Abstract
Objective
To describe the clinical and laboratory profile, management, intensive care needs, and outcome of children with toxic shock syndrome (TSS) admitted to the pediatric intensive care unit (PICU) of a tertiary care center in North India.
Methods
This retrospective study was conducted in the PICU of a tertiary care hospital in North India over a period of 10 y (January 2011–December 2020) including children < 12 y with TSS (n = 63).
Results
The median (interquartile range, IQR) age was 5 (2–9) y, 58.7% were boys, and Pediatric Risk of Mortality III (PRISM-III) score was 15 (12–17). The primary focus of infection was identified in 60.3% children, 44.5% had skin and soft tissue infections, and 17.5% (n = 11) had growth of Staphylococcus aureus. Common manifestations were shock (100%), rash (95.2%), thrombocytopenia (79.4%), transaminitis (66.7%), coagulopathy (58.7%), and acute kidney injury (AKI) (52.4%); and involvement of gastrointestinal (61.9%), mucus membrane (55.5%), respiratory (47.6%), musculoskeletal (41.3%), and central nervous system (CNS) (31.7%). The treatment included fluid resuscitation (100%), vasoactive drugs (92.1%), clindamycin (96.8%), intravenous immunoglobulin (IVIG) (92.1%), blood products (74.6%), mechanical ventilation (58.7%), and renal replacement therapy (31.7%). The mortality was 27% (n = 17). The duration of PICU and hopsital stay was 5 (4–10) and 7 (4–11) d, respectively. Higher proportion of nonsurvivors had CNS involvement, transaminitis, thrombocytopenia, coagulopathy, and AKI; required mechanical ventilation and blood products; and had higher vasoactive–inotropic score.
Conclusion
TSS is not uncommon in children in Indian setup. The management includes early recognition, intensive care, antibiotics, source control, and adjunctive therapy (IVIG and clindamycin). Multiorgan dysfunction and need for organ supportive therapies predicted mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Toxic shock syndrome (TSS) is an uncommon superantigen-mediated disease caused by toxin-producing strains of Staphylococcus aureus (TSS toxin 1, TSST-1) or Streptococcus pyogenes (pyrogenic exotoxin A, B, or both) [1, 2]. The pathophysiology of TSS is linked to superantigen exotoxins, which, in contrast to conventional antigens, are not processed by antigen-presenting cells before being presented to T cells. They directly stimulate T cells by cross-linking major histocompatibility complex class II molecules. This results in massive T-cell activation, uncontrolled immune stimulation and release of proinflammatory mediators (cytokine storm). The effect of this cascade is responsible for manifestations of TSS like fever, erythematous rash, gastrointestinal (GI) symptoms, capillary leak, hypotension, and multiorgan dysfunction syndrome (MODS) [2]. Many streptococci and staphylococci have the genes for toxin production, but they are expressed only under certain conditions. Transformation of infections into TSS can occur when toxins are produced in the absence of protective antibodies in the host. The protective antibody titers increase with age, and for this reason, children are more susceptible to TSS [3]. The course is fulminant and despite treatment, the mortality rate remains high, 4%–56% in streptococcal TSS and 0–22% in staphylococcal TSS [3,4,5]. However, the outcome of TSS is more favorable in children than in adults [6].
The diagnosis of TSS is based on standardized case definitions [7,8,9]. Some manifestations may be transient (i.e., hypotension), lacking (i.e., cutaneous rash), or have delayed occurrence (i.e., desquamation). Therefore, the diagnosis is often difficult during the early stages, and it may be difficult at times to distinguish TSS from septic shock, Kawasaki disease with shock, and drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome [10]. Also, there is an overlap between TSS and other tropical infections like scrub typhus, dengue, malaria, leptospirosis, and enteric fever, as the common presentations include febrile illness, shock, and multisystemic involvement [11]. Moreover, during the current coronavirus disease 2019 (COVID-19) pandemic, multisystemic inflammatory syndrome in children (MIS-C) is a close differential of TSS which warrants specific treatment as per the disease phenotype [12,13,14]. It is important to differentiate TSS from the above conditions, as the specific treatments differ. Prompt recognition of TSS is important as early administration of antibiotics, management of shock, targeted/adjunctive therapy [clindamycin and intravenous immunoglobulin (IVIG)], and supportive care in pediatric intensive care unit (PICU) are of paramount importance to decrease the mortality [3, 5, 15, 16]. The pediatricians and pediatric intensivists should be aware about the diagnosis of TSS for early recognition, timely treatment, and better outcome.
