Abstract
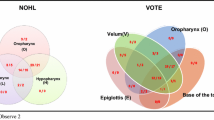
Purpose: To investigate associations between polysomnographic findings and the severity of upper airway obstructions during Muller’s Maneuver (MM) and Drug-Induced Sleep Endoscopy (DISE) in patients with obstructive sleep apnea syndrome (OSAS). Methods: This was a prospective cohort study. Adult patients newly diagnosed with OSAS in a tertiary sleep center were included consecutively and evaluated by polysomnography and MM. They then underwent DISE in an operating room. The associations between polysomnographic findings and the severity of upper airway obstructions during MM and DISE were assessed. Also, the degree and pattern of obstructions were compared using a modified VOTE questionnaire. Results: 145 patients (mean age 41.5 ± 10.1 years) were enrolled. There were no associations between Respiratory Disturbance Index (RDI), mean and lowest O2 saturation, and body mass index on the one hand, and obstruction degree in MM and DISE (p > 0.05). However, a significant positive correlation was observed between RDI and total VOTE scores in DISE and MM (r = 0.179, p = 0.031 and r = 0.221, p = 0.008 respectively). There were no differences between MM and DISE in diagnosing the degree of obstruction in the velum area (p = 0.687) and the epiglottis (p = 0.50). However, a significant difference was observed between the two techniques in the oropharynx lateral wall (p < 0.001) and tongue base (p = 0.017). Conclusion: Although there was no association between polysomnographic findings and the severity of obstruction in MM and DISE for the separate levels of the upper airway, obstruction severity may be assessed more accurately by total VOTE score, which is representative of RDI severity.
Similar content being viewed by others
Data Availability
Not applicable.
Code Availability
Not applicable.
References
Fusetti M, Fioretti AB, Valenti M, Masedu F, Lauriello M, Pagliarella M (2012) Cardiovascular and metabolic comorbidities in patients with obstructive sleep apnoea syndrome. Acta Otorhinolaryngol Ital 32(5):320–325
Young T, Evans L, Finn L, Palta M (1997) Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women. Sleep 20(9):705–706
Amali A, Motiee-Langroudi M, Saedi B, Rahavi-Ezabadi S, Karimian A, Amirzargar B (2017) A comparison of Uvulopalatopharyngoplasty and Modified Radiofrequency tissue ablation in mild to moderate obstructive sleep apnea: a Randomized Clinical Trial. J Clin Sleep Med 13(9):1089–1096. https://doi.org/10.5664/jcsm.6730
Sher AE, Schechtman KB, Piccirillo JF (1996) The efficacy of surgical modifications of the upper airway in adults with obstructive sleep apnea syndrome. Sleep 19(2):156–177
Faber CE, Grymer L (2003) Available techniques for objective assessment of upper airway narrowing in snoring and sleep apnea. Sleep Breath 7(2):77–86. https://doi.org/10.1007/s11325-003-0077-9
Belgu AU, Erdogan B, San T, Gurkan E (2015) The relationship between AHI, Epworth scores and sleep endoscopy in patients with OSAS. Eur Arch Otorhinolaryngol 272(1):241–245. https://doi.org/10.1007/s00405-014-3220-2
Schwartz RN, Payne RJ, Forest VI, Hier MP, Fanous A, Vallee-Gravel C (2015) The relationship between upper airway collapse and the severity of obstructive sleep apnea syndrome: a chart review. J Otolaryngol Head Neck Surg 44:32. https://doi.org/10.1186/s40463-015-0086-2
Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, Kapur VK, Marcus CL, Mehra R, Parthasarathy S, Quan SF, Redline S, Strohl KP, Davidson Ward SL, Tangredi MM, American Academy of Sleep (2012) Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med 8(5):597–619. https://doi.org/10.5664/jcsm.2172
Vroegop AV, Vanderveken OM, Wouters K, Hamans E, Dieltjens M, Michels NR, Hohenhorst W, Kezirian EJ, Kotecha BT, de Vries N, Braem MJ (2013) Observer variation in drug-induced sleep endoscopy: experienced versus nonexperienced ear, nose, and throat surgeons. Sleep 36(6) 947 – 53. https://doi.org/10.5665/sleep.2732. Van de
Petri N, Suadicani P, Wildschiodtz G, Bjorn-Jorgensen J (1994) Predictive value of Muller maneuver, cephalometry and clinical features for the outcome of uvulopalatopharyngoplasty. Evaluation of predictive factors using discriminant analysis in 30 sleep apnea patients. Acta Otolaryngol 114(5):565–571
Moon IJ, Han DH, Kim JW, Rhee CS, Sung MW, Park JW, Kim DS, Lee CH (2010) Sleep magnetic resonance imaging as a new diagnostic method in obstructive sleep apnea syndrome. Laryngoscope 120(12):2546–2554. https://doi.org/10.1002/lary.21112
Herzog M, Metz T, Schmidt A, Bremert T, Venohr B, Hosemann W, Kaftan H (2006) The prognostic value of simulated snoring in awake patients with suspected sleep-disordered breathing: introduction of a new technique of examination. Sleep 29(11):1456–1462. https://doi.org/10.1093/sleep/29.11.1456
