Abstract
In this paper, we review the current state of breakthrough cancer pain (BTcP) management. BTcP is a heterogeneous condition and a global problem for cancer patients. It is often managed suboptimally, which results in a negative outcome for patients, healthcare providers, and healthcare systems. Several barriers to the appropriate management of BTcP have been identified. These include, among others, an incomplete definition of BTcP, poor training of healthcare providers and patients alike, a lack of a multidisciplinary approach and the absence of specific protocols and tools. We provide some actions to help physicians and patients improve their approach to BTcP, including specific training, the design of easy-to-use tools for BTcP identification and assessment (such as checklists and pocket-sized cards), individualized treatment, and the use of multidisciplinary teams.

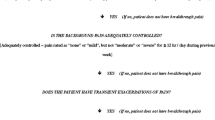
adapted from Davies et al. [29]

Similar content being viewed by others
References
Edwards BK, Brown ML, Wingo PA, Howe HL, Ward E, Ries LAG, et al. Annual report to the nation on the status of cancer, 1975–2002, featuring population-based trends in cancer treatment. J Natl Cancer Inst. 2005;97(19):1407–27.
Margarit C, Juliá J, López R, Anton A, Escobar Y, Casas A, et al. Breakthrough cancer pain-still a challenge. J Pain Res. 2012;5:559–66.
González-Escalada JR, Camba A, Casas A, Gascón P, Herruzo I, Núñez-Olarte JM, et al. Código de buena práctica para el control del dolor oncológico. Revista de la Sociedad Española del Dolor. 2011;18(2):98–117.
Maxwell K. The challenges of cancer pain assessment and management. Ulster Med J. 2012;81(2):100–1.
Mercadante S. The patient with difficult cancer pain. Cancers (Basel). 2019;11(4):565.
Fallon M, Giusti R, Aielli F, Hoskin P, Rolke R, Sharma M, et al. Management of cancer pain in adult patients: ESMO Clinical Practice Guidelines. Ann Oncol. 2018;29(Supplement_4):iv166–iv191.
Mercadante S. Treating breakthrough pain in oncology. Expert Rev Anticancer Ther. 2018;18(5):445–9.
Vellucci R, Mediati RD, Gasperoni S, Mammucari M, Marinangeli F, Romualdi P. Assessment and treatment of breakthrough cancer pain: from theory to clinical practice. J Pain Res. 2017;10:2147–55.
Mercadante S. Breakthrough pain in cancer patients: prevalence, mechanisms and treatment options. Curr Opin Anaesthesiol. 2015;28(5):559–64.
Sabato AF. Idiopathic breakthrough pain: a new hypothesis. Clin Drug Investig. 2010;30(Suppl 2):27–9.
Fortner BV, Demarco G, Irving G, Ashley J, Keppler G, Chavez J, et al. Description and predictors of direct and indirect costs of pain reported by cancer patients. J Pain Symptom Manage. 2003;25(1):9–18.
Petzke F, Radbruch L, Zech D, Loick G, Grond S. Temporal presentation of chronic cancer pain: transitory pains on admission to a multidisciplinary pain clinic. J Pain Symptom Manage. 1999;17(6):391–401.
Portenoy RK, Payne D, Jacobsen P. Breakthrough pain: characteristics and impact in patients with cancer pain. Pain. 1999;81(1–2):129–34.
Swanwick M, Haworth M, Lennard RF. The prevalence of episodic pain in cancer: a survey of hospice patients on admission. Palliat Med. 2001;15(1):9–18.
Deandrea S, Corli O, Consonni D, Villani W, Greco MT, Apolone G. Prevalence of breakthrough cancer pain: a systematic review and a pooled analysis of published literature. J Pain Symptom Manage. 2014;47(1):57–76.
Working Group Nientemale DEI, Vellucci R, Fanelli G, Pannuti R, Peruselli C, Adamo S, et al. What to do, and What not to do, When diagnosing and dreating breakthrough cancer pain (BTcP): expert opinion. Drugs. 2016;76(3):315–30.
Yang P, Cheville AL, Wampfler JA, Garces YI, Jatoi A, Clark MM, et al. Quality of life and symptom burden among long-term lung cancer survivors. J Thorac Oncol. 2012;7(1):64–70.
