Abstract
Obsessive-compulsive disorder (OCD) is characterized by cognitive abnormalities encompassing several executive processes. Neuroimaging studies highlight functional abnormalities of executive fronto-parietal network (FPN) and default-mode network (DMN) in OCD patients, as well as of the prefrontal cortex (PFC) more specifically. We aim at assessing the presence of functional connectivity (FC) abnormalities of intrinsic brain networks and PFC in OCD, possibly underlying specific computational impairments and clinical manifestations. A systematic review of resting-state fMRI studies investigating FC was conducted in unmedicated OCD patients by querying three scientific databases (PubMed, Scopus, PsycInfo) up to July 2022 (search terms: “obsessive–compulsive disorder” AND “resting state” AND “fMRI” AND “function* *connect*” AND “task-positive” OR “executive” OR “central executive” OR “executive control” OR “executive-control” OR “cognitive control” OR “attenti*” OR “dorsal attention” OR “ventral attention” OR “frontoparietal” OR “fronto-parietal” OR “default mode” AND “network*” OR “system*”). Collectively, 20 studies were included. A predominantly reduced FC of DMN – often related to increased symptom severity – emerged. Additionally, intra-network FC of FPN was predominantly increased and often positively related to clinical scores. Concerning PFC, a predominant hyper-connectivity of right-sided prefrontal links emerged. Finally, FC of lateral prefrontal areas correlated with specific symptom dimensions. Several sources of heterogeneity in methodology might have affected results in unpredictable ways and were discussed. Such findings might represent endophenotypes of OCD manifestations, possibly reflecting computational impairments and difficulties in engaging in self-referential processes or in disengaging from cognitive control and monitoring processes.
Similar content being viewed by others
Introduction
Obsessive–compulsive disorder (OCD) is a psychiatric condition affecting 2–3% of the population characterized by somatosensory, motor, cognitive and affective abnormalities (Ruscio et al., 2010). Typical manifestations include thought disturbances, with or without behavioral sequelae, categorized as obsessions (i.e., intrusive and recurrent thoughts, mental images or impulses) and compulsions (mental or behavioral actions occurring in the form of rituals intended at neutralizing obsessions and at reducing obsessions-related negative affects) (American Psychiatric Association, 2013). After decades of research, the underlying mechanisms at the basis of OCD remain elusive. Some hints come from evidence of impairments in executive functions (Norman et al., 2019; Snyder et al., 2015) and from recent theoretical accounts proposing computational abnormalities at the basis of OCD (Fradkin et al., 2020). Such abnormalities and their phenomenological correlates might emerge from intrinsic functional connectivity (FC) alterations within and between brain networks subserving either task-dependent or task-independent processes (Menon 2011). In this light, we aimed at reviewing findings about intrinsic FC abnormalities in OCD and discussing them also from a computational perspective.
Executive deficits in OCD and relationships with clinical features
OCD patients are characterized by a broad spectrum of cognitive abnormalities, mainly encompassing executive functions (Bora, 2020; Norman et al., 2019; Snyder et al., 2015). Interestingly, executive deficits were also identified in relatives of OCD patients and in the premorbid phase (Bora, 2020; Cavedini et al., 2010; Chamberlain et al., 2007). Thus, they have been proposed as an endophenotype of OCD (Cavedini et al., 2010; Suhas & Rao, 2019). Specifically, impairments in planning (Cavedini et al., 2010; Kashyap et al., 2013; Tükel et al., 2012), set-shifting (Fenger et al., 2005; Lacerda et al., 2003), cognitive flexibility and inhibition (Rosa-Alcázar et al., 2020; Tükel et al., 2012), decision-making (Cavallaro et al., n.d.; Cavedini et al., 2010; Kashyap et al., 2013; Starcke et al., 2010), implementation and maintenance of goal-directed behaviors (Gillan & Robbins 2014; Gillan et al., 2014), and performance monitoring (Endrass & Ullsperger 2014; Endrass et al., 2010) have been found. Interestingly, decision-making was particularly affected in conditions of uncertainty (Banca n.d.; Pushkarskaya et al., 2015), whose intolerance seems to promote information gathering and checking behaviors, especially in OCD patients (Toffolo et al., 2016) but also in subclinical (Fradkin et al., 2020) and healthy participants (Bennett et al., 2016).
Concerning the relationship between obsessive–compulsive symptoms and executive performance, the literature is sparse and inconsistent (Abramovitch et al., 2019; Suhas & Rao, 2019). Nonetheless, associations between executive impairments and specific clinical dimensions (Bragdon et al., 2018; Pedron et al., 2015) were reported, along with evidence that obsessional beliefs affect executive performance (Martínez-Esparza et al., 2021).
Executive and default-mode networks in obsessive–compulsive disorder
Functional alterations in large-scale circuits have been found across several neuropsychiatric disorders (Wang et al., 2021). Hence, understanding neurofunctional dynamics at the system level may shed light on brain dysfunctions in psychopathology (Menon & Uddin, 2010; Menon, 2011).
Concerning OCD, both executive and default-mode networks were found to be altered. Precisely, aberrant intrinsic and task-related FC has been reported for executive and fronto-parietal networks (FPN) (Stern et al., 2012; Vries et al., 2014) subserving attentional shifting and cognitive control (Menon, 2011; Vossel et al., 2014), default-mode network (DMN) (Koch et al., 2018; Posner et al., 2017; Stern et al., 2012) implicated in self-referential processes and episodic memory retrieval (Raichle, 2015), fronto-striatal and cortico-limbic circuits (Vaghi et al., 2017; Vaghi et al., 2017; Vries et al., 2019) implicated in reward, learning and adaptive selection of behavior (Averbeck & O’Doherty, 2021; Graybiel & Grafton, 2015).
Additionally, relationships between FC patterns and indices of symptom severity or cognitive impairments were reported (Vaghi et al., 2017), although results are often inconsistent across studies. A recent meta-analysis (Gürsel et al., 2018) supports the presence of FC alterations in OCD mainly encompassing FPN, DMN, fronto-striatal network and salience network (SN), the latter being implicated in the detection of salient stimuli and regulating the switching between default-mode and executive networks (Menon, 2011). Intriguingly, specific FC alterations of such brain networks have been proposed to represent neural fingerprints of OCD (Vaghi et al., 2017). A depiction of canonical networks adapted from (Menon & D’Esposito, 2022) by means of BioImage Suite software (Papademetris et al., 2006) (http://www.bioimagesuite.org) is shown in Fig. 1.
Depiction of the three canonical networks adapted from (Menon & D’Esposito 2022) with the help of BioImage Suite software (Papademetris et al., 2006) (http://www.bioimagesuite.org). A: fronto-parietal network (FPN). B: default-mode network (DMN). C: salience network (SN)
The role of the prefrontal cortex
The above-discussed literature may suggest the involvement of prefrontal abnormalities in OCD, as the prefrontal cortex (PFC) plays a key role in executive functioning and cognitive control (for reviews, see (Menon & D’Esposito, 2022; Friedman & Robbins, 2022)). Such abnormalities, if present also at rest, might represent an intrinsic vulnerability factor for the development of executive dysfunctions – extensively observed in OCD patients – and specific obsessive–compulsive symptoms (e.g., behavioral disinhibition).
Concerning the role of PFC in OCD (for reviews, see (Milad & Rauch, 2012; Ahmari & Rauch, 2022)), fronto-striatal dysfunctions have been proposed as the mechanism underlying both cognitive (Snyder et al., 2015) and clinical (Burguière et al., 2015) impairments. Consistently, aberrant metabolism of several lateral and medial prefrontal subdivisions were reported (Millet, 2013; Moon & Jeong, 2018) and, in some cases, structural and functional PFC alterations were associated with severity scores (Beucke et al., 2013; Moon & Jeong, 2018) and their improvement after treatment (Straten et al., 2017).
Additionally, FC alterations of PFC have been reported in OCD patients (Beucke et al., 2013; Vries et al., 2019), in some cases associated with symptom severity (Beucke et al., 2013; Sha, 2020) and executive deficits (Vaghi et al., 2017). Intriguingly, activity and connectivity of PFC was altered during executive tasks in OCD patients (Vaghi et al., 2017; Vaghi et al., 2017) and different prefrontal subdivisions were associated with specific symptom dimensions during symptom-provoking tasks (Mataix-Cols et al., 2004).
Furthermore, executive processes seem to be characterized by a partially asymmetric organization. Indeed, criterion setting (i.e., the ability to flexibly set up rules and associations to perform specific tasks) is subserved more by left lateral PFC, whereas monitoring (i.e., the ability to evaluate internal and external contingencies to update representations) is subserved more by right lateral PFC (for reviews, see (Stuss, 2011; Vallesi, 2020)).
Therefore, deficits in performance monitoring and cognitive flexibility, along with enhanced control and checking behaviors, might reflect lateralized prefrontal abnormalities.
Hypotheses and aims
We hypothesize that OCD might show FC alterations within and/or between neural systems subserving cognitive control and attentional shifts (Menon, 2019; Menon, 2011; Vossel et al., 2014). Specifically, OCD might be characterized by increased FC in FPNs, putatively underlying hyper-active cognitive control and attentional mechanisms. Additionally, functional abnormalities of DMN might also characterize OCD, as they: (i) anti-correlate with FPNs; (ii) subserve functions whose disruption might explain some OCD abnormalities; and (iii) can be modulated by salience attributed to external and internal events (Menon, 2019; Menon & Uddin, 2010; Raichle, 2015). Moreover, OCD might be characterized by aberrant FC of right-lateralized prefrontal regions subserving monitoring, consistently with literature about OCD manifestations (Bucci et al., 2007; Endrass & Ullsperger, 2014; Endrass et al., 2010; Riesel et al., 2014) and theoretical accounts about the role of the PFC (Stuss, 2011; Vallesi, 2020). Finally, potential prefrontal inter-hemispheric alterations are not excluded, as executive functioning is hypothesized to, at least partially, emerge from the interplay between lateralized sub-functions (Vallesi, 2020).
To address such hypotheses, we conducted a systematic review of resting state (rs-) fMRI studies investigating FC of FPNs and DMN in OCD patients. We restricted our search to rs-fMRI studies to reduce potential task-related heterogeneities. Indeed, the huge variability associated with experimental designs represents a major confound, especially when investigating neurofunctional correlates of higher-order cognitive processes. Effects due to medications were minimized by selecting studies with unmedicated or drug-naïve samples (Snyder et al., 2015). By excluding medicated patients, we aimed at identifying aberrant patterns of FC uniquely associated with the OCD condition per se occurring above and beyond pharmacological interventions.
In the literature, there are recent meta-analyses of rs-FC in OCD, which however focused only on studies implementing a seed-based whole-brain approach (Gürsel et al., 2018; Liu et al., 2022). While reducing variability in methodology, the choice of seed-based analyses might have biased the results by excluding specific circuits of interest, which do not include the selected seed(s). For instance, by selecting exclusively striatum, thalamus and ACC as seeds (Liu et al., 2022), only circuits including subcortical areas and ACC could be identified, leading to overlook cortico-cortical circuits. Thus, the present review aims at overcoming such limitations by integrating results obtained with different methodological approaches, in order to provide a more complete overview of the neurofunctional alterations associated with OCD.
Moreover, Gürsel and colleagues (Gürsel et al., 2018) considered alterations in positive and negative connectivity as analogously interpretable (e.g., decreased positive connectivity and increased negative connectivity were both interpreted as hypoconnectivity). However, positive and negative FC patterns seem to reflect different types of interactions between brain areas (Fox et al., n.d.). Therefore, considering them altogether could posit interpretational issues. Thus, we critically evaluated altered FC patterns also by distinguishing the results in terms of either functional coupling or decoupling.
Methods and materials
Search strategy
The present systematic review was performed according to PRISMA guidelines (Moher et al., 2009; Liberati, et al., 2009). Literature search was carried out on three scientific databases (Scopus, PsycInfo, PubMed) including articles published until July 2022. We included in the search terms all labels indicating networks subserving cognitive control and attentional functions (Witt et al., 2020). Nonetheless, given the high number of labels present in literature and, importantly, the lack of agreement regarding the topological overlap between networks (Witt et al., 2020), we will always collectively refer to these circuits as "Fronto-Parietal Network" (FPN), regardless of the original labels used. Specifically, we chose this label since it is used for referring to all four meta-analytical clusters of regions subserving executive functions(Witt et al., 2020) (see Fig. 2 A-H for a representation of clusters identified by Witt et al. (2020)). A similar approach was adopted for default-mode networks, all labeled as "Default-Mode Network" (DMN).
Representation of the four clusters of areas included in executive networks found in the meta-analysis of Witt et al., 2020(Witt et al., 2020) labeled as FPN. A–B: cluster 1 (cyan), dorsal and lateral view. C–D: cluster 2 (green), dorsal and lateral view. E–F: cluster 3 (red), dorsal and frontal view. G–H: cluster 4 (purple), dorsal and lateral view. MFG: middle frontal gyrus; SPL: superior parietal lobule; medFG: medial frontal gyrus; IPL: inferior parietal lobule; SFG: superior frontal gyrus; PCun: precuneus; INS: insula; ACC: anterior cingulate cortex; MTG: middle temporal gyrus; ITG: inferior temporal gyrus; PUT: putamen; PreCG: precentral gyrus; STG: superior temporal gyrus; PCC: posterior cingulate cortexINS; CAU: caudate nucleus; THA: thalamus
Search terms: “obsessive–compulsive disorder” AND “resting state” AND “fMRI” AND “function* *connect*” AND “task-positive” OR “executive” OR “central executive” OR “executive control” OR “executive-control” OR “cognitive control” OR “attenti*” OR “dorsal attention” OR “ventral attention” OR “frontoparietal” OR “fronto-parietal” OR “default mode” AND “network*” OR “system*”.
Inclusion criteria: (1) original articles published in peer-review scientific journals; (2) human studies; (3) rs-fMRI studies investigating FC; (4) age \(\ge\) 18 years; (5) OCD diagnosis; (6) studies only including unmedicated/drug-naïve individuals (7) direct statistical comparisons between OCD patients and healthy controls (HCs).
Exclusion criteria: (1) genetic studies; (2) reviews and meta-analyses; (3) theoretical/opinion articles and conference papers; (4) presence of comorbid axis-I disorders; (5) analyses restricted to areas/networks of non-interest.
Data extraction
Data were collected through manual screening after automatic removal of duplicates (Zotero software; https://www.zotero.org/; RRID: SCR_013784). The following data were recorded: sample characteristics (sample size, age, education), clinical data (diagnosis, washout period, illness duration, symptom severity scores, statistical relationships between severity scores and functional alterations), methods for FC analyses (e.g., seed-based, whole-brain), fMRI scan procedures (e.g., instructions, scan duration).