Kum RO, Ozcan M, Yilmaz YF, Gungor V, Yurtsever N, Kum, Unal A (2014) The relation of the obstruction site on Muller’s Maneuver with BMI, Neck circumference and PSG Findings in OSAS. Indian J Otolaryngol Head Neck Surg 66(2):167–172. https://doi.org/10.1007/s12070-014-0699-1
Woodson BT, Naganuma H (1999) Comparison of methods of airway evaluation in obstructive sleep apnea syndrome. Otolaryngol Head Neck Surg 120(4):460–463
Friedman M, Tanyeri H, La Rosa M, Landsberg R, Vaidyanathan K, Pieri S, Caldarelli D (1999) Clinical predictors of obstructive sleep apnea. Laryngoscope 109(12):1901–1907. https://doi.org/10.1097/00005537-199912000-00002
Kheirandish-Gozal L, Gozal D (2008) The multiple challenges of obstructive sleep apnea in children: diagnosis. Curr Opin Pediatr 20(6):650–653. https://doi.org/10.1097/MOP.0b013e328316bdb2
Weitzman ED, Pollak C, Borowiecki B, Burack B, Shprintzen R, Rakoff S (1977) The Hypersomnia Sleep-Apnea Syndrome: site and mechanism of upper airway obstruction. Trans Am Neurol Assoc 102:150–153
Croft CB, Pringle M (1991) Sleep nasendoscopy: a technique of assessment in snoring and obstructive sleep apnoea. Clin Otolaryngol Allied Sci 16(5):504–509. https://doi.org/10.1111/j.1365-2273.1991.tb01050.x
Askar SM, Quriba AS, Hassan EM, Awad AM (2020) Positional Awake Endoscopy Versus DISE in Assessment of OSA: a comparative study. Laryngoscope 130(9):2269–2274. https://doi.org/10.1002/lary.28391
Ha JG, Lee Y, Nam JS, Park JJ, Yoon JH, Kim CH, Cho HJ (2020) Can drug-induced sleep endoscopy improve the success rates of tongue base surgery? J Otolaryngol Head Neck Surg 49(1):8. https://doi.org/10.1186/s40463-020-00405-w
Yegin Y, Celik M, Kaya KH, Koc AK, Kayhan FT (2017) Comparison of drug-induced sleep endoscopy and Muller’s maneuver in diagnosing obstructive sleep apnea using the VOTE classification system. Braz J Otorhinolaryngol 83(4):445–450. https://doi.org/10.1016/j.bjorl.2016.05.009
Soares D, Folbe AJ, Yoo G, Badr MS, Rowley JA, Lin HS (2013) Drug-induced sleep endoscopy vs awake Muller’s maneuver in the diagnosis of severe upper airway obstruction. Otolaryngol Head Neck Surg 148(1):151–156. https://doi.org/10.1177/0194599812460505
Hong SD, Dhong HJ, Kim HY, Sohn JH, Jung YG, Chung SK, Park JY, Kim JK (2013) Change of obstruction level during drug-induced sleep endoscopy according to sedation depth in obstructive sleep apnea. Laryngoscope 123(11):2896–2899. https://doi.org/10.1002/lary.24045
Yoon BW, Hong JM, Hong SL, Koo SK, Roh HJ, Cho KS (2016) A comparison of dexmedetomidine versus propofol during drug-induced sleep endoscopy in sleep apnea patients. Laryngoscope 126(3):763–767. https://doi.org/10.1002/lary.25801
Kim Y, Park H, Shin J, Choi JH, Park SW, Kang HY (2018) Effect of remifentanil during drug-induced sleep endoscopy in patients with obstructive sleep apnea. Sleep Breath 22(4):919–923. https://doi.org/10.1007/s11325-018-1738-z
Vroegop AV, Vanderveken OM, Verbraecken JA (2020) Drug-Induced Sleep Endoscopy: evaluation of a Selection Tool for Treatment Modalities for Obstructive Sleep Apnea. Respiration. 1–7. https://doi.org/10.1159/000505584
Viana A, Zhao C, Rosa T, Couto A, Neves DD, Araujo-Melo MH, Capasso R (2019) The Effect of Sedating Agents on Drug-Induced Sleep Endoscopy Findings. Laryngoscope 129(2):506–513. https://doi.org/10.1002/lary.27298
Aktas O, Erdur O, Cirik AA, Kayhan FT (2015) The role of drug-induced sleep endoscopy in surgical planning for obstructive sleep apnea syndrome. Eur Arch Otorhinolaryngol 272(8):2039–2043. https://doi.org/10.1007/s00405-014-3162-8
Safiruddin F, Koutsourelakis I, de Vries N (2015) Upper airway collapse during drug induced sleep endoscopy: head rotation in supine position compared with lateral head and trunk position. Eur Arch Otorhinolaryngol 272(2):485–488. https://doi.org/10.1007/s00405-014-3215-z
Lechner M, Wilkins D, Kotecha B (2018) A review on drug-induced sedation endoscopy - technique, grading systems and controversies. Sleep Med Rev 41:141–148. https://doi.org/10.1016/j.smrv.2018.02.001
Acknowledgements
The research was fully sponsored by Otorhinolaryngology Research Center of Tehran University of Medical Sciences.
Funding
This study received no funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing Interests
The authors declare no conflict of interest.
Financial Interests
None.
Non-financial Interests
None.
Ethical Approval
All procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964. Helsinki declaration. The study was approved by the institutional review board and Ethics Committee of Tehran University of Medical Sciences. (IR.TUMS.REC.1394.1697)
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Consent for Publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Amali, A., Erfanian, R., Amirzargar, B. et al. Polysomnographic Findings Versus Degree of Obstruction During Drug-Induced Sleep Endoscopy and Muller’s Maneuver. Indian J Otolaryngol Head Neck Surg 75, 2769–2776 (2023). https://doi.org/10.1007/s12070-023-03871-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-023-03871-6