Fendler W, Melzer H, Walz C, Schweinitz D, Coppenrath E, Schmid I, Bartenstein P, et al. High 123I-MIBG uptake in neuroblastic tumours indicates unfavourable histopathology. Eur J Nucl Med Mol Imaging. 2013;40:1701–10.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No potential conflicts of interest were disclosed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kitamura, Y., Baba, S., Isoda, T. et al. Usefulness of semi-quantitative analysis in 123I metaiodobenzylguanidine SPECT/CT for the differentiation of pheochromocytoma and cortical adenoma. Ann Nucl Med 36, 95–102 (2022). https://doi.org/10.1007/s12149-021-01690-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-021-01690-9