Primary outcome measures: (1) specific network(s) (i.e., functionally interconnected brain areas associated with a specific label in literature) characterized by altered FC and the direction of effect relative to HCs, (2) specific prefrontal link/s characterized by FC alterations, its/their hemispheric distribution and direction of effects relative to HCs, (3) results of statistically-tested relationships between measures of general/specific symptom severity and FC patterns, particularly focusing on PFC alterations.
Results
A total of 222 records were initially retrieved. After removal of duplicates (n = 93) and records referring to error correction (n = 2), 127 records survived. The screening of titles and abstracts led to the further exclusion of 68 articles for the following reasons: reviews and meta-analyses (n = 14), book chapters (n = 1), commentaries (n = 1), theoretical articles (n = 1), children and/or adolescents included (n = 9), non rs-fMRI studies (n = 3), population not diagnosed with OCD (n = 38), analyzed clusters restricted to areas/networks of non-interest (n = 1). Therefore, 59 reports were assessed for eligibility and 39 studies were further excluded for the following reasons: non unmedicated/drug-naïve population (n = 28), diagnostic heterogeneity (n = 6), presence of psychiatric comorbidities (n = 6). Eventually, 20 studies were included (the selection process is illustrated in Fig. 3).
Collectively, the 20 studies included 837 HC (sample range: 19–110) and 806 OCD patients (sample range: 18–107), of which 351 were treatment-naïve and 457 treatment-free (washout period range: 2–288 weeks). Only 11 studies recruited homogeneous samples in terms of treatment (4 treatment-naïve and 7 treatment-free), whereas the remaining studies included both treatment-naïve and treatment-free patients. Symptom severity was measured by means of the Yale-Brown Obsessive Compulsive Scale (Y-BOCS (Goodman et al., 1991)) and State-Trait Anxiety Inventory (STAI (Spielberger, 1983)). Moreover, one study measured cognitive flexibility by computing the percentage of perseverative errors in a Wisconsin Card Sorting Test (Alvarez & Emory, 2006).
Concerning brain networks, 13 studies found aberrant FC of FPNs and 12 studies aberrant FC of DMN. Results concerning other networks characterized by FC alterations (SN and cortico-striato-thalamo-cortical circuit, CSTC) will be selectively discussed.
Concerning methods, 11 studies implemented a seed-based approach, 3 studies used ROI approaches, 5 studies chose a whole-brain approach (i.e., graph theory, voxel-wise global FC), 3 studies performed multivariate pattern analysis (MVPA), 1 study implemented network-based analysis, five studies performed Independent Component Analysis (ICA), 3 studies investigated effective connectivity (EC; Granger causality analysis), 2 studies assessed dynamic functional connectivity (dFC) and 1 study focused on local connectivity (fractional Amplitude of Low-Frequency Fluctuations; fALFF). Additional analyses and limitations will be selectively discussed. Collected data are reported in Tables 1, 2, and 3.
Summary of retrieved studies
Executive networks
Collectively, 13 studies found FC alterations of FPNs in OCD patients compared to HCs (Table 3). Specifically, either increased or decreased connectivity were found for functional links belonging to FPNs (Chen et al., 2018; Cheng, 2013; Cui, 2020; Fan et al., 2017; Göttlich et al., 2014; Kwak et al., 2020; Li et al., 2012; Liu et al., 2020, 2021; Luo et al., 2021; Shi et al., 2021; Shin et al., 2014; Xie et al., 2017).
Considering studies reporting increased FPN connectivity, adopting a graph-theoretical approach both intra- and inter-network (with sensory-motor network) connectivity of FPN was increased (Göttlich et al., 2014). However, the statistical threshold to derive significant connections in each network was arbitrarily selected, potentially biasing results. Additionally, a predominant enhancement of regional FC strength for FPN areas (mainly fronto-temporal) was found (Cheng, 2013). Interestingly, alterations were also reported between prefrontal areas and seeds – anterior (ACC) and posterior (PCC) cingulate cortices – known to play a role in executive control and error monitoring (Kolling et al., 2016; Leech et al., 2011; Pearson et al., 2011; Shenhav et al., 2016). Consistently, intra-network FC of right ventral FPN and inter-network FC between dorsal FPN and SN were found to be enhanced (Fan et al., 2017).
Focusing on works reporting decreased connectivity, 3 studies (Liu et al., 2020; Shi et al., 2021; Shin et al., 2014) found weakened FC of FPN. Specifically, patients were characterized by reduced intra-network and inter-network (between FPN and visual network) connectivity (Shin et al., 2014). However, FPN and DMN – kept segregated in HCs – were clustered in a single module in OCD patients, representing a potential confound. Additionally, a predominantly weakened inter-network FC with DMN and SN was found implementing a network-based approach (Shi et al., 2021). Nonetheless, such alteration is interpreted as “reduced FC”, even if OCD showed higher magnitude in negative connectivity than HCs (for whom near-zero connectivity was reported), which could be also interpreted as increased inter-network functional decoupling. As previously discussed, functional coupling and decoupling are thought to reflect different interactions between neural substrates (Fox et al., n.d.) and, therefore, should not be interpreted analogously.
Concerning studies reporting FC disruptions in both directions, either decreased inter-network FC between FPN and the SN (Chen et al., 2018) or increased intra-network FC within FPN (Cui, 2020) were reported. Interestingly, altered global FC of FPN was able to differentiate OCD patients from HCs with moderate accuracy (AUC: 0.804–0.868) (Cui, 2020). Moreover, FC was found to be weaker in OCD patients when selecting the left anterior PFC as the seed (Li et al., 2012; Xie et al., 2017), whereas it was increased when the seed was located in the right-sided homologous area (Li, et al., 2012). Nonetheless, analyses were restricted to areas showing positive FC, thus excluding potentially relevant information about decoupling.
Considering studies investigating causal relationships, both EC and FC of FPN were found to be disrupted in OCD patients (Liu et al., 2020). Specifically, EC from fronto-parietal areas to basal ganglia was weakened. Moreover, a MVPA analysis was performed to differentiate OCD patients from HCs on the basis of their FC and EC patterns. Intriguingly, classification accuracy improved when both were considered together, suggesting that the two measures capture different neurophysiological alterations characterizing OCD. Nonetheless, positive and negative correlations among time-series were considered together, introducing interpretation problems. Interestingly, Xie et al. (2017) found a reduced intra-network FC within FPN and a reduced EC from FPN to the reward circuit. This reduced EC was paralleled by an enhancement in the opposite direction (i.e., increased EC from the reward system to FPN), suggesting that the reward system may prevail over FPN in OCD.
Focusing on dFC, an increased number of transitions between 4 states characterized by different FC patterns between several networks (among which, FPN, anterior and posterior SN, dorsal and ventral DMN) was found for OCD patients (Liu et al., 2021). Such result was interpreted as evidence of a pathological hyper-active resting state, which “lowers the threshold” for falling into repetitive thinking and behaviors following seemingly irrelevant triggers. Notably, the left FPN negatively correlated with SN across all states (Supplementary material (Liu et al., 2021)), suggesting that FC between such networks is stable at rest, regardless of dynamic rearrangements of FC patterns. OCD patients were also found to spend more time in a highly modular dynamic state characterized, among other features, by decreased FC between DMN and FPN (Luo et al., 2021). Notably, results were consistent across participants with different medication use histories (unmedicated versus drug-naïve) and across different time-window lengths (44 s versus 60 s).
Lastly, altered FC patterns at baseline within FPN and between the latter and DMN were found to be useful for differentiating OCD patients from HCs, and for classifying OCD patients on the basis of their responsiveness to treatment, as non-responders had altered inter-network FC pattern between FPN and DMN, a pattern not present in responders (Kwak et al., 2020).
Default-mode network
Collectively, 12 studies reported functional alterations of DMN (Table 3). Both intra- and inter-network FC of DMN were predominantly weakened (Chen et al., 2018; Cheng, 2013; Cui, 2020; Göttlich et al., 2014; Jang et al., 2010; Shin et al., 2014). Nonetheless, some studies also reported enhanced FC (Fan et al., 2017; Hou, 2013; Luo et al., 2021; Shi et al., 2021; Ye et al., 2021). Moreover, FC alterations of DMN were useful for differentiating OCD patients from HCs (Cui, 2020; Kwak et al., 2020) and for classifying different OCD subgroups (Kwak et al., 2020).
Focusing on studies reporting weakened FC, a reduced intra- and inter-network FC within DMN and between the DMN and a limbic module was found, respectively (Göttlich et al., 2014)). Similarly, node strength (i.e., sum of the connectivity weights of all the edges attached to a node) of regions belonging to DMN was reduced in OCD patients (Shin et al., 2014). Consistently, regional FC within the ICA-derived module corresponding to DMN was found to be weakened (Cheng, 2013). Interestingly, links within DMN characterized by reduced global FC were also useful for differentiating OCD patients from HCs (Cui, 2020). Besides, FC of the PCC – a core DMN region – with other DMN regions was found to be reduced in OCD patients (Jang et al., 2010). Finally, Shi et al. (2021) also found reduced FC within DMN, as well as between the latter, SN and right FPN. However, the sample was extremely heterogeneous in terms of washout period (9–676 weeks) and OCD patients were mainly characterized by negative connectivity compared to HCs.
Concerning findings about enhanced connectivity, intra-network FC within DMN (Cheng, 2013) and anterior DMN (Fan et al., 2017) and inter-network FC between the superior-posterior DMN and SN (Fan et al., 2017) were increased. Notably, the same DMN-SN connectivity was also reported to be weakened in another study (Chen et al., 2018). However, Chen and colleagues (Chen et al., 2018) considered different DMN subregions altogether – while they were separately investigated by Fan and colleagues (Fan et al., 2017) – thus, results are only partially comparable. Finally, an increased inter-network FC between DMN and right cerebellum (lobule VI, belonging to FPN) was found with a seed-based approach (Murayama, 2021). Unfortunately, such result did not survive correction for multiple comparisons. Notably, cerebellar seeds were selected from a previous study conducted on both OCD and HCs (Xu et al., 2019) and then assigned to different networks based on other studies conducted on HCs. Such approach might have introduced unaccounted variability, eventually leading to null results.
Furthermore, three studies reported the simultaneous presence of functional coupling and decoupling between regions belonging to DMN (Cheng, 2013; Hou, 2013; Ye et al., 2021). Nonetheless, Hou and colleagues (Hou, 2013) aimed at investigating structural–functional coupling, thus structurally abnormal regions were used as seeds, potentially biasing the results. Contrarily, Ye et al. (2021) functionally segregated the precuneus (PCun) – one the main DMN hubs characterized by functional heterogeneity – in order to improve the sensitivity in detecting FC alterations. Indeed, by implementing a data-driven approach (i.e., functional parcellation and functional modular analysis), either reduced or increased FC was found between ventral, anterior and posterior PCun and other regions (see Table 3 for a complete list). Nonetheless, some results did not survive stricter statistical thresholding (i.e., PCun-vermis connectivity). Moreover, only two between-group differences in FC between PCun and 10 cortical and cerebellar modules were at the margin of statistical significance (i.e., posterior PCun with superior and middle posterior cerebellar lobe; p = 0.05 and p = 0.06, respectively (Ye et al., 2021)). Nonetheless, such findings suggest that the functional heterogeneity of the PCun must be accounted for in order to improve sensitivity, also given that all the significant results disappeared or were reduced in significance when the whole PCun was considered in a validation analysis. Lastly, Cheng and colleagues (Cheng, 2013) found bidirectional alterations of regional FC for regions – mainly including midline prefrontal areas – belonging to the DMN.
Interestingly, implementing a multivariate approach, inter- and intra-network FC of DMN were found to be useful for differentiating OCD patients from HC (Cui, 2020; Kwak et al., 2020), as well as for classifying different OCD subgroups according to their responsiveness to treatment (Kwak, et al., 2020). Specifically, responders were characterized by a specific FC pattern between DMN and both visual and auditory networks, whereas non-responders were characterized by a broader pattern of altered FC including, among others, intra- (DMN) and inter-network (between DMN and FPN) links (Kwak et al., 2020). Still, being pharmacological and psychotherapeutic treatments administered together, it is impossible to disentangle responsiveness univocally associated with either intervention. Further, great heterogeneity in terms of type of medication and dosage might have introduced unaccountable variability.
Concerning dFC, ventral and dorsal DMN were among networks whose connectivity described different dynamic states (discussed above) (Liu et al., 2021). Specifically, OCD patients were characterized by an increased number of state transitions, suggesting that FC of several DMN subregions – along with other networks – may contribute to determine a highly dynamic neurofunctional environment wired to promptly respond to external triggers. Nonetheless, although in each state both positive and negative FC patterns were found between DMN and other networks, the dorsal DMN negatively correlated with posterior SN, while the ventral DMN negatively correlated with anterior SN in a systematic way, across all states. Such a stable pattern suggests that FC between these networks is intrinsically stable and contributes less to state transitions.
Interestingly, a methodologically similar study found that OCD patients spent an increased fractional time in a state characterized by enhanced FC within DMN and functional decoupling between DMN, SN and FPN (Luo et al., 2021). Moreover, topological analyses revealed that the PCun was characterized by reduced variability of degree centrality (i.e., a graph-theory index measuring how much a node is functionally connected with other nodes of the network) and of nodal efficiency (i.e., the ability of a node to propagate information to other nodes in a network in parallel; see Supplementary material (Luo et al., 2021)) in OCD. These results are interpreted as abnormal functional segregation, reduced ability to shift outside a default-mode state, and decreased ability of PCun to exchange information, possibly underlying the experience of “being stuck” into thoughts or behaviors.
Finally, enhanced reciprocal causal influences – both inhibitory and excitatory – between prefrontal seeds and regions (a posteriori) classified as belonging to DMN were reported only once (Li, et al., 2020).
Association between clinical scores and functional connectivity measures
Collectively, 16 studies investigated relationships between functional alterations and clinical scores (Table 2, Fig. 3). Aberrant FC of specific areas/networks correlated, either positively or negatively, with total/general severity scores (Göttlich et al., 2014; Hou, 2013; Luo et al., 2021; Shin et al., 2014; Xie et al., 2017; Ye et al., 2021), specific clinical dimensions (Jang et al., 2010; Ye et al., 2021), trait anxiety (Fan et al., 2017), and with the percentage of perseverative errors (Tomiyama et al., 2019). Notably, correlational analyses were often performed (or reported) exclusively with global severity measures, thus correlations with specific clinical dimensions might have been overlooked.
