Abstract
Evaluate the lingual manifestations of COVID-19, and provide a clinical guide in managing these symptoms. Electronic databases, such as PubMed/Medline, and Scopus were searched until November 1, 2020, and only randomized controlled trials, cross-sectional and cohort studies, as well as case reports and series, and review articles in English were considered. A total of 40 studies were included in this study. Lingual involvement has been extensively reported in patients with coronavirus disease 2019 (COVID-19). The most common features of lingual involvements were red or light red, yellow coating, and greasy coating tongue, though other complications, such as pale, purple, white coating, grayish-black coating, rough, tender, puffy, spotty, prickles, fissured, and tooth-marked tongue was also reported. Poor oral hygiene, opportunistic infections (OIs), medications, and hyper-inflammatory response to infection are the most common predisposing factors for the onset of oral lesions in patients with COVID-19. In conclusion, the current review described the lingual manifestations of COVID-19, and as oral complaints are relatively common in COVID-19 patients, an intraoral examination should be conducted in all suspected cases of SARS-CoV-2 infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
While respiratory and gastrointestinal complications were the main manifestations of coronavirus disease 2019 (COVID-19), many more manifestations became apparent as the pandemic progressed [1]. Lingual involvement has been extensively reported in COVID-19 patients. The most primary features are chemosensory disorders, such as smell and taste problems [2]. These complications frequently happen during many viral infections, such as influenza [3].
Tongue Features in COVID-19
Chemo-sensory disorders can be defined as diseases related to the sense of taste and smell. Taste disturbances can be categorized as quantitative and qualitative disorders. Hypogeusia, a diminished sense of taste, and ageusia, or the absence of taste, are examples of quantitative taste problems, while dysgeusia is a qualitative change in taste perception [4]. Temporary taste changes may be the sole manifestation of COVID-19 [5]. Dry mouth or xerostomia, which is reported in several patients due to hyposalivation or decreased saliva production [6], is associated with taste disturbances [7] and is manifested by an increased need for drinking fluids in patients with COVID-19 [8]. Some of these patients may even experience tongue burns or spicy, salty, sour, sweet taste, or even dysgeusia [9]. The tongue’s blisters, scattered reddish macules on the tongue [10], ulcers, and the tongue’s painful inflammation have also been reported [11].
Moreover, COVID-19 has been attributed to a Kawasaki-like disease with glossitis, also called red strawberry tongue [12]. Furthermore, the tongue can also be involved as a component of angioedema in the context of COVID-19 [13]. A new feature of COVID-19 has been reported in a patient presenting with Melkersson-Rosenthal syndrome (MRS), a triad of orofacial edema, facial paralysis, and fissured tongue [14].
Different medications used to treat COVID-19, such as remdesivir, favipiravir, ribavirin, and lopinavir/ritonavir, can also cause xerostomia and taste disorders [15, 16]. Also, chloroquine has been reported to be linked to transient oral pigmentations [17]. Moreover, azithromycin played a role in tongue discoloration and oral candidiasis [18]. Furthermore, intensive care unit (ICU) admitted patients who have been intubated routinely develop tongue coatings and candidiasis [19].
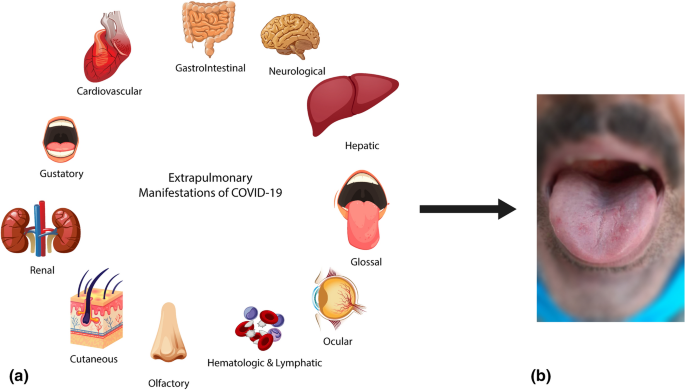
The tongue features of COVID-19 have been investigated in several studies, particularly in traditional Chinese medicine. Changes in tongue characteristics are correlated to the progression and severity of the disease [20]. The shape, color, and coating of the tongue, and color and thickness of the fur, are among the characteristics studied previously. The most common subjective characteristics of lingual involvement were red or light red tongue, yellow coating, and greasy coating. However, the pale tongue, purple tongue, white coating, grayish-black coating, rough tongue, tender tongue, puffy tongue, spots, prickles tongue, fissured tongue, and tooth-marked tongue were also reported [21]. Interestingly patients with milder COVID-19 had thinner tongues with lighter colors, while in patients with more severe disease, thicker coatings, more tender and purplish tongues were observed [22]. Figure 1 illustrates the extrapulmonary manifestations of COVID-19, and a patient with COVID-19 who manifested with erythematous tongue with deep grooves is presented.