Majority of the data on TSS in children is available from the developed countries [3, 5, 16,17,18]. The data regarding incidence, management, and outcome of TSS in children from India are limited to case reports [19,20,21]. There is no information on differences in TSS in developed versus resource-limited countries like India. Also, there is not much explanation on why the TSS is uncommon in India where the staphylococcal infections are common [22]. Therefore, this study was planned with the objective to describe the clinical laboratory profile, management, intensive care needs, and outcome of children with TSS admitted to PICU of a tertiary care center in North India.
Material and Methods
This retrospective study was conducted in a level III PICU of a tertiary care referral hospital in North India over a period of 10 y (January 2011–December 2020) involving children ≤ 12 y with the diagnosis of TSS. Approval was obtained from the Institute Ethics Committee and the Departmental Review Board.
Diagnostic criteria for staphylococcal TSS included 3 major criteria (all required) including fever (temperature > 38.8 °C), hypotension, and rash (erythroderma with convalescent desquamation); ≥ 3 minor criteria including mucus membrane inflammation (oropharyngeal, conjunctival, vaginal hyperemia, strawberry tongue), GI symptoms (vomiting, diarrhea), liver abnormalities (bilirubin or transaminases levels > twice the upper limit of normal), renal abnormalities (blood urea nitrogen or creatinine > twice the upper limit of normal, or > 5 white blood cells per high power field), muscle abnormalities (myalgia, or creatinine phosphokinase > twice the upper limit of normal), CNS abnormalities (alteration in sensorium without focal neurological deficits), and thrombocytopenia (≤ 100,000/cumm); and exclusion of other explanation, and negative blood cultures (except occasionally for Staphylococcus aureus). Clinical criteria for streptococcal TSS included hypotension plus ≥ 2 of the features including renal impairment, coagulopathy, hepatic involvement, acute respiratory distress syndrome, generalized erythematous macular rash, and soft tissue necrosis. The definitive case included clinical criteria plus group A streptococcus from a normally sterile site and probable case included clinical criteria plus group A streptococcus from a nonsterile site [7,8,9].
Data with respect to demographic details, symptoms, prereferral admission and treatment, physiological status at admission, primary site of infection, and Pediatric Risk of Mortality III (PRISM-III) score were retrieved from the admission files and PICU electronic database manager and entered on a prestructured proforma. Organ system involvement including shock, mucocutaneous, GI, respiratory, and central nervous system (CNS) involvement, transaminitis, thrombocytopenia, coagulopathy, and acute kidney injury (AKI) were recorded. Laboratory investigations including complete blood count, renal and liver functions tests, C-reactive protein (CRP), and culture results were noted. Treatment details including fluid boluses, vasoactive drugs including vasoactive–inotropic score (VIS), intravenous antibiotics, respiratory support, blood components, and renal replacement therapy (RRT) were recorded. Adjunctive therapies used to target the toxin (IVIG and clindamycin) were noted. Final outcome (survival or death), and length of PICU and hospital stay were also recorded.
Data entry and statistical analysis were performed using Microsoft Excel 2013 (Microsoft, Redmond, WA) and SPSS software version 21 (IBM Corp. 2012. IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp). The categorical variables were expressed as numbers and percentages, and continuous variables as median (interquartile range, IQR). Comparison between survivors and nonsurvivors was done by Chi-Square or Fisher exact tests for categorical variables and Mann–Whitney U test for continuous variables. All tests were two-tailed and a p value < 0.05 was considered statistically significant.
Results
A total of 63 children with median (IQR) age of 5 (2–9) y, fulfilling the criteria for staphylococcal TSS, were admitted during the study period. None of the cases had confirmed or probable streptococcal TSS. Thirty-seven (58.7%) were boys. The most common clinical symptoms were fever (100%), rash (95.2%), diarrhea (49.2%), rapid breathing (47.6%), vomiting (42.9%), altered sensorium (23.8%), and cough (15.9%). The duration of symptoms before hospitalization was 4 (2–7) d (Table 1).