Concerning FPNs, a positive correlation between FPN intra-network connectivity and total severity scores was found (Göttlich et al., 2014). Contrarily, when nucleus accumbens (NAcc) was selected as seed, predominantly negative associations were found between FC of (mainly prefrontal) regions belonging to FPN or reward system and total severity scores (Xie et al., 2017). Instead, when PCC and ACC were chosen as seeds for their involvement in cognitive control (Kolling et al., 2016; Leech et al., 2011; Pearson et al., 2011; Shenhav et al., 2016), FC with other regions belonging to DMN correlated with symptom severity scores (PCC negatively and ACC positively, respectively). Furthermore, FC of right MFG – belonging to FPN – positively correlated with total severity scores (Cheng, 2013). Finally, increased FC between dorsal FPN and SN positively correlated with trait anxiety (Fan et al., 2017). However, being anxiety a transdiagnostic factor, this piece of evidence lacks specificity for OCD.
Moving on to DMN, aberrant FC of several regions correlated – either positively or negatively – with total severity scores (Cheng, 2013). Specifically, reduced FC of PCC with other DMN regions was associated with increased severity scores; moreover, alteration within DMN (i.e., increased FC of thalamus/ACC and reduced FC of right MFG with other DMN regions) positively correlated with clinical scores. Nonetheless, such regions had different peak coordinates than that characterized by altered FC in OCD patients (see Supplementary material (Cheng, 2013)). Similarly, associations – either positive or negative – between DMN connectivity (PCC as seed) and specific clinical dimensions (i.e., cleaning, checking, hoarding, symmetry) were found (Jang et al., 2010). Moreover, similar associations emerged when different PCun sub-regions were chosen as seeds – representing anterior and posterior DMN hubs – and implementing module-wise analyses (Ye et al., 2021). Specifically, reduced posterior PCun-vermis FC was associated with increased total and compulsion scores. The same negative association was found for anterior PCun-visual module FC and for posterior PCun-anterior cerebellar module FC. Notably, when the whole PCun was selected as seed only the latter association survived, highlighting the importance of functionally segregating the PCun. Lastly, a negative correlation between DMN intra-network connectivity and total severity scores was detected (Göttlich et al., 2014), although not surviving statistical correction for multiple comparisons.
Interestingly, 2 studies found positive correlations between cortico-subcortical FC and clinical impairments. Firstly, a consistent relationship between FC of several CSTC regions and total symptom scores was detected (Hou, 2013). Secondly, (Tomiyama et al., 2019) an association between the percentage of perseverative errors and the magnitude of FC between dorsal caudate and both anterior insula and dorsal ACC was found. Nonetheless, such FC patterns did not differ between OCD patients and HCs.
Focusing on associations between FC and symptom improvement, connectivity degree changes (follow-up versus baseline) of right ventral PFC negatively correlated with the percentage of change in total, obsession and compulsion scores (Shin et al., 2014). Nonetheless, HCs also showed significant connectivity changes at follow-up – without any treatment being administered – potentially reflecting the influence of confounds. Moreover, the extent of the negative FC at baseline between nodes mainly belonging to the right FPN and SN was able to predict total severity scores at follow-up. Specifically, patients were characterized by negative FC at baseline – unlike HCs who showed near-zero FC – and the more the negative FC at baseline, the higher the improvement at follow-up (Shi et al., 2021).
Finally, concerning dFC, total severity scores positively correlated with the number of transitions between states characterized by different FC patterns between systems including both FPNs and DMN (Liu et al., 2021).
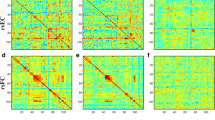
In summary (Fig. 4), total severity scores were positively related to FC alterations involving FPN, DMN, CSTC and ACC (Cheng, 2013; Göttlich et al., 2014; Hou, 2013) and to indices of dFC characterizing FPNs and DMN (Liu et al., 2021), whereas negative associations were found between total severity scores and FC of FPN, DMN, PCC and PCun (Cheng, 2013; Xie et al., 2017; Ye et al., 2021). Moreover, specific symptom dimensions correlated – either positively or negatively – with FC of DMN or PCC/PCun (Jang et al., 2010; Ye et al., 2021). Lastly, positive relationships were found for trait anxiety and cognitive inflexibility with inter-network FC alterations of FPNs and of cortico-subcortical circuits, respectively (Fan et al., 2017; Tomiyama et al., 2019).
Positive (reddish) and negative (blueish) brain-behavior relationships reported in the reviewed literature. FPN: frontoparietal network. CS: cortico-striatal network. CSTC: cortico-striatal-thalamo-cortical circuit. DMN: default-mode network. FPN: fronto-parietal network. SN: salience network. ACC: anterior cingulate cortex. PCC/PCun: posterior cingulate cortex/precuneus. Y-BOCS: Yale-Brown Obsessive–Compulsive Scale. %PE: percentage of perseverative errors. STAI-T: stait-trait anxiety inventory – trait score. TNNs: task-negative networks. TPNs: task-positive networks
Focusing on prefrontal cortex
Collectively, 18 studies reported FC alterations of links including prefrontal areas. Nonetheless, results are characterized by great inter-regional variability. Interestingly, 8 studies found significant associations between FC of PFC and clinical measures (Table 3).
Specifically, a predominant involvement of prefrontal links characterized by altered (mainly increased) FC was reported (Cheng, 2013). Interestingly, regional FC of the right middle PFC positively correlated with total severity scores. Furthermore, FC of bilateral prefrontal regions belonging to DMN was altered and correlated – either positively or negatively – with specific clinical dimensions (see Table 3) (Jang et al., 2010).
Furthermore, a widespread pattern of abnormal FC characterized by either enhanced or weakened FC between several (predominantly medial) prefrontal areas and seeds belonging to CSTC and DMN was reported (Hou, 2013). Interestingly, fronto-striatal FC (i.e., bilateral lateral and medial PFC with left and bilateral caudate, respectively) positively correlated with total symptom scores. Moreover, both increased and decreased FC between intra-hemispheric links involving PFC belonging to FPN were found (Göttlich et al., 2014).
Concerning causal influences, reduced EC from and to lateral and medial prefrontal areas was reported (Liu et al., 2020). Conversely, when EC between bilateral dorsolateral prefrontal cortex (DLPFC) and the whole brain was explored, predominantly increased inhibitory reciprocal influences between DLPFC and other prefrontal (right OFC) and temporal regions were found (Li et al., 2020). In both cases, other links involving prefrontal nodes – non overlapping (Liu et al., 2020) or only partially overlapping (Li et al., 2020) with the ones identified through EC analysis – were consistently characterized by reduced FC. Notably, the importance of DLPFC in OCD is also suggested by the positive association between FC normalization of left DLPFC and symptom relief after cognitive-behavioral therapy (Li et al., 2018).
Furthermore, FC alterations involving specific prefrontal links were extensively found, specifically: (a) increased FC of right SFG (Fan et al., 2017); (b) decreased seed-based FC between ventral PCun and left SFG (Ye et al., 2021); (c) bidirectional FC (Cui, 2020; Li et al., 2018; Xie et al., 2017) and EC (Xie et al., 2017) alterations of links including DLPFC; (d) reduced regional and long-range FC of links including bilateral ventromedial (VMPFC) (Shin et al., 2014) and ventrolateral (VLPFC) (Chen et al., 2018) prefrontal cortex, respectively; (e) either decreased or increased FC between areas connecting to anterior PFC (Li et al., 2012); and (f) decreased temporal variability of degree centrality characterizing the right MFC (Luo et al., 2021). Notably, among these alterations, only FC strength of right DLPFC, right VMPFC and left VLPFC negatively correlated with total severity scores (Xie et al., 2017). Concerning the hemispheric distribution of prefrontal links, both intra-hemispheric (Cui, 2020; Fan et al., 2017; Göttlich et al., 2014; Jang et al., 2010; Kwak et al., 2020; Shin et al., 2014) and inter-hemispheric (Chen et al., 2018; Cheng, 2013; Hou, 2013; Li et al., 2012, 2018, 2020; Liu et al., 2020; Xie et al., 2017) FC abnormalities were reported.
Moreover, 37 left-lateralized versus 33 right-lateralized links with altered FC including at least one prefrontal node were identified across studies. Interestingly, some studies found opposite FC patterns according to the hemispheric distribution of a prefrontal seed (Li et al., 2012). Specifically, FC was consistently reduced – for both inter- and intra-hemispheric connections – when the left anterior PFC was chosen as a seed. Contrarily, intra-hemispheric FC was selectively increased when the homologous right-sided region was chosen as a seed (Li et al., 2012). Finally, altered FC involving some right-lateralized prefrontal areas was useful in differentiating OCD patients from HCs, although similar bilaterally-distributed FC alterations were also able to classify patients according to their responsiveness to treatment (Kwak et al., 2020).
Discussion
Altered connectivity of executive networks
Despite the high degree of heterogeneity, a partially coherent picture emerges when FPNs were investigated. Specifically, a trend towards increased intra-network connectivity can be highlighted, with only 2 studies reporting contrasting results (Shin et al., 2014; Xie et al. 2017). Contrarily, a reduced inter-network FC between FPNs and SN, DMN, visual network, basal ganglia and a reduced EC from FPN to the reward system were found, with contrasting results only reported twice (Göttlich et al., 2014; Xie et al., 2017).
The increased intra-network FC suggests an intrinsic aberrant recruitment of cognitive control processes. Indeed, OCD is thought to be characterized by over-recruitment of cognitive control (Bucci et al., 2004; Yoshimura et al., 2019). Specifically, hyperactivity and defective downregulation of monitoring processes were extensively reported (Bucci et al., 2007; Endrass & Ullsperger, 2014; Endrass et al., 2010; Riesel et al., 2014). Consistently, enhanced indices of error detection and conflict resolution were proposed as endophenotypes of OCD (Carrasco et al., 2013; Melcher et al., 2008; Riesel et al., 2011).
Speculatively, as a working hypothesis, the over-recruitment of frontal circuits subserving monitoring might be interpreted from a Bayesian perspective and might be driven by an aberrant mismatch between predicted and actual states (Gehring et al., 2000; Pitman 1987). Indeed, hypotheses accounting for psychiatric disorders have been recently developed in the context of the Bayesian framework (Friston et al., 2011; Rao & Ballard, 1999). Concerning OCD, a decreased precision of priors representing how states evolve has been hypothesized (Fradkin et al., 2020; Fradkin et al., 2020). Specifically, the reduced reliance on action-related priors would be compensated for by an over-reliance on sensory evidence. Hence, even slight deviations from the predicted state cannot be discarded as noise and would be perceived as error signals, according to which representations are updated and the goodness of action execution is assessed.
At a phenomenological level, this would induce the experience that events are never “as expected”, giving rise to doubts, obsessions and not-just-right experiences typical of OCD. Indeed, decreased confidence on actions and related priors were found to enhance gathering behaviors (Fradkin et al., 2020; Toffolo et al., 2016). Such computational abnormality makes sensory information extremely salient and negligible variations usually registered as “noise” would produce salient prediction error signals (Fradkin et al., 2020). In this light, compulsions, checking and rituals may represent behavioral strategies implemented to reduce uncertainty (Hout et al., 2019).
This hypothesis is in line with clinical and empirical evidence, for instance: (1) unpredictability about state transitions augments gathering and checking behaviors (Parr & Friston, 2017); (2) small variations in sensory information produce error signals, inducing pathological doubts and not-just-right-experiences (Fradkin et al., 2020); (3) impaired sensory attenuation of self-generated actions, supporting the increased salience of irrelevant sensory information (Gentsch et al., 2012; Rossi et al., 2005); (4) increased uncertainty after compulsive acts (simulated data (Fradkin et al., 2020)), explaining the paradoxical effect of compulsive behaviors in boosting obsessive doubts and urgency to perform rituals (Hout et al., 2019); (5) deficits in predicting the unfolding of internal and external instances (Fradkin et al., 2019; Seli et al., 2017), possibly underlying the preference for habitual routines over planned policies (Gillan & Robbins, 2014; Gillan et al., 2014).
Concerning results about reduced FC within FPNs (Shin et al., 2014; Xie et al., 2017), these might be due to introduction of confounds, specifically: (a) the collapse of FPN and DMN in a unitary module for OCD sub-sample (Shin et al., 2014); (b) the use of an overall index of FC (i.e., average strength) as contrast measure (Xie et al., 2017), which prevents investigating the individual weights associated with specific links within the averaged network.
Concerning inter-network connectivity, results could be summarized as follows: (1) a prominently reduced connectivity between FPNs and several other networks (DMN, SN, basal ganglia, reward system and visual network); (2) a less frequently reported increased connectivity with sensory-motor circuits, SN and incoming causal influences from reward system.
Reward-related structures (e.g., dorsal ACC, basal ganglia) subserve automatic information processing and selection of habitual behaviors (Beucke et al., 2014), and also play a crucial role in performance monitoring and outcome predictions (Ullsperger et al., 2014). Thus, increased EC from reward to cognitive control systems might entail: (1) excessive reliance upon habitual – rather than planned – policies (Gillan & Robbins, 2014; Gillan et al., 2014); (2) aberrant error and conflict signaling driving an excessive engagement in monitoring processes (Milad & Rauch, 2012); and (3) increased reliance upon prediction errors driven by reward. Hence, decision-making (Hauser et al., 2017) and action selection (Vaghi et al., 2017) would be deeply undermined. Indeed, an over-recruitment of learning processes has been also reported in OCD (Hauser et al., 2017), likely reflecting the difficulty to rely on past states to predict actual outcomes (Fradkin et al., 2020).
Furthermore, the reduced FC of networks subserving executive functions with the SN might reflect a disrupted communication between the two, possibly underpinning a deficit in integrating prior representations with actual information (Menon, 2019) and/or in flexibly selecting salience-driven strategies (Gruner & Pittenger, 2017). Moreover, the SN regulates the switching between FPN and DMN (Menon, 2019; Menon & Uddin, 2010), and its reduced connectivity with both might reflect a defective switching between internally-oriented and externally-oriented information processing (Gürsel et al., 2020). Interestingly, this hypothesis is also supported by dFC studies: OCD patients spend more time in a state characterized, among other features, by negative coupling between DMN and FPNs (Luo et al., 2021) and switched more frequently between states characterized by different FC patterns (Liu et al., 2021). Such results might underlie the lack of coordination between these circuits recruited independently from the salience of contingencies and a reduced temporal stability of the whole system.
Finally, increased FC between FPN and sensory-motor network might underlie the hypothesized hyperactive action control (Bucci et al., 2004; Maltby et al., 2005). Nonetheless, several studies found inhibitory control deficits in OCD patients (Norman et al., 2019). When combined, such results may reflect the difficulty to benefit from sensory feedback to update representations (Fradkin et al., 2020), eventually leading to difficulties in inhibiting cognitive and behavioral strategies implemented to reduce uncertainty.
Reduced connectivity of default-mode network
A trend towards a reduced connectivity of DMN – both intra- and inter-network – emerged. Reduced DMN connectivity was consistently reported adopting a variety of methodological approaches. Thus, this multiverse empirical evidence is relatively immune to between-studies heterogeneities.