Black hairy tongue (BHT) or lingua villosa nigra is quite commonly demonstrated in the COVID-19 setting. It is a painless and benign disorder due to the lack of desquamation and increased proliferation and hypertrophy of the tongue’s filiform papillae, leading to a black, sometimes brown, yellow, or green discoloration of the tongue, halitosis, and a metallic taste [23]. Several underlying conditions have been suggested to lead to this disorder, which include antibiotics, such as bismuth [24], amoxicillin [25], tetracycline [26], linezolid [27], and psychotropic agents, including olanzapine, phenothiazines, and tricyclic antidepressants [28]. Dehydration decreased saliva production, trigeminal neuralgia, poor oral hygiene, smoking, alcoholism, and infections were also observed to trigger this condition [29]. BHT may be asymptomatic or cause nausea, halitosis, or dysgeusia [30].
Pathophysiology of Tongue Involvement
In addition to the respiratory and gastrointestinal tract, the angiotensin-converting enzyme 2 (ACE2), which is a severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) receptor in the human body, is also expressed in the epithelium of the oral cavity, including the epithelial cells of the tongue [31]. ACE2 receptors are more densely located on the tongue’s dorsum, where the epithelium is significantly altered during COVID-19 and predisposes to overgrowth of anaerobic bacteria, leading to halitosis [32]. Any infectious or inflammatory conditions can lead to hyposalivation due to disturbed salivary secretion, and infection with SARS-CoV-2 can also initiate this process [33].
Dysgeusia and xerostomia may be due to nasal congestion and rhinorrhea caused by oral respiration in viral infections of the upper respiratory [34]. However, in the context of SARS-CoV-2 infection, they are attributed to an olfactory malfunction or neurological impairment [35]. Taste damage results in dysgeusia and ageusia mainly due to an underlying olfactory disturbance, but sometimes primary taste impairment may occur in the context of COVIDjav-19 [36]. The distribution of oral microbiota equilibrium caused by systemic drugs used in COVID-19 may also have a role in oral manifestations and, in particular, halitosis [37]. The pathophysiology of tongue color changes can be microcirculation damage, decreased arterial pressure of oxygen, and increased platelet aggregation [22].
Moreover, the yellow discoloration of the tongue can be attributed to fever and infection, which is correlated with lung damage severity [38]. Furthermore, the tongue’s greasy coatings may indicate either damage to the free oxygen radicals scavenger system or dysbiosis, which latter is a decrease in the levels of Lactobacillus and Bifidobacterium [39]. Besides, the tongue’s tenderness reflects organ failure within the context of a systemic disease, such as COVID-19 [40]. It should be noted that all oral lesions associated with COVID-19 are related to immunosuppression and physical stress [17].
Management of COVID-19 Patients with Tongue Involvements
Most of the lingual problems and taste disturbances subside spontaneously [41]. Nevertheless, some may need specialized treatment, like immunoglobulin and corticosteroids for the Kawasaki-like disease [42] or antihistamines and corticosteroids for angioedema [13]. BHT management increases hydration, induces salivation, discontinues tobacco or alcohol use, and other predisposing factors [43]. If ineffective, gentle tongue cleaning with a brush, topical retinoids or salicylic acid, keratolytic agents, or surgical excision may be curative [44].