Majority (93.7%) of children were admitted in prereferral hospitals where they received intravenous antibiotics (85.7%), intravenous fluids (84.1%), oxygen support (50.3%), fluid boluses (15.9%), and vasoactive medications (11.1%) (Table 1).
The physiological status at admission to the authors’ hospital was hypotensive shock in 41.3% children; compensated shock, respiratory distress, and systemic dysfunction in 14.3% each; respiratory failure in 12.7%; and cardiopulmonary failure in 3.2% children. The median PRISM-III score was 15 (12–17). A primary focus of infection was identified in 60.3% children, the commonest being skin and soft tissue (44.5%), lower respiratory tract (14.3%), and burns (1.6%) (Table 1).
During the course of illness in the hospital, the organ systems involved included hypotensive shock (100%), diffuse macular erythroderma and/or generalized erythematous macular rash (95.2%), thrombocytopenia (79.4%), transaminitis (66.7%), GI involvement (61.9%) in the form of diarrhea and/or vomiting, coagulopathy (58.7%), mucus membrane involvement (55.5%) in the form of oropharyngeal erythema and/or conjunctival congestion, AKI (52.4%), respiratory system (47.6%), musculoskeletal (41.3%), and CNS involvement (31.7%) (altered sensorium in 16; and seizures and altered sensorium in 4 children) (Table 2). Baseline laboratory investigations are shown in Table 3. There were 12 positive cultures for Staphylococcus aureus (6 blood cultures and 6 pus cultures) in 11 (17.5%) children, which included 5 methicillin-sensitive Staphylococcus aureus (MSSA) and 7 methicillin-resistant Staphylococcus aureus (MRSA) (Table 3). One child had MRSA growth from both blood and pus.
Treatment details are provided in Table 4. All children received antibiotics including ceftriaxone (96.8%), cloxacillin (98.4%), clindamycin (96.8%), and vancomycin (50.8%). All cases had shock during the course of illness, which was managed with fluid boluses (100%) and vasoactive drugs (92.1%). The median VIS was 35 (20–80). Most cases (92.1%) received IVIG. Organ support therapies included mechanical ventilation (58.7%) for a duration of 5 (2–8) d, blood component therapy (74.6%), and RRT (31.7%). Seventeen children (27%) died. The length of PICU and hospital stay in survivors was 5 (4–10) and 7 (4–11) d, respectively (Table 4).
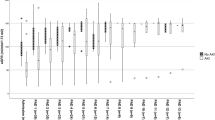
The nonsurvivors had higher proportion of CNS involvement (p = 0.005), transaminitis (p = 0.03), thrombocytopenia (p = 0.013), coagulopathy (p = 0.024), AKI (p = 0.004), and higher need for organ support therapies like mechanical ventilation (p = 0.001) and blood components, (p = 0.03), and had higher VIS (p = 0.01) (Table 5).
Discussion
This is the first report on the profile of children with TSS from India with respect to treatment, intensive care needs, and short-term outcome. Although standardized case definitions for TSS exist [7,8,9], the diagnosis is often difficult, especially during the early stages or in the absence of hypotensive shock. Careful observation in suspected cases is desired to pick up the additional features and development of hypotension during the course of illness.
The common differentials for TSS include septic shock, Kawasaki disease with shock, and DRESS syndrome [10]; tropical infections (scrub typhus, dengue, malaria, leptospirosis, and enteric fever) [11]; and post COVID-19 MIS-C [12,13,14]. It is important for pediatricians and pediatric intensivists to maintain a high index of suspicion and recognize the constellation of evolving signs and symptoms and laboratory markers in children with skin and soft tissue infections who present with shock, especially in tropical region like India. Timely resuscitation (fluids and vasoactive drugs), appropriate antibiotics, targeted/adjunctive therapy (IVIG and clindamycin), timely source control, and supportive care in PICU are important to prevent morbidity and mortality [3, 5, 15, 16].