As DMN and executive networks are alternatively engaged (Fox & Raichle, 2007; Fox et al., n.d.), the intrinsic over-recruitment of the latter might interfere with the recruitment of DMN. Therefore, disengaging from monitoring and engaging in self-referential processes (Raichle Jul., 2015) would be hindered, if not prevented. Indeed, obsessive-compulsive indecisiveness has been associated with increased reliance on external information (Sarig et al., 2012) and inflated uncertainty about episodic memory traces (Cougle et al., 2007; Hermans et al., 2008). These phenomena might emerge from the impossibility to engage in default-mode processes (Andrews-Hanna et al., 2010; Leech & Sharp, 2014).
Crucially, it has been recently proposed that the impossibility to detach from action-perception cycles and to engage in default-mode processes might hinder the optimization of internal models through complexity reduction (Pezzulo et al., 2021). Hence, priors would remain sub-optimal high-dimensional representations, possibly hindering inferential processes (Fradkin et al., 2020). Such hypothesis is also supported by the above-discussed trend towards FPNs hyperconnectivity and the hypoconnectivity of both DMN and CEN with SN (Menon, 2019; Menon & Uddin, 2010).
Nonetheless, some studies reported either increased or decreased intra- and inter-network FC of DMN. Such inconsistency might be due to the specific DMN subdivision considered, as dissociable DMN subdivisions subserve distinct functions (Andrews-Hanna et al., 2010; Leech & Sharp, 2014; Mulders et al., 2015) alternatively engaged according to the contextual requirements (Mulders et al., 2015; Salomon et al., 2014). Indeed, when different DMN subsystems are separately investigated, an increased FC circumscribed to the anterior DMN and an increased sensitivity to detect different DMN alterations were found (Fan et al., 2017).
Interestingly, anterior DMN is involved in self-referential processes rather than in episodic memory retrieval (Leech & Sharp, 2014; Sestieri et al., 2011; Zhu et al., 2012), and its alteration has been associated with severity of ruminative thoughts (Zhu et al., 2012) and anxiety (Coutinho et al., 2016). Lastly, the consistently weakened FC of DMN might be driven by the greater robustness of posterior DMN to individual-level variations relative to anterior DMN, which makes the former more stable within and across studies (Kim & Lee, 2011).
Concerning inter-network FC, evidence points towards a reduced of DMN with: (1) SN, consistently with the hypothesized alteration in DMN-CEN switching (Fan et al., 2017); (2) limbic structures, possibly reflecting a defective modulation of the amygdala underlying a bias towards negative events and expectations (Fullana et al., 2004a, b; Göttlich et al., 2014); (3) cerebellum, possibly underlying a reduced accessibility to internal models, impairments in behavioral inhibition and cognitive flexibility (Miquel et al., 2019; Ye et al., 2021); and (4) attentional networks, potentially reflecting a reduced ability to automatically direct attention towards internal memory-based representations (Cabeza et al., 2012; Vossel et al., 2014).
Finally, bidirectional alterations within the SRN (Cheng, 2013) might reflect a deficit in re-orienting attention towards the internal milieu and to process self-relevant stimuli.
Relationship between connectivity patterns and clinical scores
Significant relationships between FC and clinical measures emerged. Specifically, executive networks FC has been predominantly positively associated with total severity scores, in line with evidence about hyper-responsiveness of cognitive control and monitoring systems at the basis of OCD manifestations (Bucci et al., 2004; Bucci et al., 2007; Endrass & Ullsperger, 2014; Endrass et al., 2010; Maltby et al., 2005; Riesel et al., 2014; Yoshimura et al., 2019). Nonetheless, relationships in the opposite direction (Xie et al., 2017) might challenge this assumption. However, in this study (Xie et al., 2017) FPN was defined as regions showing negative relationships with the NAcc. Notably, hypotheses about systematic negative associations between executive regions and NAcc contrasts with evidence about significant interactions between NAcc and lateral PFC (Arco & Mora, 2008; Luís et al., 2017). This might have led to including areas not typically or exclusively related to executive control (i.e., bilateral PCun, IPL – also part of the DMN (Broyd et al., 2009) – and fusiform face area (Xie et al., 2017)) and to excluding regions typically involved in executive processing (e.g., frontopolar cortex, ACC and OFC (Cole & Schneider, 2007; Niendam et al., 2012)).
Interestingly, reduced FC of DMN was consistently associated with higher total and specific severity scores. This finding is in line with the hypothesized DMN dysconnectivity as core neurophysiological correlate of severity across symptom dimensions, possibly reflecting the above-discussed deficit in self-referential processing and episodic memory retrieval (Andrews-Hanna et al., 2010; Leech & Sharp, 2014; Raichle, 2015; Sestieri et al., 2011).
Moreover, the functional fractionability of anterior and posterior DMN outlined above is also supported by correlational analyses, as the two were differentially associated with specific clinical dimensions. Notably, a partially consistent pattern emerged when considering total severity scores (i.e., positive and negative associations with anterior and posterior DMN, respectively). This further supports the selective involvement of anterior DMN in defective emotional processing of self-relevant stimuli (Leech & Sharp, 2014; Zhu et al., 2012), also substantiated by the positive association between FC of SRN and total severity scores.
Considering the relationship between increased FC of CSTC and reduced cognitive flexibility (Tomiyama et al., 2019), orbitofrontal and striatal components belonging to CSTC are thought to code hidden state transitions (Nassar et al., 2019) and to coordinate the selection of habitual versus goal-directed actions (Graybiel & Grafton, 2015; Parr & Friston, 2018). Therefore, this association might reflect a deficit in computing and representing state transitions, possibly exacerbating the need to gather sensory information to reduce uncertainty (specific for OCD and not found in other anxiety-related disorders; (Toffolo et al., 2016)). In turn, this would prompt the selection of automatic and rigid policies at the expenses of more flexible responses.
Concerning dFC, the positive association between number of state transitions and total severity scores might reflect a temporal instability of the whole system and an intrinsic predisposition to frequently rearrange FC patterns, potentially accounting for OCD manifestations. Such instability might underlie a pathologically hyper-responsive state possibly driven by an increased sensitivity to environmental changes (Fradkin et al., 2020) which, in turn, could explain the intrusiveness and the urgency to perform specific actions (Liu et al., 2021).
Prefrontal cortex connectivity
Several studies reported FC alterations of prefrontal nodes. However, results highly heterogeneous – across- but also within-studies – in terms of hemispheric distribution, specific regions/links altered and direction of alterations.
Specifically, no clear asymmetric pattern emerged. Nonetheless, when focusing on long-range alterations between specific nodes (see Figs. 5, 6, and 7; visualized via BrainNet Viewer; (Xia et al., 2013); http://www.nitrc.org/projects/bnv/; RRID: SCR_009446), a predominantly increased FC for right-lateralized prefrontal links emerged (Fig. 6). Contrarily, results about left-lateralized (Fig. 5) and inter-hemispheric (Fig. 7) links were inconsistent.
Left-lateralized intra-hemispheric links involving prefrontal areas and reported to be altered across studies. (A): lateral view. (B): dorsal view. Red lines: links characterized by increased FC. Blue lines: links characterized by decreased FC. Node size approximately represents the number of times that a specific node is reported in the reviewed literature. ACC: anterior cingulate cortex. AMY: amygdala. ANG: angular gyrus. CAU: caudate nucleus. DLPFC: dorsolateral prefrontal cortex. FFG: fusiform gyrus. Fpole: frontal pole. IFG: inferior frontal gyrus. INS: insula. ITG: inferior temporal gyrus. medFG: medial frontal gyrus. medOFC: medial orbitofrontal cortex. MFG: middle frontal gyrus. MOG: middle occipital gyrus. OFC: orbitofrontal cortex. Par: parietal cortex. PCC: posterior cingulate cortex. PoCG: postcentral gyrus. PUT: putamen. SFG: superior frontal gyrus. STG: superior temporal gyrus
Right-lateralized intra-hemispheric links involving prefrontal areas and reported to be altered across studies. (A): lateral view. (B): dorsal view. Red lines: links characterized by increased FC. Blue lines: links characterized by decreased FC. Node size: number of times that a specific node is reported in the reviewed literature. CAU: caudate nucleus. DLPFC: dorsolateral prefrontal cortex. Fpole: frontal pole. IFG: inferior frontal gyrus. IFGorbit: inferior frontal gyrus pars orbitalis. INS: insula. ITG: inferior temporal gyrus. LinG: lingual gyrus. medFG: medial frontal gyrus. medOFG: medial orbitofrontal gyrus. midCC: middle cingulate cortex. OFC: orbitofrontal cortex. PCC: posterior cingulate cortex. PCun: precuneus. PUT: putamen. SFG: superior frontal gyrus
Inter-hemispheric links involving prefrontal areas and reported to be altered across studies. (A): frontal view. (B): dorsal view. Red lines: links characterized by increased FC. Blue lines: links characterized by decreased FC. Node size: number of times that a specific node is reported in the reviewed literature. ACC: anterior cingulate cortex. CAU: caudate nucleus. Cer: cerebellum. DLPFC: dorsolateral prefrontal cortex. FFG: fusiform gyrus. Fpole: frontal pole. IFG: inferior frontal gyrus. INS: insula. ITG: inferior temporal gyrus. MFG: middle frontal gyrus. MOG: middle occipital gyrus. mSFG: medial superior frontal gyrus. OFC: orbitofrontal cortex. PCC: posterior cingulate cortex. PoCG: postcentral gyrus. PreCG: precentral gyrus. PUT: putamen. SFG: superior frontal gyrus. SMA: supplementary motor area. STG: superior temporal gyrus. VLPFC: ventrolateral prefrontal cortex
The right-lateralized hyperconnectivity supports the hypothesized hyperactive monitoring in OCD (Bucci et al., 2004; Endrass & Ullsperger, 2014; Endrass et al., 2010; Maltby et al., 2005; Riesel et al., 2014; Yoshimura et al., 2019). Indeed, right lateral PFC subserves monitoring, reality checking and hypothesis evaluation (Coltheart, 2010), aimed at updating representations to optimize behavior (Shallice, 2008; Stuss et al., 1995; Stuss, 2011; Vallesi, 2020). Moreover, links included lateral prefrontal areas, consistently with the ROBBIA model (Stuss et al., 1995; Stuss, 2011; Vallesi, 2020). Intriguingly, when homologous prefrontal seeds were chosen (Li et al., 2012), FC was selectively increased only with the right-lateralized seed. This result further suggests that right-sided functions might pathologically prevail over left-lateralized ones in OCD.
Furthermore, the majority of right prefrontal regions showed increased FC with posterior regions (mainly PCC and striatum) whereas a weakened FC is mostly observed for right-lateralized links connecting prefrontal regions among each other. Besides, the predominantly enhanced FC of prefrontal areas with cingulate (PCC and ACC) and striatal cortices is observed regardless of the hemispheric distribution. Moreover, fronto-striatal hyperconnectivity is particularly marked for left-lateralized links (Fig. 5). Finally, the DLPFC – especially the right-lateralized node – is the prefrontal component more consistently found to be altered across studies.
Fronto-posterior hyperconnectivity
The PCC is a core region of the (posterior) DMN (Andrews-Hanna et al., 2010; Mulders et al., 2015) and, among other functions (Leech & Sharp, 2014), it sustains vigilance (Hahn et al., 2007) and controls the balance between externally- and internally-oriented information processing (Mesulam, 1998). Moreover, the PCC signals the occurrence of behaviorally-relevant information (Pearson et al., 2011). Interestingly, its hyperactivity and hyperconnectivity were associated with intrusion of internal instances during performance (Sonuga-Barke & Castellanos, 2007; Weissman et al., 2006) detection of unpredictable stimuli (Hahn et al., 2007) and increased preparedness to external stimulation (Hampson et al., 2006). Therefore, its hyperconnectivity with PFC might underpin the facilitation of externally-oriented – at the detriment of self-oriented – information processing, possibly modulating or being modulated by attentional and executive processes (Bucci et al., 2004; Endrass & Ullsperger, 2014; Endrass et al., 2010; Maltby et al., 2005; Riesel et al., 2014; Yoshimura et al., 2019).
Fronto-striatal hyperconnectivity
Fronto-striatal dysfunctions are hypothesized to underpin OCD manifestations (Pauls et al., 2014; Saxena & Rauch, 2000). Indeed, cortico-striatal hyperconnectivity was found in OCD patients at rest and during the administration of symptom-provoking stimuli (Anticevic et al., 2014; Cocchi et al., 2012; Figee et al., 2013; Harrison et al., 2009). Moreover, symptom improvement was observed after normalization of cortico-striatal hyperconnectivity (Dunlop et al., 2016; Figee et al., 2013). Consistently, such result might reflect a facilitation of routine schemata versus goal-directed behaviors, leading to cognitive and behavioral inflexibility (Gillan et al., 2014; Gillan et al., 2014). Notably, the PFC is thought to encode representations about state transitions (Nassar et al., 2019) guiding the selection of behaviors according to contingencies (Graybiel & Grafton, 2015; Parr & Friston, 2018). Hence, fronto-striatal hyperconnectivity might reflect the need to rely on rigid habits for minimizing error signals and improving inferential processes in presence of imprecise priors. Indeed, habits are “Bayesian-optimal actions”, given their ability to reduce uncertainty (Fradkin et al., 2020).
Fronto-frontal alterations and DLPFC
The interplay between functionally-segregated prefrontal regions subserving different control functions (Carlén, 2017) might be disrupted in OCD, contributing to outline a heterogeneous clinical picture (Snyder et al., 2015). For instance, the VMPFC predicts action-related outcomes and represents information about their subjective value (Alexander & Brown, 2011; Euston et al., 2012), whereas the lateral OFC encodes biologically-relevant representations of internal goals (Behrens et al., 2018; Parr et al., 2020; Schuck et al., 2016). Therefore, hypoconnectivity between those regions might reflect an intrinsic neural inefficiency in predicting action outcomes and in assigning appropriate value to them. Moreover, the dorsomedial PFC subserves conflict detection, working in concert with lateral PFC implementing behavioral adjustments for conflict resolution (Botvinick et al., n.d.; MacDonald et al., 2000; Pellegrino et al., 2007), therefore FC alterations between these regions might underlie synchronization abnormalities, possibly hindering conflict resolution and performance optimization.
Finally, right DLPFC connectivity alterations are consistent with the excessive engagement in monitoring processes in OCD (Bucci et al., 2007; Endrass & Ullsperger, 2014; Endrass et al., 2010; Yoshimura et al., 2019). Indeed, the right DLPFC subserves domain-general monitoring processes and is involved in low-confidence decision-making, where uncertainty plays a major role (Fleck, 2005; Vallesi, 2020). Moreover, its intrinsic lateralization predicts monitoring performance across several task domains (Ambrosini et al., 2020). Therefore, its altered connectivity might underpin the hypothesized monitoring deficits entailing OCD manifestations.