American Pain Foundation n. Breakthrough cancer pain: mending the break in the continuum of care. J Pain Palliat Care Pharmacother. 2011;25(3):252–64.
Davies A, Buchanan A, Zeppetella G, Porta-Sales J, Likar R, Weismayr W, et al. Breakthrough cancer pain: an observational study of 1000 European oncology patients. J Pain Symptom Manage. 2013;46(5):619–28.
Mantyh PW. Cancer pain and its impact on diagnosis, survival and quality of life. Nat Rev Neurosci. 2006;7(10):797–809.
Perez-Hernandez C, Jimenez-Lopez AJ, Sanz-Yague A, Mar-Medina J, Larranaga I, Soler-Lopez B. Observational study evaluating the economic impact of breakthrough pain in cancer patients in clinical practice in Spain: the IMDI study. Pain Ther. 2018;7(2):227–40.
Ruggeri M, Turriziani A, Oradei M. Cost-effectiveness analysis of transnasal fentanyl citrate for the treatment of breakthrough cancer pain. Expert Rev Pharmacoecon Outcomes Res. 2014;14(3):459–64.
Fortner BV, Okon TA, Portenoy RK. A survey of pain-related hospitalizations, emergency department visits, and physician office visits reported by cancer patients with and without history of breakthrough pain. J Pain. 2002;3(1):38–44.
Fortner BV, Okon TA, Ashley J, Kepler G, Chavez J, Tauer K, et al. The zero acceptance of pain (ZAP) quality improvement project: evaluation of pain severity, pain interference, global quality of life, and pain-related costs. J Pain Symptom Manage. 2003;25(4):334–43.
Mularski RA, White-Chu F, Overbay D, Miller L, Asch SM, Ganzini L. Measuring pain as the 5th vital sign does not improve quality of pain management. J Gen Intern Med. 2006;21(6):607–12.
Camps Herrero C, Reina Zoilo JJ, Monge Martín D, Caballero Martínez F, Guillem Porta V, Aranda Aguilar E, et al. Active study: undetected prevalence and clinical inertia in the treatment of breakthrough cancer pain (BTcP). Clin Transl Oncol. 2019;21(3):380–90.
Escobar Álvarez Y, Biete i Solà A, Camba Rodríguez M, Gálvez Mateos R, Mañas Rueda A, Rodríguez Sánchez CA, et al. Diagnóstico y tratamiento del dolor irruptivo oncológico: recomendaciones de consenso. Revista de la Sociedad Española del Dolor. 2013;20(2):61–8.
García-Mata J, Álamo C, de Castro J, Contreras J, Gálvez R, Jara C, et al. A survey of perceptions, attitudes, knowledge and practices of medical oncologists about cancer pain management in Spain. Clin Transl Oncol. 2018;20(8):1061–71.
Association for Palliative Medicine of Great B 2009 The management of cancer-related breakthrough pain: recommendations of a task group of the Science Committee of the Association for Palliative Medicine of Great Britain and Ireland Eur J Pain. 13 4 331 338
Mercadante S, Portenoy RK. Breakthrough cancer pain: twenty-five years of study. Pain. 2016;157(12):2657–63.
Løhre ET, Klepstad P, Bennett MI, Brunelli C, Caraceni A, Fainsinger RL, et al. From "breakthrough" to "episodic" cancer pain? A European association for palliative care research network expert delphi survey toward a common terminology and classification of transient cancer pain exacerbations. J Pain Symptom Manage. 2016;51(6):1013–9.
Jara C, Del Barco S, Gravalos C, Hoyos S, Hernandez B, Munoz M, et al. SEOM clinical guideline for treatment of cancer pain (2017). Clin Transl Oncol. 2018;20(1):97–107.
Kwon JH. Overcoming barriers in cancer pain management. J Clin Oncol. 2014;32(16):1727–33.
Breivik H, Cherny N, Collett B, de Conno F, Filbet M, Foubert AJ, et al. Cancer-related pain: a pan-European survey of prevalence, treatment, and patient attitudes. Ann Oncol. 2009;20(8):1420–33.