Since the authors’ is a tertiary care referral center, the children reported in the index study most likely represent the severe end of the disease spectrum as all cases were admitted to PICU, all had shock, 92.1% required vasoactive drugs, and 59% required invasive mechanical ventilation. The median age was 5 (2-9) y, which was comparable to the previously reported data [3, 5, 16]. Although TSS is caused by both staphylococcus and streptococcus, the TSS reported by the authors is mainly staphylococcal; majority of children had underlying skin and soft tissue infection (44.5%) and all positive isolates were staphylococci (19%). The predominance of staphylococcal skin and soft tissue infection in a tropical country like India [22] is the main reason for more staphylococcal rather than streptococcal TSS. The common manifestations included fever, rash, shock, thrombocytopenia, coagulopathy, transaminitis, AKI; and musculoskeletal, GI, respiratory, and CNS involvement similar to what has been reported in other studies [3, 5, 16].
The treatment of TSS includes early recognition, resuscitation, targeted antibiotics, wound hygiene, appropriate drainage and debridement of necrotic tissue to remove foci of bacterial toxin production, adjunctive treatment (clindamycin and IVIG), and supportive care in PICU [15, 23, 24]. Some antibiotics (clindamycin, rifampicin, or linezolid) possess antitoxin effects by reducing exotoxin synthesis which may result in reduction in inflammation and cytokine storm [15]. IVIG neutralize the superantigens [25, 26] and has been shown to reduce mortality in TSS, especially in streptococcal TSS in adults [27, 28]. Although definitive evidence for beneficial effects of either IVIG or clindamycin in children with TSS is lacking, they are relatively safe treatments and suggested as adjunctive treatment in children with TSS [5, 15, 24]. Underusage of agents with antitoxin activity (IVIG and clindamycin) in TSS has been suggested to contribute to higher mortality [2, 3, 5, 29].
Most children in the index study required significant multisystem supportive therapies in PICU. The mortality was 27%, which was in the range of reported mortality in other studies [3, 30]. Higher proportion of nonsurvivors had CNS involvement, transaminitis, thrombocytopenia, coagulopathy, AKI, and requirement of invasive mechanical ventilation and blood products, and had higher VIS as compared to survivors. Strom et al. [18] also demonstrated that higher age, respiratory failure, liver disease/failure, chickenpox, and coagulopathy were predictors of mortality in children with TSS.
Most of the studies on TSS in children are mainly from the developed countries [3, 5, 16,17,18] and literature on this subject is limited from India [19,20,21]. Adalat et al. [3] reported 49 children with TSS from pediatric and burns units in the United Kingdom and Ireland (November 2008 and December 2009), and noted that 59.2% (n = 29) had streptococcal TSS and 20.8% (n = 20) had staphylococcal TSS. Skin and soft tissue (30.6%, n = 15) and burns (8.2%, n = 4) were the most common foci of infection. The site of infection was not recognized in 30.6% (n = 15). Children with streptococcal TSS were younger than those with staphylococcal TSS (3.8 vs. 9.5 y; p < 0.003). Majority (78%) needed PICU admission where they received invasive mechanical ventilation (69%), inotropic support (67%), and hemofiltration (12%). The adjuvant therapies with antitoxin effects were underutilized (clindamycin in 67%, IVIG in 20%, and fresh frozen plasma in 40% children). The mortality rate was 16.3% (n = 8) and all were in streptococcal TSS group (28% of streptococcal cases) and none of them received IVIG. There was no mortality in staphylococcal TSS group. Chen et al. [5], in a retrospective study, reported 62 children over a period of 11 y (2003–2014) from Victoria, Australia. Among them, 69.4% (n = 43) had staphylococcal and 30.6% (n = 19) had streptococcal TSS. S. aureus was isolated from 62.8% (27/43) staphylococcal TSS and S. pyogenes was isolated from all 19 streptococcal TSS cases. Admission to the PICU was required in 74% (n = 46) children. Management included inotropic support (71%, n = 44), IVIG (48.4%, n = 30), clindamycin (90.3%, n = 56), clindamycin and IVIG (45.2%, n = 28), fresh frozen plasma (24%, n = 15), and extracorporeal membrane oxygenation (ECMO) (11.3%, n = 7). There was no mortality. Children with streptococcal TSS were younger; higher proportion had coagulopathy and left ventricular dysfunction; was more likely to receive mechanical ventilation, ECMO, hemofiltration, and surgical procedure; and had more residual morbidity at discharge as compared with staphylococcal TSS.