Inter-hemispheric alterations
The broad inter-hemispheric pattern of aberrant FC – although inconsistent in terms of directionality – might underpin a defective interplay between right- and left-sided neurofunctional substrates subserving criterion-setting and monitoring (Ambrosini et al., 2019; Vallesi, 2020). Specifically, their defective cooperation might entail a constant updating of internal models, possibly driven by uncertainty and increased salience of sensory information (Fradkin et al., 2020; Parr & Friston, 2018).
Relationship between prefrontal connectivity and clinical measures
Reported associations between PFC connectivity and clinical measures support the predicted importance of PFC to obsessive–compulsive manifestations above and beyond their role in executive dysfunctions but with a due caveat for correlational evidence. Results highlight a predominant involvement of lateral PFC and a slight trend towards positive associations, supporting the over-recruitment of cognitive control at the basis of OCD (Bucci et al., 2007; Endrass & Ullsperger, 2014; Endrass et al., 2010; Maltby et al., 2005; Yoshimura et al., 2019).
For instance, bilateral DLPFC was found to be related to a variety of clinical scores in several studies. Interestingly, the MFC is in an intermediate position along a caudo-rostral axis characterized by a progressively increasing gradient of abstraction (Nee & D’Esposito, 2016, 2017). In particular, mid-lateral prefrontal areas integrate external/present-oriented with internal/future-oriented contingencies, enhancing inter-network interactions during contextual control (Nee, 2021). Therefore, the inefficient integration of external contingencies with future-oriented goals might also underlie OCD manifestations.
Nonetheless, since the direction of alterations is highly inconsistent, future experimental studies aimed at further characterizing the role of PFC will be essential to clarify the picture.
Limitations
A first limit concerns the variability characterizing reported results. Thus, potential sources of heterogeneity – within- and across-studies – must be discussed.
Firstly, the majority of studies recruited a mixed population in terms of treatment (i.e., unmedicated and drug-naïve patients often considered together). Moreover, the washout period range was considerably wide across studies (2–288 weeks). Notably, in most cases these confounds were not accounted for either during the selection process or in the analyses. Thus, either short- or long-term effects of medications might have unpredictably affected functional measures. Additionally, patients were not differentiated according to their scores in specific clinical dimensions, hindering the identification of neurophysiological substrates associated with specific clinical phenotypes. Furthermore, the presence of axis-I comorbidities was often not assessed and the diagnosis was sometimes accepted regardless of the concomitant presence of high anxiety and depression. Such variables, as well as illness duration, were often not included as covariates.
Concerning scanning procedures, a substantial variability can be highlighted in terms of instructions (eyes-opening), presence/absence of expedients to evaluate consciousness (eye-tracking) and scanning duration (4–14 min). Such variability can deeply influence results, hindering reliability and replicability of FC findings (Dijk et al., 2010; Patriat et al., 2013).
Focusing on data-analysis, a great variability in the methods implemented to compute FC might have affected results. Indeed, methods are characterized by different parameters, investigate different neural properties and exploit a priori assumptions to different extents (for reviews, see (Chen et al., 2020; Smitha et al., 2017)). Notably, contrasting results emerge when a dataset is analyzed with different methods (Smith et al., 2011). Thus, multiverse analysis approaches are desirable in the future also for this field.
Moreover, comparison problems also emerge when implementing the same approach with different parameters or theoretical assumptions, for instance: hypothesis-driven or data-driven ROI/seed(s) selection; clustering and parcellation procedures; arbitrariness in the number of independent components to be extracted (Cole, 2010); topological stability of brain networks, especially when different masks are used (Oliver et al., 2019), redundancy of labels for overlapping circuits (Witt et al., 2020); choice to regress out global signal or not (Murphy & Fox, 2017).
Regarding functional asymmetries, none of the studies performed a pairwise statistical comparison between homologous regions, representing a prerequisite to infer lateralization (Nieuwenhuis et al., 2011). Therefore, asymmetries discussed here must be considered solely for their exploratory and hypothesis-generating value.
Finally, the choice to consider only resting-state studies might have inflated positive results concerning DMN. In turn, the relative contribution of FPNs in OCD might have been underestimated.
In order to provide an overview of the quality of the single studies included in the present review, we used an adapted version of the Newcastle-Ottawa Quality assessment scale (NOS) for case-control studies (Peterson et al., 2011), whose results are shown in Table 4. Overall, included studies suffer from risk of bias mainly due to selection procedures. Moreover, not all studies statistically controlled for potential important confounding factors. Indeed, only a few studies can be rated as "high quality" according to our assessment. On the other hand, almost all studies performed statistical correction for multiple comparisons. Therefore, reported results are reliable in most cases, at least from a purely statistical viewpoint. Nonetheless, as discussed above, methodological heterogeneity across studies might have prevented the identification of stable FC patterns associated with OCD and related clinical manifestations.
Conclusions
The present review highlighted the presence of FC alterations of FPNs and DMN in OCD. A trend towards increased intra-network and decreased inter-network FC for FPNs emerged, sometimes positively associated with clinical measures. Moreover, a consistently reduced intra-and inter-network connectivity of DMN was reported, often negatively associated with clinical measures. Besides, a predominant (right-sided) hyperconnectivity of fronto-posterior and fronto-striatal links emerged, along with a predominant hypoconnectivity of fronto-frontal links. Finally, several brain-behavior relationships often including FC alterations of lateral prefrontal links were found, although often inconsistent in terms of direction.
Such results suggest (i) an over-recruitment of cognitive control and monitoring functions, possibly intended to (fruitlessly) reduce uncertainty; (ii) the impossibility to disengage from action-perception cycles and to adaptively switch between systems subserving internally- versus externally-oriented processing; (iii) the disintegration of self-reflective processes, possibly driven by an aberrant salience of environmental information. Such abnormalities might lead to a defective optimization of internal models, eventually affecting inferential processes and leading to obsessive-compulsive manifestations.
In spite of its limitations, our work provides an overview of relevant findings concerning intrinsic functional abnormalities characterizing brain networks in OCD. Neurofunctional alterations and their relationship with clinical measures were highlighted and interpreted at different levels of analysis, also within the Bayesian brain framework, pinpointing relevant considerations for future research. Specifically, future studies should focus on harmonizing methodology, especially concerning sampling strategy, pre-processing steps and procedures for extracting networks of interest. Moreover, the relationship between FC alterations and cognitive functions known to be altered in OCD and potentially accounting for some clinical manifestations needs to be further explored. Finally, it might be relevant investigating the role of inferential processes in OCD and the existence of a link between abnormalities in such processes, FC alterations and clinical manifestations. A feasible approach might include the administration of tasks optimized for investigating inferential processes subserving cognitive control, along with the implementation of computational models aimed at identifying inter-individual differences in how and how efficiently the underlying causes of sensory events are estimated (e.g., Hierarchical Gaussian Filter, (Mathys et al., 2011, 2014)).
Data availability
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.
Abbreviations
- %PE:
-
Percentage of perseverative errors
- ACC:
-
Anterior cingulate cortex
- AI:
-
Anterior insula
- AL:
-
Anterior (cerebellar) lobe
- ALFF:
-
Amplitude of low-frequency fluctuations
- AMY:
-
Amygdala
- AN:
-
Auditory network
- ANG:
-
Angular gyrus
- antDMN:
-
Anterior default-mode network
- antSFG:
-
Anterior superior frontal gyrus
- A-PCun:
-
Anterior precuneus
- AUC:
-
Area under the curve
- BG:
-
Basal ganglia
- BOLD:
-
Blood oxygen level-dependent
- CAU:
-
Caudate
- Cer:
-
Cerebellum
- CSTC:
-
Cortico-striatal-thalamic circuit
- dACC:
-
Dorsal anterior cingulate cortex
- DAN:
-
Dorsal attention network
- DA-PCun:
-
Dorsal anterior precuneus
- dFC:
-
Dynamic functional connectivity
- dFPN:
-
Dorsal fronto-parietal network
- DLPFC:
-
Dorsolateral prefrontal cortex
- dlSFG:
-
Dorsolateral superior frontal gyrus
- DMN:
-
Default-mode network
- DMPFC:
-
Dorsomedial prefrontal cortex
- DP-PCun:
-
Dorsal posterior precuneus
- EC:
-
Effective connectivity
- fALFF:
-
Fractional amplitude of low-frequency. fluctuations
- FC:
-
Functional connectivity
- FFG:
-
Fusiform gyrus
- fMRI:
-
Functional magnetic resonance imaging
- FPN:
-
Fronto-parietal network
- Fpole:
-
Frontal pole
- GFC:
-
Global functional connectivity
- GICA:
-
Group independent component analysis
- HC:
-
Healthy controls
- IC:
-
Independent component
- ICA:
-
Independent component analysis
- IFG:
-
Inferior frontal gyrus
- IFGoperc:
-
Inferior frontal gyrus – pars opercularis
- IFGorbit:
-
Inferior frontal gyrus – pars orbitalis
- IFGtriang:
-
Inferior frontal gyrus – pars triangularis
- INS:
-
Insula
- ITG:
-
Inferior temporal gyrus
- LAN:
-
Language network
- LIM:
-
Limbic network
- LinG:
-
Lingual gyrus
- medFC:
-
Medial frontal gyrus
- medOFC:
-
Medial orbitofrontal cortex
- medSFG:
-
Medial superior frontal gyrus
- MFG:
-
Middle frontal gyrus
- MFGorbit:
-
Medial frontal gyrus – pars orbitalis
- MFGorbit:
-
Middle frontal gyrus – pars orbitalis
- midCC:
-
Middle cingulate cortex
- ModCon:
-
Modular connectivity
- MOG:
-
Middle orbital gyrus
- MVPA:
-
Multivariate pattern analysis
- NAcc:
-
Nucleus accumbens
- NBA:
-
Network-based analysis
- OCD:
-
Obsessive-compulsive disorder
- OCD_NR:
-
Patients non-responding to medications
- OCD_R:
-
Patients responding to medications
- OFC:
-
Orbitofrontal cortex
- PCC:
-
Posterior cingulate cortex
- PCun:
-
Precuneus
- PFC:
-
Prefrontal cortex
- PoCG:
-
Postcentral gyrus
- postDMN:
-
Posterior default-mode network
- PreCG:
-
Precentral gyrus
- PUT:
-
Putamen
- ReCD:
-
Regional connectivity degree
- ReHo:
-
Regional homogeneity
- ROC:
-
Receiver operating characteristic
- ROI:
-
Region of interest
- rs-fMRI:
-
Resting-state functional magnetic resonance imaging
- rvFPN:
-
Right ventral fronto-parietal network
- SFG:
-
Superior frontal gyrus
- SFGorbit:
-
Superior frontal gyrus – pars orbitalis
- SMA:
-
Supplementary motor area
- SMN:
-
Sensory-motor network
- SN:
-
Salience network
- SPL:
-
Superior parietal lobe
- STAI-T:
-
State-trait anxiety inventory – trait
- STG:
-
Superior temporal gyrus
- TPole:
-
Temporal pole
- VLPFC:
-
Ventrolateral prefrontal cortex
- VMPFC:
-
Ventromedial prefrontal cortex
- VN:
-
Visual network
- V-PCun:
-
Ventral precuneus
- Y-BOCS:
-
Yale-Brown Obsessive-Compulsive Scale
References
Abramovitch, A., McCormack, B., Brunner, D., Johnson, M., & Wofford, N. (2019). The impact of symptom severity on cognitive function in obsessive-compulsive disorder: A meta-analysis. Clinical Psychology Review, 67, 36–44. https://doi.org/10.1016/j.cpr.2018.09.003
Ahmari, S. E., & Rauch, S. L. (2022). The prefrontal cortex and OCD. Neuropsychopharmacology, 47(1), 211–224. https://doi.org/10.1038/s41386-021-01130-2
Alexander, W. H., & Brown, J. W. (2011). Medial prefrontal cortex as an action-outcome predictor. Nature Neuroscience, 14(10), 1338–1344. https://doi.org/10.1038/nn.2921
Alvarez, J. A., & Emory, E. (2006). Executive function and the frontal lobes: A meta-analytic review. Neuropsychology Review, 16(1), 17–42. https://doi.org/10.1007/s11065-006-9002-x
Ambrosini, E., Arbula, S., Rossato, C., Pacella, V., & Vallesi, A. (2019). Neuro-cognitive architecture of executive functions: A latent variable analysis. Cortex, 119, 441–456. https://doi.org/10.1016/j.cortex.2019.07.013
Ambrosini, E., Capizzi, M., Arbula, S., & Vallesi, A. (2020). Right-lateralized intrinsic brain dynamics predict monitoring abilities. Cognitive, Affective, & Behavioral Neuroscience, 20(2), 294–308. https://doi.org/10.3758/s13415-020-00769-6
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5 (5th ed.). Autor.
Andrews-Hanna, J. R., Reidler, J. S., Sepulcre, J., Poulin, R., & Buckner, R. L. (2010). Functional-anatomic fractionation of the brain’s default network. Neuron, 65(4), 550–562. https://doi.org/10.1016/j.neuron.2010.02.005
Anticevic, A., et al. (2014). Global resting-state functional magnetic resonance imaging analysis identifies frontal cortex, striatal, and cerebellar dysconnectivity in obsessive-compulsive disorder. Biological Psychiatry, 75(8), 595–605. https://doi.org/10.1016/j.biopsych.2013.10.021
Averbeck, B., & O’Doherty, J. P. (2021). Reinforcement-learning in fronto-striatal circuits. Neuropsychopharmacology. https://doi.org/10.1038/s41386-021-01108-0
Banca, P., Vestergaard, M. D., Rankov, V., Baek, K., Mitchell, S., Lapa, T., ... & Voon, V. (2015). Evidence accumulation in obsessive-compulsive disorder: the role of uncertainty and monetary reward on perceptual decision-making thresholds. Neuropsychopharmacology, 40(5), 1192-1202.