Carulla Torrent J, Jara Sánchez C, Sanz Ortiz J, Batista López N, Camps Herrero C, Cassinello Espinosa J, et al. Oncologists' perceptions of cancer pain management in Spain: the real and the ideal. Eur J Pain. 2007;11(3):352–9.
Kwon JH, Oh SY, Chisholm G, Lee J-A, Lee JJ, Park KW, et al. Predictors of high score patient-reported barriers to controlling cancer pain: a preliminary report. Support Care Cancer. 2013;21(4):1175–83.
Fallon M, Giusti R, Aielli F, Hoskin P, Rolke R, Sharma M, et al. Management of cancer pain in adult patients: ESMO Clinical Practice Guidelines†. Ann Oncol. 2018;29(Supplement_4):iv166–iv191.
Vellucci R. Breakthrough cancer pain. Eur J Oncol. 2015;20(suppl 1):11–2.
Boceta J, De la Torre A, Samper D, Farto M, Sánchez-de la Rosa R. Consensus and controversies in the definition, assessment, treatment and monitoring of BTcP: results of a Delphi study. Clin Transl Oncol. 2016;18(11):1088–97.
Webber K, Davies AN, Zeppetella G, Cowie MR. Development and validation of the breakthrough pain assessment tool (BAT) in cancer patients. J Pain Symptom Manage. 2014;48(4):619–31.
Webber K, Davies AN, Cowie MR. Accuracy of a diagnostic algorithm to diagnose breakthrough cancer pain as compared with clinical assessment. J Pain Symptom Manage. 2015;50(4):495–500.
Fallon M, Walker J, Colvin L, Rodriguez A, Murray G, Sharpe M, et al. Pain management in cancer center inpatients: a cluster randomized trial to evaluate a systematic integrated approach-the edinburgh pain assessment and management tool. J Clin Oncol. 2018;36(13):1284–90.
Jacobsen PB, Snyder CF. Improving pain assessment and management in routine oncology practice: the role of implementation research. J Clin Oncol. 2018;36(13):1272–4.
Porta-Sales J, Garzón Rodríguez C, Julià Torras J, Casals MM. Dolor irruptivo en cáncer. Med Clin (Barc). 2010;135(6):280–5.
Vissers DCJ, Lenre M, Tolley K, Jakobsson J, Sendersky V, Jansen JP. An economic evaluation of short-acting opioids for treatment of breakthrough pain in patients with cancer. Value Health. 2011;14(2):274–81.
Caraceni A, Davies A, Poulain P, Cortes-Funes H, Panchal SJ, Fanelli G. Guidelines for the management of breakthrough pain in patients with cancer. J Natl Compr Canc Netw. 2013;11(Suppl 1):S29–36.
Porta-Sales J, Pérez C, Escobar Y, Martínez V. Diagnosis and management of breakthrough cancer pain: Have all the questions been resolved? A Delphi-based consensus assessment (DOIRON). Clin Transl Oncol. 2016;18(9):945–54.
Álamo C, Zaragozá-Arnáez C, Noriega-Matanza C, M-Torres L. Fentanilo: una molécula y múltiples formulaciones galénicas de trascendencia clínica en el tratamiento del dolor irruptivo oncológico. Revista de la Sociedad Española del Dolor. 2017;24:188–200.
Rauck R, North J, Gever LN, Tagarro I, Finn AL. Fentanyl buccal soluble film (FBSF) for breakthrough pain in patients with cancer: a randomized, double-blind, placebo-controlled study. Ann Oncol. 2010;21(6):1308–14.
Buchanan A, Davies A, Geerling J. Breakthrough cancer pain: the role of the nurse. Int J Palliat Nurs. 2014;20(3):126–9.
Vallerand AH, Musto S, Polomano RC. Nursing's role in cancer pain management. Curr Pain Headache Rep. 2011;15(4):250–62.
Wengstrom Y, Geerling J, Rustoen T. European Oncology Nursing Society breakthrough cancer pain guidelines. Eur J Oncol Nurs. 2014;18(2):127–31.
Mercadante S, Adile C, Torta R, Varetto A, Fulfaro F, Giarratano A, et al. Meaningful cut-off pain intensity for breakthrough pain changes in advanced cancer patients. Curr Med Res Opin. 2013;29(1):93–7.