The authors’ observations were similar, barring the fact that their cohort comprised mainly staphylococcal TSS, all were admitted to PICU, and majority received clindamycin and IVIG along with other supportive therapy. S. aureus was isolated in only 17.4% children. This was in line with the pathophysiology of staphylococcal TSS, where the toxin production occurs at distant sites, often in the absence of bacteremia or positive culture from a sterile site [5]. Other studies reported that S. aureus was isolated in 10%–63% of children with staphylococcal TSS [3, 5].
The strengths of the present study are that this is the first study on TSS in children from India with large sample size; the standard diagnostic criteria for TSS and organ system involvement were followed. This report gives a comprehensive picture of the organ systems affected. The retrospective study design and being a single-center study are its major limitations. The present data is skewed towards more severe TSS as the authors’ center is a tertiary care referral hospital. The long-term outcome has not been reported.
Conclusion
Early recognition of TSS by identifying constellation of signs and symptoms is important. Management includes early referral, intensive care, targeted antibiotics, and adjunctive therapies (IVIG and clindamycin). Despite aggressive treatment, mortality can be high. Multiorgan dysfunction and need for organ supportive therapies predicted mortality.
References
Noorbakhsh S, Rabiei AA, Rahbarimanesh AA, Haghighi M, Ashouri S. Searching the staphylococcal toxic shock syndrome toxin -1 in septic children with negative cultures: a comparative study in Tehran. Iran Infect Disord Drug Targets. 2021;21:187–92.
Javouhey E, Bolze PA, Jamen C, et al. Similarities and differences between staphylococcal and streptococcal toxic shock syndromes in children: results from a 30-case cohort. Front Pediatr. 2018;6:360.
Adalat S, Dawson T, Hackett SJ, Clark JE. In association with the British Paediatric Surveillance U. Toxic shock syndrome surveillance in UK children. Arch Dis Child. 2014;99:1078–82.
Descloux E, Perpoint T, Ferry T, et al. One in five mortality in non-menstrual toxic shock syndrome versus no mortality in menstrual cases in a balanced French series of 55 cases. Eur J Clin Microbiol Infect Dis. 2008;27:37–43.
Chen KY, Cheung M, Burgner DP, Curtis N. Toxic shock syndrome in Australian children. Arch Dis Child. 2016;101:736–40.
Chuang YY, Huang YC, Lin TY. Toxic shock syndrome in children: epidemiology, pathogenesis, and management. Paediatr Drugs. 2005;7:11–25.
Case definitions for infectious conditions under public health surveillance. Centers for disease control and prevention. MMWR Recomm Rep. 1997;46:1–55.
Hajjeh RA, Reingold A, Weil A, Shutt K, Schuchat A, Perkins BA. Toxic shock syndrome in the United States: surveillance update, 1979 1996. Emerg Infect Dis. 1999;5:807–10.
Defining the group A streptococcal toxic shock syndrome. Rationale and consensus definition. The Working Group on Severe Streptococcal Infections. JAMA. 1993;269:390–1.
Lin YJ, Cheng MC, Lo MH, Chien SJ. Early differentiation of kawasaki disease shock syndrome and toxic shock syndrome in a pediatric intensive care unit. Pediatr Infect Dis J. 2015;34:1163–7.
Nallasamy K, Gupta S, Bansal A, et al. Clinical profile and predictors of intensive care unit admission in pediatric scrub typhus: a retrospective observational study from North India. Indian J Crit Care Med. 2020;24:445–50.
Takia L, Angurana SK, Nallasamy K, Bansal A, Muralidharan J. Updated management protocol for multisystem inflammatory syndrome in children (MIS-C). J Trop Pediatr. 2021;67:fmab071.
Henderson LA, Canna SW, Friedman KG, et al. American college of rheumatology clinical guidance for multisystem inflammatory syndrome in children associated with sars-cov-2 and hyperinflammation in pediatric COVID-19: Version 2. Arthritis Rheumatol. 2021;73:e13-29.
Godfred-Cato S, Abrams JY, Balachandran N, et al. Distinguishing multisystem inflammatory syndrome in children from covid-19, kawasaki disease and toxic shock syndrome. Pediatr Infect Dis J. 2022;41:315–23.
Wilkins AL, Steer AC, Smeesters PR, Curtis N. Toxic shock syndrome - the seven Rs of management and treatment. J Infect. 2017;74(Suppl 1):S147–52.