Behrens, T. E. J., et al. (2018). What is a cognitive map? Organizing knowledge for flexible behavior. Neuron, 100(2), 490–509. https://doi.org/10.1016/j.neuron.2018.10.002
Bennett, D., Bode, S., Brydevall, M., Warren, H., & Murawski, C. (2016). Intrinsic Valuation of Information in Decision Making under Uncertainty. PLOS Computational Biology, 12(7), e1005020. https://doi.org/10.1371/journal.pcbi.1005020
Beucke, J. C., et al. (2013). Abnormally high degree connectivity of the orbitofrontal cortex in obsessive-compulsive disorder. JAMA Psychiatry, 70(6), 619. https://doi.org/10.1001/jamapsychiatry.2013.173
Beucke, J. C., Sepulcre, J., Eldaief, M. C., Sebold, M., Kathmann, N., & Kaufmann, C. (2014). Default mode network subsystem alterations in obsessive–compulsive disorder. The British Journal of Psychiatry, 205(5), 376–382. https://doi.org/10.1192/bjp.bp.113.137380
Bora, E. (2020). Meta-analysis of neurocognitive deficits in unaffected relatives of obsessive-compulsive disorder (OCD): Comparison with healthy controls and patients with OCD. Psychological Medicine, 50(8), 1257–1266. https://doi.org/10.1017/S0033291720001634
Botvinick, M. M., Braver, T. S., Barch, D. M., Carter, C. S., & Cohen, J. D. (2001). Conflict monitoring and cognitive control. Psychological Review, 108(3), 624–652. https://doi.org/10.1037/0033-295X.108.3.624
Bragdon, L. B., Gibb, B. E., & Coles, M. E. (2018). Does neuropsychological performance in OCD relate to different symptoms? A meta-analysis comparing the symmetry and obsessing dimensions. Depression and Anxiety, 35(8), 761–774. https://doi.org/10.1002/da.22785
Broyd, S. J., Demanuele, C., Debener, S., Helps, S. K., James, C. J., & Sonuga-Barke, E. J. S. (2009). Default-mode brain dysfunction in mental disorders: A systematic review. Neuroscience and Biobehavioral Reviews, 33(3), 279–296. https://doi.org/10.1016/j.neubiorev.2008.09.002
Bucci, P., Mucci, A., Volpe, U., Merlotti, E., Galderisi, S., & Maj, M. (2004). Executive hypercontrol in obsessive–compulsive disorder: Electrophysiological and neuropsychological indices. Clinical Neurophysiology, 115(6), 1340–1348. https://doi.org/10.1016/j.clinph.2003.12.031
Bucci, P., et al. (2007). Neurocognitive indices of executive hypercontrol in obsessive?compulsive disorder. Acta Psychiatrica Scandinavica, 115(5), 380–387. https://doi.org/10.1111/j.1600-0447.2006.00911.x
Burguière, E., Monteiro, P., Mallet, L., Feng, G., & Graybiel, A. M. (2015). Striatal circuits, habits, and implications for obsessive–compulsive disorder. Current Opinion in Neurobiology, 30, 59–65. https://doi.org/10.1016/j.conb.2014.08.008
Cabeza, R., Ciaramelli, E., & Moscovitch, M. (2012). Cognitive contributions of the ventral parietal cortex: An integrative theoretical account. Trends in Cognitive Sciences, 16(6), 338–352. https://doi.org/10.1016/j.tics.2012.04.008
Carlén, M. (2017). What constitutes the prefrontal cortex? Science, 358(6362), 478–482.
Carrasco, M., Harbin, S. M., Nienhuis, J. K., Fitzgerald, K. D., Gehring, W. J., & Hanna, G. L. (2013). Increased error-related brain activity in youth with obsessive-compulsive disorder and unaffected siblings: Research Article: Error-Related Negativity in OCD. Depression and Anxiety, 30(1), 39–46. https://doi.org/10.1002/da.22035
Cavallaro, R., Cavedini, P., Mistretta, P., Bassi, T., Angelone, S. M., Ubbiali, A., & Bellodi, L. (2003). Basal-corticofrontal circuits in schizophrenia and obsessive-compulsive disorder: a controlled, double dissociation study. Biological psychiatry, 54(4), 437-443.
Cavedini, P., Zorzi, C., Piccinni, M., Cavallini, M. C., & Bellodi, L. (2010). Executive dysfunctions in obsessive-compulsive patients and unaffected relatives: Searching for a new intermediate phenotype. Biological Psychiatry, 67(12), 1178–1184. https://doi.org/10.1016/j.biopsych.2010.02.012
Chamberlain, S. R., Fineberg, N. A., Menzies, L. A., Blackwell, A. D., Bullmore, E. T., Robbins, T. W., & Sahakian, B. J. (2007). Impaired cognitive flexibility and motor inhibition in unaffected first-degree relatives of patients with obsessive-compulsive disorder. American Journal of Psychiatry, 164(2), 335-338.
Chen, Y.-H., et al. (2018). Decreased intrinsic functional connectivity of the salience network in drug-naïve patients with obsessive-compulsive disorder. Frontiers in Neuroscience, 12, 889. https://doi.org/10.3389/fnins.2018.00889
Chen, K., Azeez, A., Chen, D. Y., & Biswal, B. B. (2020). Resting-state functional connectivity: Signal origins and analytic methods. Neuroimaging Clinics of North America, 30(1), 15–23. https://doi.org/10.1016/j.nic.2019.09.012
Cheng, Y., et al. (2013). Abnormal resting-state activities and functional connectivities of the anterior and the posterior cortexes in medication-naïve patients with obsessive-compulsive disorder. PLoS ONE, 8(6), e67478. https://doi.org/10.1371/journal.pone.0067478
Cocchi, L., et al. (2012). Functional alterations of large-scale brain networks related to cognitive control in obsessive-compulsive disorder. Human Brain Mapping, 33(5), 1089–1106. https://doi.org/10.1002/hbm.21270
Cole, D. M., Smith, S. M., & Beckmann, C. F. (2010). Advances and pitfalls in the analysis and interpretation of resting-state FMRI data. Frontiers in systems neuroscience, 8. https://doi.org/10.3389/fnsys.2010.00008
Cole, M. W., & Schneider, W. (2007). The cognitive control network: Integrated cortical regions with dissociable functions. NeuroImage, 37(1), 343–360. https://doi.org/10.1016/j.neuroimage.2007.03.071
Coltheart, M. (2010). The neuropsychology of delusions. Annals of the New York Academy of Sciences, 1191(1), 16–26. https://doi.org/10.1111/j.1749-6632.2010.05496.x
Cougle, J. R., Salkovskis, P. M., & Wahl, K. (2007). Perception of memory ability and confidence in recollections in obsessive-compulsive checking. Journal of Anxiety Disorders, 21(1), 118–130. https://doi.org/10.1016/j.janxdis.2006.03.015
Coutinho, J. F., Fernandesl, S. V., Soares, J. M., Maia, L., Gonçalves, Ó. F., & Sampaio, A. (2016). Default mode network dissociation in depressive and anxiety states. Brain Imaging and Behavior, 10(1), 147–157. https://doi.org/10.1007/s11682-015-9375-7
Cui, G., Ou, Y., Chen, Y., Lv, D., Jia, C., Zhong, Z., ... & Li, P. (2020). Altered global brain functional connectivity in drug-naive patients with obsessive-compulsive disorder. Frontiers in Psychiatry, 11, 98. https://doi.org/10.3389/fpsyt.2020.00098
de Vries, F. E., et al. (2014). Compensatory frontoparietal activity during working memory: An endophenotype of obsessive-compulsive disorder. Biological Psychiatry, 76(11), 878–887. https://doi.org/10.1016/j.biopsych.2013.11.021
de Vries, F. E., et al. (2019). Cognitive control networks in OCD: A resting-state connectivity study in unmedicated patients with obsessive-compulsive disorder and their unaffected relatives. The World Journal of Biological Psychiatry, 20(3), 230–242. https://doi.org/10.1080/15622975.2017.1353132
Del Arco, A., & Mora, F. (2008). Prefrontal cortex–nucleus accumbens interaction: In vivo modulation by dopamine and glutamate in the prefrontal cortex. Pharmacology Biochemistry and Behavior, 90(2), 226–235. https://doi.org/10.1016/j.pbb.2008.04.011
di Pellegrino, G., Ciaramelli, E., & Làdavas, E. (2007). The regulation of cognitive control following rostral anterior cingulate cortex lesion in humans. Journal of Cognitive Neuroscience, 19(2), 275–286. https://doi.org/10.1162/jocn.2007.19.2.275
Dunlop, K., Woodside, B., Olmsted, M., Colton, P., Giacobbe, P., & Downar, J. (2016). Reductions in cortico-striatal hyperconnectivity accompany successful treatment of obsessive-compulsive disorder with dorsomedial prefrontal rTMS. Neuropsychopharmacology, 41(5), 1395–1403. https://doi.org/10.1038/npp.2015.292
Endrass, T., & Ullsperger, M. (2014). Specificity of performance monitoring changes in obsessive-compulsive disorder. Neuroscience & Biobehavioral Reviews, 46, 124–138. https://doi.org/10.1016/j.neubiorev.2014.03.024
Endrass, T., Schuermann, B., Kaufmann, C., Spielberg, R., Kniesche, R., & Kathmann, N. (2010). Performance monitoring and error significance in patients with obsessive-compulsive disorder. Biological Psychology, 84(2), 257–263. https://doi.org/10.1016/j.biopsycho.2010.02.002
Euston, D. R., Gruber, A. J., & McNaughton, B. L. (2012). The role of medial prefrontal cortex in memory and decision making. Neuron, 76(6), 1057–1070. https://doi.org/10.1016/j.neuron.2012.12.002
Fan, J., et al. (2017). Altered connectivity within and between the default mode, central executive, and salience networks in obsessive-compulsive disorder. Journal of Affective Disorders, 223, 106–114. https://doi.org/10.1016/j.jad.2017.07.041
Fenger, M. M., Gade, A., Adams, K. H., Hansen, E. S., Bolwig, T. G., & Knudsen, G. M. (2005). Cognitive deficits in obsessive–compulsive disorder on tests of frontal lobe functions. Nordic Journal of Psychiatry, 59(1), 39–44. https://doi.org/10.1080/08039480510018814
Figee, M., et al. (2013). Deep brain stimulation restores frontostriatal network activity in obsessive-compulsive disorder. Nature Neuroscience, 16(4), 386–387. https://doi.org/10.1038/nn.3344
Fleck, M. S. (2005). Role of prefrontal and anterior cingulate regions in decision-making processes shared by memory and nonmemory tasks. Cerebral Cortex, 16(11), 1623–1630. https://doi.org/10.1093/cercor/bhj097
Fox, M. D., Snyder, A. Z., Vincent, J. L., Corbetta, M., Van Essen, D. C., & Raichle, M. E. (2005). The human brain is intrinsically organized into dynamic, anticorrelated functional networks. Proceedings of the National Academy of Sciences, 102(27), 9673-9678. https://doi.org/10.1073/pnas.050413610
Fox, M. D., & Raichle, M. E. (2007). Spontaneous fluctuations in brain activity observed with functional magnetic resonance imaging. Nature Reviews Neuroscience, 8(9), 700–711. https://doi.org/10.1038/nrn2201
Fradkin, I., Eitam, B., Strauss, A. Y., & Huppert, J. D. (2019). Thoughts as unexpected intruders: Context, obsessive-compulsive symptoms, and the sense of agency over thoughts. Clinical Psychological Science, 7(1), 162–180. https://doi.org/10.1177/2167702618797102
Fradkin, I., Ludwig, C., Eldar, E., & Huppert, J. D. (2020). Doubting what you already know: Uncertainty regarding state transitions is associated with obsessive compulsive symptoms. PLOS Computational Biology, 16(2), e1007634. https://doi.org/10.1371/journal.pcbi.1007634
Fradkin, I., Adams, R. A., Parr, T., Roiser, J. P., & Huppert, J. D. (2020). Searching for an anchor in an unpredictable world: A computational model of obsessive compulsive disorder. Psychological Review, 127(5), 672–699. https://doi.org/10.1037/rev0000188
Friedman, N. P., & Robbins, T. W. (2022). The role of prefrontal cortex in cognitive control and executive function. Neuropsychopharmacology, 47(1), 72–89. https://doi.org/10.1038/s41386-021-01132-0
Friston, K., Mattout, J., & Kilner, J. (2011). Action understanding and active inference. Biological Cybernetics, 104(1–2), 137–160. https://doi.org/10.1007/s00422-011-0424-z
Fullana, M. A., et al. (2004a). High sensitivity to punishment and low impulsivity in obsessive-compulsive patients with hoarding symptoms. Psychiatry Research, 129(1), 21–27. https://doi.org/10.1016/j.psychres.2004.02.017
Fullana, M. A., et al. (2004b). Personality characteristics in obsessive-compulsive disorder and individuals with subclinical obsessive-compulsive problems. British Journal of Clinical Psychology, 43(4), 387–398. https://doi.org/10.1348/0144665042388937
Gehring, W. J., Himle, J., & Nisenson, L. G. (2000). Action-monitoring dysfunction in obsessive-compulsive disorder. Psychological Science, 11(1), 1–6. https://doi.org/10.1111/1467-9280.00206
Gentsch, A., Schütz-Bosbach, S., Endrass, T., & Kathmann, N. (2012). Dysfunctional forward model mechanisms and aberrant sense of agency in obsessive-compulsive disorder. Biological Psychiatry, 71(7), 652–659. https://doi.org/10.1016/j.biopsych.2011.12.022
Gillan, C. M., & Robbins, T. W. (2014). Goal-directed learning and obsessive–compulsive disorder. Philosophical Transactions of the Royal Society b: Biological Sciences, 369(1655), 20130475. https://doi.org/10.1098/rstb.2013.0475
Gillan, C. M., et al. (2014). Enhanced avoidance habits in obsessive-compulsive disorder. Biological Psychiatry, 75(8), 631–638. https://doi.org/10.1016/j.biopsych.2013.02.002
Goodman, W., Rasmussen, S., Price, L., Mazure, L., Heninger, G., & Charney, D. (1991). Yale-brown obsessive compulsive scale (y-BOCS). Verhaltenstherapie, 1(3), 226–233.
Göttlich, M., Krämer, U. M., Kordon, A., Hohagen, F., & Zurowski, B. (2014). Decreased limbic and increased fronto-parietal connectivity in unmedicated patients with obsessive-compulsive disorder: Altered Brain Networks in OCD. Human Brain Mapping, 35(11), 5617–5632. https://doi.org/10.1002/hbm.22574
Graybiel, A. M., & Grafton, S. T. (2015). The striatum: Where skills and habits meet. Cold Spring Harbor Perspectives in Biology, 7(8), a021691. https://doi.org/10.1101/cshperspect.a021691
Gruner, P., & Pittenger, C. (2017). Cognitive inflexibility in obsessive-compulsive disorder. Neuroscience, 345, 243–255. https://doi.org/10.1016/j.neuroscience.2016.07.030
Gürsel, D. A., Avram, M., Sorg, C., Brandl, F., & Koch, K. (2018). Frontoparietal areas link impairments of large-scale intrinsic brain networks with aberrant fronto-striatal interactions in OCD: A meta-analysis of resting-state functional connectivity. Neuroscience and Biobehavioral Reviews, 87, 151–160. https://doi.org/10.1016/j.neubiorev.2018.01.016
Gürsel, D. A., et al. (2020). Frontoparietal and salience network alterations in obsessive–compulsive disorder: Insights from independent component and sliding time window analyses. Journal of Psychiatry and Neuroscience, 45(3), 214–221. https://doi.org/10.1503/jpn.190038
Hahn, B., Ross, T. J., & Stein, E. A. (2007). Cingulate activation increases dynamically with response speed under stimulus unpredictability. Cerebral Cortex, 17(7), 1664–1671.