Mercadante S, Cuomo A. Breakthrough cancer pain: ten commandments. Value Health. 2016;19(5):531–6.
Olarte JMN. Breakthrough cancer pain and rational drug use. Support Care Cancer. 2017;25(Suppl 1):11–7.
López López R, Camps Herrero C, Khosravi-Shahi P, Guillem Porta V, Carrato Mena A, Garcia-Foncillas J, et al. Oncologist's knowledge and implementation of guidelines for breakthrough cancer pain in Spain: CONOCE study. Clin Transl Oncol. 2018;20(5):613–8.
O'Hagan P, Mercadante S. Breakthrough cancer pain: the importance of the right treatment at the right time. Eur J Pain. 2018;22(7):1362–74.
Caraceni A, Martini C, Zecca E, Portenoy RK, Ashby MA, Hawson G, et al. Breakthrough pain characteristics and syndromes in patients with cancer pain. An international survey. Palliat Med. 2004;18(3):177–83.
Zeppetella G, Davies AN. Opioids for the management of breakthrough pain in cancer patients. Cochrane Database Syst Rev. 2013; 21(10):CD004311. https://doi.org/10.1002/14651858.CD004311.pub3. Review. Update in: Cochrane Database Syst Rev. 2015;(8):CD004311.
Davies AN, Elsner F, Filbet MJ, Porta-Sales J, Ripamonti C, Santini D, et al. Breakthrough cancer pain (BTcP) management: a review of international and national guidelines. BMJ Support Palliat Care. 2018;8(3):241–9.
Camps C, Rubio ED, Lopez R, Carrato A, Gascon P, Margarita F, et al. The quality oncology practice initiative program: experience in Spain. J Clin Oncol. 2017;35(8_suppl):214.
Dubois MY, Follett KA. Pain medicine: The case for an independent medical specialty and training programs. Acad Med. 2014;89(6):863–8.
Sabia M, Weaver M, Gessman R, Kalariya J. Update on the importance of medical education in the changing field of pain medicine. J Anesthesia Patient Care. 2017;2:1–5.
Kuip EJ, Zandvliet ML, Koolen SL, Mathijssen RH, van der Rijt CC. A review of factors explaining variability in fentanyl pharmacokinetics; focus on implications for cancer patients. Br J Clin Pharmacol. 2017;83(2):294–313.
Daeninck P, Gagnon B, Gallagher R, Henderson JD, Shir Y, Zimmermann C, et al. Canadian recommendations for the management of breakthrough cancer pain. Curr Oncol. 2016;23(2):96–108.
Acknowledgments
We thank Pilar Lopez (LIDESEC) for their assistance in writing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors state that they have no conflicts of interest. Camps C. has received speaker honoraria from AstraZeneca, Roche, MSD, Pfizer, Bristol-Myers Squibb. He is an advisory board member at AstraZeneca, Boehringer Ingelheim, Bristol-Myers Squibb, MSD, Roche, Bayer and Angellini. He has received research funding from AstraZeneca and Bristol-Myers Squibb. Ilsa D. has received speaker honoraria from Amgen, AstraZeneca, BMS, Boehringer Ingelheim, Eli Lilly Oncology, F. Hoffmann-La Roche, MSD, Novartis, Pierre Fabre and Pfizer, and consultation honoraria from AbbVie, Amgen, AstraZeneca, BMS, Boehringer Ingelheim, Eli Lilly Oncology, F. Hoffmann-La Roche, Merck, MSD, Novartis, Pierre Fabre, Pfizer and Takeda. She has received research funding from AstraZeneca, BMS, F. Hoffmann-La Roche, MSD and Pierre Fabre. Additionally, she has a leadership role as an Executive Board Member of the Commission for the Approval of New Drugs. Regional Health Care Department, Spain.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Camps Herrero, C., Batista, N., Díaz Fernández, N. et al. Breakthrough cancer pain: review and calls to action to improve its management. Clin Transl Oncol 22, 1216–1226 (2020). https://doi.org/10.1007/s12094-019-02268-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-019-02268-8