Cook A, Janse S, Watson JR, Erdem G. Manifestations of toxic shock syndrome in children, Columbus, Ohio, USA, 2010–20171. Emerg Infect Dis. 2020;26:1077–83.
Gaensbauer JT, Birkholz M, Smit MA, Garcia R, Todd JK. Epidemiology and clinical relevance of toxic shock syndrome in US children. Pediatr Infect Dis J. 2018;37:1223–6.
Strom MA, Hsu DY, Silverberg JI. Prevalence, comorbidities and mortality of toxic shock syndrome in children and adults in the USA. Microbiol Immunol. 2017;61:463–73.
Roy P, Sahni AK, Kumar A. A fatal case of staphylococcal toxic shock syndrome. Med J Armed Forces India. 2015;71(Suppl 1):S107–10.
Nandwani S, Pande A, Saluja M. A case of Staphylococcus toxic shock syndrome presenting with multiple pneumatocoeles in the chest. Indian J Chest Dis Allied Sci. 2013;55:45–7.
Zaki SA, Shanbag P, Chavan V, Shenoy P. Staphylococcal toxic shock syndrome presenting as acute respiratory distress and cor pulmonale. Ann Trop Paediatr. 2010;30:77–81.
Baranwal AK, Singhi SC, Jayashree M. A 5-year PICU experience of disseminated staphylococcal disease, part 1: clinical and microbial profile. J Trop Pediatr. 2007;53:245–51.
Lappin E, Ferguson AJ. Gram-positive toxic shock syndromes. Lancet Infect Dis. 2009;9:281–90.
Gottlieb M, Long B, Koyfman A. The evaluation and management of toxic shock syndrome in the emergency department: a review of the literature. J Emerg Med. 2018;54:807–14.
Sriskandan S, Ferguson M, Elliot V, Faulkner L, Cohen J. Human intravenous immunoglobulin for experimental streptococcal toxic shock: bacterial clearance and modulation of inflammation. J Antimicrob Chemother. 2006;58:117–24.
Kaul R, McGeer A, Norrby-Teglund A, et al. Intravenous immunoglobulin therapy for streptococcal toxic shock syndrome--a comparative observational study. The Canadian Streptococcal Study Group. Clin Infect Dis. 1999;28:800–7.
Amreen S, Brar SK, Perveen S, Chaudhry MR, AlBabtain S, Khan S. Clinical efficacy of intravenous immunoglobulins in management of toxic shock syndrome: an updated literature review. Cureus. 2021;13:e12836.
Parks T, Wilson C, Curtis N, Norrby-Teglund A, Sriskandan S. Polyspecific intravenous immunoglobulin in clindamycin-treated patients with streptococcal toxic shock syndrome: a systematic review and meta-analysis. Clin Infect Dis. 2018;67:1434–6.
Curtis N. Toxic shock syndrome: under-recognised and under-treated? Arch Dis Child. 2014;99:1062–4.
Shah SS, Hall M, Srivastava R, Subramony A, Levin JE. Intravenous immunoglobulin in children with streptococcal toxic shock syndrome. Clin Infect Dis. 2009;49:1369–76.
Funding
None.
Author information
Authors and Affiliations
Contributions
SKA: Conceptualization of the study, literature review, data analysis, and manuscript preparation; PA: Data collection and analysis; SKC: Data collection; KN: Data analysis and literature review; AB: Supervision of the study and literature review; MJ: Conceptualization and supervision of the study and final review of the manuscript. All authors approved the final manuscript. MJ will act as the guarantor for this paper.
Corresponding author
Ethics declarations
Ethical Approval
Institute Ethics Committee (IEC), PGIMER, Chandigarh; No. INT/IEC/2021/SPL1978, dated 11/6/2021.
Conflict of Interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Suresh Kumar Angurana and Puspraj Awasthi are joint first authors.
Rights and permissions
About this article
Cite this article
Angurana, S.K., Awasthi, P., K.C., S. et al. Clinical Profile, Intensive Care Needs, and Short-Term Outcome of Toxic Shock Syndrome Among Children: A 10-Year Single-Centre Experience from North India. Indian J Pediatr 90, 334–340 (2023). https://doi.org/10.1007/s12098-022-04271-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-022-04271-4