Hampson, M., Driesen, N. R., Skudlarski, P., Gore, J. C., & Constable, R. T. (2006). Brain connectivity related to working memory performance. Journal of Neuroscience, 26(51), 13338–13343.
Harrison, B. J., et al. (2009). Altered corticostriatal functional connectivity in obsessive-compulsive disorder. Archives of General Psychiatry, 66(11), 12.
Hauser, T. U., et al. (2017). Increased fronto-striatal reward prediction errors moderate decision making in obsessive–compulsive disorder. Psychological Medicine, 47(7), 1246–1258. https://doi.org/10.1017/S0033291716003305
Hermans, D., Engelen, U., Grouwels, L., Joos, E., Lemmens, J., & Pieters, G. (2008). Cognitive confidence in obsessive-compulsive disorder: Distrusting perception, attention and memory. Behaviour Research and Therapy, 46(1), 98–113. https://doi.org/10.1016/j.brat.2007.11.001
Hou, J., et al. (2013). Morphologic and functional connectivity alterations of corticostriatal and default mode network in treatment-naïve patients with obsessive-compulsive disorder. PloS one, 8(12), e83931. https://doi.org/10.1371/journal.pone.0083931
Jang, J. H., et al. (2010). Functional connectivity in fronto-subcortical circuitry during the resting state in obsessive-compulsive disorder. Neuroscience Letters, 474(3), 158–162. https://doi.org/10.1016/j.neulet.2010.03.031
Kashyap, H., Kumar, J. K., Kandavel, T., & Reddy, Y. C. J. (2013). Neuropsychological functioning in obsessive-compulsive disorder: Are executive functions the key deficit? Comprehensive Psychiatry, 54(5), 533–540. https://doi.org/10.1016/j.comppsych.2012.12.003
Kim, D.-Y., & Lee, J.-H. (2011). Are posterior default-mode networks more robust than anterior default-mode networks? Evidence from resting-state fMRI data analysis. Neuroscience Letters, 498(1), 57–62. https://doi.org/10.1016/j.neulet.2011.04.062
Koch, K., et al. (2018). Increased default mode network connectivity in obsessive-compulsive disorder during reward processing. Frontiers in Psychiatry, 9, 254. https://doi.org/10.3389/fpsyt.2018.00254
Kolling, N., Wittmann, M. K., Behrens, T. E. J., Boorman, E. D., Mars, R. B., & Rushworth, M. F. S. (2016). Value, search, persistence and model updating in anterior cingulate cortex. Nature Neuroscience, 19(10), 1280–1285. https://doi.org/10.1038/nn.4382
Kwak, S., Kim, M., Kim, T., Kwak, Y., Oh, S., Lho, S. K., ... & Kwon, J. S. (2020). Defining data-driven subgroups of obsessive–compulsive disorder with different treatment responses based on resting-state functional connectivity. Translational psychiatry, 10(1), 359. https://doi.org/10.1038/s41398-020-01045-4
Lacerda, A. L. T., Dalgalarrondo, P., Caetano, D., Haas, G. L., Camargo, E. E., & Keshavan, M. S. (2003). Neuropsychological performance and regional cerebral blood flow in obsessive–compulsive disorder. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 27(4), 657–665. https://doi.org/10.1016/S0278-5846(03)00076-9
Leech, R., & Sharp, D. J. (2014). The role of the posterior cingulate cortex in cognition and disease. Brain : A Journal of Neurology, 137(Pt 1), 12–32. https://doi.org/10.1093/brain/awt162
Leech, R., Kamourieh, S., Beckmann, C. F., & Sharp, D. J. (2011). Fractionating the default mode network: Distinct contributions of the ventral and dorsal posterior cingulate cortex to cognitive control. Journal of Neuroscience, 31(9), 3217–3224. https://doi.org/10.1523/JNEUROSCI.5626-10.2011
Li, P., et al. (2012). Altered resting state functional connectivity patterns of the anterior prefrontal cortex in obsessive-compulsive disorder. NeuroReport: For Rapid Communication of Neuroscience Research, 23(11), 681–686. https://doi.org/10.1097/WNR.0b013e328355a5fe
Li, P., Yang, X., Greenshaw, A. J., Li, S., Luo, J., Han, H., ... & Li, Z. (2018). The effects of cognitive behavioral therapy on resting‐state functional brain network in drug‐naive patients with obsessive–compulsive disorder. Brain and behavior, 8(5), e00963. https://doi.org/10.1002/brb3.963
Li, H. et al. (2020). Neural primacy of the dorsolateral prefrontal cortex in patients with obsessive-compulsive disorder. NeuroImage: Clinical, 28, 102432. https://doi.org/10.1016/j.nicl.2020.102432.
Liberati, A., et al. (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ, 339(jul21 1), b2700–b2700. https://doi.org/10.1136/bmj.b2700.
Liu, W., et al. (2020). Disrupted pathways from frontal-parietal cortex to basal ganglia and cerebellum in patients with unmedicated obsessive compulsive disorder as observed by whole-brain resting-state effective connectivity analysis – a small sample pilot study. Brain Imaging and Behavior. https://doi.org/10.1007/s11682-020-00333-3
Liu, J., et al. (2021). Abnormal dynamics of functional connectivity in first-episode and treatment-naive patients with obsessive–compulsive disorder. Psychiatry and Clinical Neurosciences, 75(1), 14–22. https://doi.org/10.1111/pcn.13162
Liu, J., Cao, L., Li, H., Gao, Y., Bu, X., Liang, K., ... & Gong, Q. (2022). Abnormal resting-state functional connectivity in patients with obsessive-compulsive disorder: A systematic review and meta-analysis. Neuroscience & Biobehavioral Reviews, 104574. https://doi.org/10.1016/j.neubiorev.2022.104574
Luís, C., Cannella, N., Spanagel, R., & Köhr, G. (2017). Persistent strengthening of the prefrontal cortex – nucleus accumbens pathway during incubation of cocaine-seeking behavior. Neurobiology of Learning and Memory, 138, 281–290. https://doi.org/10.1016/j.nlm.2016.10.003
Luo, L., et al. (2021). Altered brain functional network dynamics in obsessive–compulsive disorder. Human Brain Mapping, 42(7), 2061–2076. https://doi.org/10.1002/hbm.25345
MacDonald, A. W., Cohen, J. D., Stenger, V. A., & Carter, C. S. (2000). dissociating the role of the dorsolateral prefrontal and anterior cingulate cortex in cognitive control. Science, 288(5472), 1835–1838. https://doi.org/10.1126/science.288.5472.1835
Maltby, N., Tolin, D. F., Worhunsky, P., O’Keefe, T. M., & Kiehl, K. A. (2005). Dysfunctional action monitoring hyperactivates frontal–striatal circuits in obsessive–compulsive disorder: An event-related fMRI study. NeuroImage, 24(2), 495–503. https://doi.org/10.1016/j.neuroimage.2004.08.041
Martínez-Esparza, I. C., Olivares-Olivares, P. J., Rosa-Alcázar, Á., Rosa-Alcázar, A. I., & Storch, E. A. (2021). Executive functioning and clinical variables in patients with obsessive-compulsive disorder. Brain Sciences, 11(2), 267. https://doi.org/10.3390/brainsci11020267
Mataix-Cols, D., Wooderson, S., Lawrence, N., Brammer, M. J., Speckens, A., & Phillips, M. L. (2004). Distinct neural correlates of washing, checking, and hoarding symptomdimensions in obsessive-compulsive disorder. Archives of General Psychiatry, 61, 13.
Mathys, C., Daunizeau, J., Friston, K. J., & Stephan, K. E. (2011). A bayesian foundation for individual learning under uncertainty. Frontiers in Human Neuroscience, 5, 39.
Mathys, C. D., et al. (2014). Uncertainty in perception and the hierarchical gaussian filter. Frontiers in Human Neuroscience, 8, 825.
Melcher, T., Falkai, P., & Gruber, O. (2008). Functional brain abnormalities in psychiatric disorders: Neural mechanisms to detect and resolve cognitive conflict and interference. Brain Research Reviews, 59(1), 96–124. https://doi.org/10.1016/j.brainresrev.2008.06.003
Menon, V. (2011). Large-scale brain networks and psychopathology: A unifying triple network model. Trends in Cognitive Sciences, 15(10), 483–506. https://doi.org/10.1016/j.tics.2011.08.003
Menon, B. (2019). Towards a new model of understanding – The triple network, psychopathology and the structure of the mind. Medical Hypotheses, 133, 109385. https://doi.org/10.1016/j.mehy.2019.109385
Menon, V., & D’Esposito, M. (2022). The role of PFC networks in cognitive control and executive function. Neuropsychopharmacology, 47(1), 90–103. https://doi.org/10.1038/s41386-021-01152-w
Menon, V., & Uddin, L. Q. (2010). Saliency, switching, attention and control: A network model of insula function. Brain Structure and Function, 214(5–6), 655–667. https://doi.org/10.1007/s00429-010-0262-0
Mesulam, M. (1998). From sensation to cognition. Brain, 121(6), 1013–1052. https://doi.org/10.1093/brain/121.6.1013
Milad, M. R., & Rauch, S. L. (2012). Obsessive-compulsive disorder: Beyond segregated cortico-striatal pathways. Trends in Cognitive Sciences, 16(1), 43–51. https://doi.org/10.1016/j.tics.2011.11.003
Millet, B., et al. (2013). Obsessive compulsive disorder networks: Positron emission tomography and neuropsychology provide new insights. PLoS ONE, 8(1), e53241. https://doi.org/10.1371/journal.pone.0053241
Miquel, M., Nicola, S. M., Gil-Miravet, I., Guarque-Chabrera, J., & Sanchez-Hernandez, A. (2019). A working hypothesis for the role of the cerebellum in impulsivity and compulsivity. Frontiers in Behavioral Neuroscience, 13, 99. https://doi.org/10.3389/fnbeh.2019.00099
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & Group, P. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Annals of Internal Medicine, 151(4), 264–269.
Moon, C.-M., & Jeong, G.-W. (2018). Associations of neurofunctional, morphometric and metabolic abnormalities with clinical symptom severity and recognition deficit in obsessive–compulsive disorder. Journal of Affective Disorders, 227, 603–612. https://doi.org/10.1016/j.jad.2017.11.059
Mulders, P. C., van Eijndhoven, P. F., Schene, A. H., Beckmann, C. F., & Tendolkar, I. (2015). Resting-state functional connectivity in major depressive disorder: A review. Neuroscience & Biobehavioral Reviews, 56, 330–344. https://doi.org/10.1016/j.neubiorev.2015.07.014
Murayama, K., Tomiyama, H., Tsuruta, S., Ohono, A., Kang, M., Hasuzawa, S., ... & Nakao, T. (2021). Aberrant resting-state cerebellar-cerebral functional connectivity in unmedicated patients with obsessive-compulsive disorder. Frontiers in Psychiatry, 12, 659616. https://doi.org/10.3389/fpsyt.2021.659616
Murphy, K., & Fox, M. D. (2017). Towards a consensus regarding global signal regression for resting state functional connectivity MRI. NeuroImage, 154, 169–173. https://doi.org/10.1016/j.neuroimage.2016.11.052
Nassar, M. R., Bruckner, R., & Frank, M. J. (2019). Statistical context dictates the relationship between feedback-related EEG signals and learning. eLife, 8, e46975. https://doi.org/10.7554/eLife.46975
Nee, D. E. (2021). Integrative frontal-parietal dynamics supporting cognitive control. eLife, 10, e57244. https://doi.org/10.7554/eLife.57244
Nee, D. E., & D’Esposito, M. (2016). The hierarchical organization of the lateral prefrontal cortex. eLife, 5, e12112. https://doi.org/10.7554/eLife.12112
Nee, D. E., & D’Esposito, M. (2017). Causal evidence for lateral prefrontal cortex dynamics supporting cognitive control. eLife, 6, e28040. https://doi.org/10.7554/eLife.28040
Niendam, T. A., Laird, A. R., Ray, K. L., Dean, Y. M., Glahn, D. C., & Carter, C. S. (2012). Meta-analytic evidence for a superordinate cognitive control network subserving diverse executive functions. Cognitive, Affective, & Behavioral Neuroscience, 12(2), 241–268. https://doi.org/10.3758/s13415-011-0083-5
Nieuwenhuis, S., Forstmann, B. U., & Wagenmakers, E.-J. (2011). Erroneous analyses of interactions in neuroscience: A problem of significance. Nature Neuroscience, 14(9), 1105–1107. https://doi.org/10.1038/nn.2886
Norman, L. J., et al. (2019). Error processing and inhibitory control in obsessive-compulsive disorder: A meta-analysis using statistical parametric maps. Biological Psychiatry, 85(9), 713–725. https://doi.org/10.1016/j.biopsych.2018.11.010
Oliver, I., Hlinka, J., Kopal, J., & Davidsen, J. (2019). Quantifying the variability in resting-state networks. Entropy, 21(9), 882. https://doi.org/10.3390/e21090882
Papademetris, X., et al. (2006). BioImage suite: An integrated medical image analysis suite: An update. The Insight Journal, 2006, 209.
Parr, T., & Friston, K. J. (2017). Uncertainty, epistemics and active inference. Journal of the Royal Society Interface, 14(136), 20170376. https://doi.org/10.1098/rsif.2017.0376
Parr, T., & Friston, K. J. (2018). The anatomy of inference: Generative models and brain structure. Frontiers in Computational Neuroscience, 12, 90. https://doi.org/10.3389/fncom.2018.00090
Parr, T., Rikhye, R. V., Halassa, M. M., & Friston, K. J. (2020). Prefrontal computation as active inference. Cerebral Cortex, 30(2), 682–695. https://doi.org/10.1093/cercor/bhz118
Patriat, R., et al. (2013). The effect of resting condition on resting-state fMRI reliability and consistency: A comparison between resting with eyes open, closed, and fixated. NeuroImage, 78, 463–473. https://doi.org/10.1016/j.neuroimage.2013.04.013
Pauls, D. L., Abramovitch, A., Rauch, S. L., & Geller, D. A. (2014). Obsessive–compulsive disorder: An integrative genetic and neurobiological perspective. Nature Reviews Neuroscience, 15(6), 410–424. https://doi.org/10.1038/nrn3746
Pearson, J. M., Heilbronner, S. R., Barack, D. L., Hayden, B. Y., & Platt, M. L. (2011). Posterior cingulate cortex: Adapting behavior to a changing world. Trends in Cognitive Sciences, 15(4), 143–151. https://doi.org/10.1016/j.tics.2011.02.002
Pedron, A. C., Ferrão, Y. A., Gurgel, L. G., & Reppold, C. T. (2015). Relations between executive functions and different symptomatic dimensions in obsessive compulsive disorder. Paidéia (Ribeirão Preto), 25(61), 229–239. https://doi.org/10.1590/1982-43272561201511
Peterson, J., Welch, V., Losos, M., Tugwell, P., et al. (2011). The newcastle-ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa: Ottawa Hospital Research Institute, 2(1), 1–12.
Pezzulo, G., Zorzi, M., & Corbetta, M. (2021). The secret life of predictive brains: What’s spontaneous activity for? Trends in Cognitive Sciences, 25(9), 730–743. https://doi.org/10.1016/j.tics.2021.05.007
Pitman, R. K. (1987). A cybernetic model of obsessive-compulsive psychopathology. Comprehensive Psychiatry, 28(4), 334–343. https://doi.org/10.1016/0010-440X(87)90070-8
Posner, J., et al. (2017). Increased functional connectivity between the default mode and salience networks in unmedicated adults with obsessive-compulsive disorder. Human Brain Mapping, 38(2), 678–687. https://doi.org/10.1002/hbm.23408
Pushkarskaya, H., et al. (2015). Decision-making under uncertainty in obsessive–compulsive disorder. Journal of Psychiatric Research, 69, 166–173. https://doi.org/10.1016/j.jpsychires.2015.08.011
Raichle, M. E. (2015). The brain’s default mode network. Annual Review of Neuroscience, 38(1), 433–447. https://doi.org/10.1146/annurev-neuro-071013-014030
Rao, R. P. N., & Ballard, D. H. (1999). Predictive coding in the visual cortex: A functional interpretation of some extra-classical receptive-field effects. Nature Neuroscience, 2(1), 79–87. https://doi.org/10.1038/4580
Riesel, A., Endrass, T., Kaufmann, C., & Kathmann, N. (2011). Overactive error-related brain activity as a candidate endophenotype for obsessive-compulsive disorder: Evidence from unaffected first-degree relatives. American Journal of Psychiatry, 168(3), 317–324. https://doi.org/10.1176/appi.ajp.2010.10030416
Riesel, A., Kathmann, N., & Endrass, T. (2014). Overactive performance monitoring in obsessive–compulsive disorder is independent of symptom expression. European Archives of Psychiatry and Clinical Neuroscience, 264(8), 707–717. https://doi.org/10.1007/s00406-014-0499-3
Rosa-Alcázar, Á., Olivares-Olivares, P. J., Martinez-Esparza, I. C., Parada-Navas, J. L., Rosa-Alcázar, A. I., & Olivares-Rodríguez, J. (2020). Cognitive flexibility and response inhibition in patients with obsessive-compulsive disorder and generalized anxiety disorder. International Journal of Clinical and Health Psychology, 20(1), 20–28. https://doi.org/10.1016/j.ijchp.2019.07.006
Rossi, S., et al. (2005). Hypofunctioning of sensory gating mechanisms in patients with obsessive-compulsive disorder. Biological Psychiatry, 57(1), 16–20. https://doi.org/10.1016/j.biopsych.2004.09.023
Ruscio, A. M., Stein, D. J., Chiu, W. T., & Kessler, R. C. (2010). The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Molecular Psychiatry, 15(1), 53–63. https://doi.org/10.1038/mp.2008.94
Salomon, R., Levy, D. R., & Malach, R. (2014). Deconstructing the default: Cortical subdivision of the default mode/intrinsic system during self-related processing: Functional subdivision of the default network. Human Brain Mapping, 35(4), 1491–1502. https://doi.org/10.1002/hbm.22268
Sarig, S., Dar, R., & Liberman, N. (2012). Obsessive-compulsive tendencies are related to indecisiveness and reliance on feedback in a neutral color judgment task. Journal of Behavior Therapy and Experimental Psychiatry, 43(1), 692–697. https://doi.org/10.1016/j.jbtep.2011.09.012
Saxena, S., & Rauch, S. L. (2000). Functional neuroimaging and the neuroanatomy of obsessive-compulsive disorder. Psychiatric Clinics of North America, 23(3), 563–586. https://doi.org/10.1016/S0193-953X(05)70181-7
Schuck, N. W., Cai, M. B., Wilson, R. C., & Niv, Y. (2016). Human orbitofrontal cortex represents a cognitive map of state space. Neuron, 91(6), 1402–1412. https://doi.org/10.1016/j.neuron.2016.08.019
Seli, P., Risko, E. F., Purdon, C., & Smilek, D. (2017). Intrusive thoughts: Linking spontaneous mind wandering and OCD symptomatology. Psychological Research Psychologische Forschung, 81(2), 392–398. https://doi.org/10.1007/s00426-016-0756-3
Sestieri, C., Corbetta, M., Romani, G. L., & Shulman, G. L. (2011). Episodic memory retrieval, parietal cortex, and the default mode network: Functional and topographic analyses. Journal of Neuroscience, 31(12), 4407–4420. https://doi.org/10.1523/JNEUROSCI.3335-10.2011
Sha, Z., et al. (2020). Functional disruption in prefrontal-striatal network in obsessive-compulsive disorder. Psychiatry Research: Neuroimaging, 300, 111081. https://doi.org/10.1016/j.pscychresns.2020.111081
Shallice, T. (2008). Mapping task switching in frontal cortex through neuropsychological group studies. Frontiers in Neuroscience, 2(1), 79–85. https://doi.org/10.3389/neuro.01.013.2008
Shenhav, A., Cohen, J. D., & Botvinick, M. M. (2016). Dorsal anterior cingulate cortex and the value of control. Nature Neuroscience, 19(10), 1286–1291. https://doi.org/10.1038/nn.4384
Shi, T. C., Pagliaccio, D., Cyr, M., Simpson, H. B., & Marsh, R. (2021). Network-based functional connectivity predicts response to exposure therapy in unmedicated adults with obsessive–compulsive disorder. Neuropsychopharmacology, 46(5), 1035–1044. https://doi.org/10.1038/s41386-020-00929-9
Shin, D.-J., et al. (2014). The effects of pharmacological treatment on functional brain connectome in obsessive-compulsive disorder. Biological Psychiatry, 75(8), 606–614. https://doi.org/10.1016/j.biopsych.2013.09.002
Smith, S. M., et al. (2011). Network modelling methods for FMRI. NeuroImage, 54(2), 875–891. https://doi.org/10.1016/j.neuroimage.2010.08.063
Smitha, K., et al. (2017). Resting state fMRI: A review on methods in resting state connectivity analysis and resting state networks. The Neuroradiology Journal, 30(4), 305–317. https://doi.org/10.1177/1971400917697342
Snyder, H. R., Kaiser, R. H., Warren, S. L., & Heller, W. (2015). Obsessive-compulsive disorder is associated with broad impairments in executive function: A meta-analysis. Clinical Psychological Science, 3(2), 301–330. https://doi.org/10.1177/2167702614534210
Sonuga-Barke, E. J., & Castellanos, F. X. (2007). Spontaneous attentional fluctuations in impaired states and pathological conditions: A neurobiological hypothesis. Neuroscience & Biobehavioral Reviews, 31(7), 977–986.
Spielberger, C. D. (1983). State-trait anxiety inventory for adults (STAI-AD) [Database record]. APA PsycTests. https://doi.org/10.1037/t06496-000
Starcke, K., Tuschen-Caffier, B., Markowitsch, H. J., & Brand, M. (2010). Dissociation of decisions in ambiguous and risky situations in obsessive–compulsive disorder. Psychiatry Research, 175(1–2), 114–120. https://doi.org/10.1016/j.psychres.2008.10.022
Stern, E. R., Fitzgerald, K. D., Welsh, R. C., Abelson, J. L., & Taylor, S. F. (2012). Resting-state functional connectivity between fronto-parietal and default mode networks in obsessive-compulsive disorder. PloS one, 7(5), e36356. https://doi.org/10.1371/journal.pone.0036356
Stuss, D. T. (2011). Functions of the frontal lobes: Relation to executive functions. Journal of the International Neuropsychological Society, 17(5), 759–765. https://doi.org/10.1017/S1355617711000695
Stuss, D. T., Shallice, T., Alexander, M. P., & Picton, T. W. (1995). A multidisciplinary approach to anterior attentional functions. Annals of the New York Academy of Sciences, 769(1 Structure), 191–212. https://doi.org/10.1111/j.1749-6632.1995.tb38140.x.
Suhas, S., & Rao, N. (2019). Neurocognitive deficits in obsessive–compulsive disorder: A selective review. Indian Journal of Psychiatry, 61(7), 30. https://doi.org/10.4103/psychiatry.IndianJPsychiatry_517_18
Toffolo, M. B. J., van den Hout, M. A., Engelhard, I. M., Hooge, I. T. C., & Cath, D. C. (2016). Patients with obsessive-compulsive disorder check excessively in response to mild uncertainty. Behavior Therapy, 47(4), 550–559. https://doi.org/10.1016/j.beth.2016.04.002
Tomiyama, H., Nakao, T., Murayama, K., Nemoto, K., Ikari, K., Yamada, S., ... & Kanba, S. (2019). Dysfunction between dorsal caudate and salience network associated with impaired cognitive flexibility in obsessive-compulsive disorder: A resting-state fMRI study. NeuroImage: Clinical, 24, 102004. https://doi.org/10.1016/j.nicl.2019.102004.
Tükel, R., et al. (2012). Neuropsychological function in obsessive-compulsive disorder. Comprehensive Psychiatry, 53(2), 167–175. https://doi.org/10.1016/j.comppsych.2011.03.007
Ullsperger, M., Fischer, A. G., Nigbur, R., & Endrass, T. (2014). Neural mechanisms and temporal dynamics of performance monitoring. Trends in Cognitive Sciences, 18(5), 259–267. https://doi.org/10.1016/j.tics.2014.02.009
Vaghi, M. M., et al. (2017). Hypoactivation and dysconnectivity of a frontostriatal circuit during goal-directed planning as an endophenotype for obsessive-compulsive disorder. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging, 2(8), 655–663. https://doi.org/10.1016/j.bpsc.2017.05.005
Vaghi, M. M., et al. (2017). specific frontostriatal circuits for impaired cognitive flexibility and goal-directed planning in obsessive-compulsive disorder: Evidence from resting-state functional connectivity. Biological Psychiatry, 81(8), 708–717. https://doi.org/10.1016/j.biopsych.2016.08.009
Vallesi, A. (2021). The quest for hemispheric asymmetries supporting and predicting executive functioning. Journal of Cognitive Neuroscience, 33(9), 1679-1697. https://doi.org/10.1162/jocn_a_01646.
van den Hout, M. A., van Dis, E. A. M., van Woudenberg, C., & van de Groep, I. H. (2019). OCD-like checking in the lab: A meta-analysis and improvement of an experimental paradigm. Journal of Obsessive-Compulsive and Related Disorders, 20, 39–49. https://doi.org/10.1016/j.jocrd.2017.11.006
van der Straten, A. L., Denys, D., & van Wingen, G. A. (2017). Impact of treatment on resting cerebral blood flow and metabolism in obsessive compulsive disorder: A meta-analysis. Scientific Reports, 7(1), 17464. https://doi.org/10.1038/s41598-017-17593-7
Van Dijk, K. R. A., Hedden, T., Venkataraman, A., Evans, K. C., Lazar, S. W., & Buckner, R. L. (2010). Intrinsic functional connectivity as a tool for human connectomics: Theory, properties, and optimization. Journal of Neurophysiology, 103(1), 297–321. https://doi.org/10.1152/jn.00783.2009
Vossel, S., Geng, J. J., & Fink, G. R. (2014). Dorsal and ventral attention systems: Distinct neural circuits but collaborative roles. The Neuroscientist, 20(2), 150–159. https://doi.org/10.1177/1073858413494269
Wang, Z., Xin, J., Wang, Z., Yao, Y., Zhao, Y., & Qian, W. (2021). Brain functional network modeling and analysis based on fMRI: A systematic review. Cognitive Neurodynamics, 15(3), 389–403. https://doi.org/10.1007/s11571-020-09630-5
Weissman, D. H., Roberts, K., Visscher, K., & Woldorff, M. (2006). The neural bases of momentary lapses in attention. Nature Neuroscience, 9(7), 971–978.
Witt, S. T., van Ettinger-Veenstra, H., Salo, T., Riedel, M. C., & Laird, A. R. (2021). What executive function network is that? An image-based meta-analysis of network labels. Brain topography, 34(5), 598-607. https://doi.org/10.1007/s10548-021-00847-z
Xia, M., Wang, J., & He, Y. (2013). BrainNet viewer: A network visualization tool for human brain connectomics. PLoS ONE, 8(7), e68910.
Xie, C., et al. (2017). Imbalanced functional link between reward circuits and the cognitive control system in patients with obsessive-compulsive disorder. Brain Imaging and Behavior, 11(4), 1099–1109. https://doi.org/10.1007/s11682-016-9585-7
Xu, T., et al. (2019). Altered resting-state cerebellar-cerebral functional connectivity in obsessive-compulsive disorder. Psychological Medicine, 49(7), 1156–1165. https://doi.org/10.1017/S0033291718001915
Ye, Q., Zhang, Z., Sun, W., Fan, Q., & Li, Y. (2021). Disrupted functional connectivity of precuneus subregions in obsessive-compulsive disorder. NeuroImage: Clinical, 31, 102720. https://doi.org/10.1016/j.nicl.2021.102720.
Yoshimura, M., et al. (2019). Hyperactivation of the frontal control network revealed by symptom provocation in obsessive-compulsive disorder using EEG microstate and sLORETA analyses. Neuropsychobiology, 77(4), 176–185. https://doi.org/10.1159/000491719
Zhu, X., et al. (2012). Evidence of a dissociation pattern in resting-state default mode network connectivity in first-episode, treatment-naive major depression patients. Biological Psychiatry, 71(7), 611–617. https://doi.org/10.1016/j.biopsych.2011.10.035
Acknowledgements
This work is partially supported by the "Department of excellence 2018-2022" initiative of the Italian Ministry of University and Research (MIUR) awarded to the Department of Neuroscience, University of Padova. SF’s PhD fellowship is supported by the Cassa di Risparmio di Padova e Rovigo (CARIPARO) Foundation. AV is partially supported by a grant from the Italian Ministry of Health (project code: GR-2018-12367927—FINAGE).
Funding
Open access funding provided by Università degli Studi di Padova within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Informed consent
Informed consent not applicable to this article as no data were directly collected during the current study.
Conflicts of interest
The authors report no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fornaro, S., Vallesi, A. Functional connectivity abnormalities of brain networks in obsessive–compulsive disorder: a systematic review. Curr Psychol 43, 900–930 (2024). https://doi.org/10.1007/s12144-023-04312-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12144-023-04312-x