Conclusion
The current COVID-19 pandemic is unique because of the diverse multi-organ manifestations it has presented. Taste disturbances and tongue changes are among the various characteristics of SARS-CoV-2 infection. Therefore, because oral complaints are relatively common in COVID-19 patients, an intraoral examination should be conducted in all suspected cases of SARS-CoV-2 infection.
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Javanian M, Bayani M, Shokri M et al (2020) Clinical and laboratory findings from patients with COVID-19 pneumonia in Babol North of Iran: a retrospective cohort study. Rom J Intern Med 58:161–167
Javanian M, Masrour-Roudsari J, Bayani M, Ebrahimpour S (2020) Coronavirus disease 2019 (COVID-19): What we need to know. Casp J Intern Med 11(2):18
Afshar ZM, Ebrahimpour S, Javanian M, Koppolu V, Vasigala VK, Hasanpour AH, Babazadeh A (2020) Coronavirus disease 2019 (COVID-19), MERS and SARS: similarity and difference. J Acute Dis 9(5):194
Amorim dos Santos J, Normando A, Carvalho da Silva R, Acevedo A, De Luca Canto G, Sugaya N et al (2021) Oral manifestations in patients with COVID-19: a living systematic review. J Dent Res 100(2):141–154
Vaira LA, Salzano G, De Riu G (2020) The importance of olfactory and gustatory disorders as early symptoms of coronavirus disease (COVID-19). Br J Oral Maxillofac Surg 58(5):615–616
Millsop JW, Wang EA, Fazel N (2017) Etiology, evaluation, and management of xerostomia. Clin Dermatol 35(5):468–476
Pedrosa MDS, Sipert CR, Nogueira FN (2020) Salivary glands, saliva and oral findings in COVID-19 infection. Pesquisa Brasileira em Odontopediatria e Clínica Integrada 20
Biadsee A, Biadsee A, Kassem F, Dagan O, Masarwa S, Ormianer Z (2020) <? covid19?> Olfactory and Oral Manifestations of COVID-19: sex-related symptoms—a potential pathway to early diagnosis. Otolaryngol Head Neck Surg 163(4):722–728
Yan CH, Faraji F, Prajapati DP, Boone CE, DeConde AS (eds) (2020) Association of chemosensory dysfunction and Covid‐19 in patients presenting with influenza‐like symptoms. International forum of allergy & rhinology. Wiley Online Library
Soares CD, de Carvalho RA, de Carvalho KA, de Carvalho MGF, de Almeida OP (2020) Letter to Editor: oral lesions in a patient with Covid-19. Medicina Oral, Patologia Oral y Cirugia Bucal 25(4):e563
Iranmanesh B, Khalili M, Amiri R, Zartab H, Aflatoonian M (2020) Oral manifestations of COVID‐19 disease: a review article. Dermatol Ther e14578
Viner RM, Whittaker E (2020) Kawasaki-like disease: emerging complication during the COVID-19 pandemic. Lancet 395(10239):1741–1743
Azmy V, Benson J, Love K, Steele R (2020) Idiopathic nonhistaminergic acquired angioedema in a patient with COVID-19. Ann Allergy Asthma Immunol
Taşlıdere B, Mehmetaj L, Özcan AB, Gülen B, Taşlıdere N (2020) Melkersson-Rosenthal syndrome induced by COVID-19: a case report. Am J Emerg Med
Scully C. Medicina oral e maxilofacial: Elsevier Brasil; 2011.
Scully CC (2003) Drug effects on salivary glands: dry mouth. Oral Dis 9(4):165–176
Díaz Rodríguez M, Jimenez Romera A, Villarroel M (2020) Oral manifestations associated with COVID‐19. Oral Dis
Riad A, Gad A, Hockova B, Klugar M (2020) Oral candidiasis in non‐severe COVID‐19 patients: call for antibiotic stewardship. Oral Surg
Gomes SF, Esteves MCL (2012) Atuação do cirurgião-dentista na UTI: um novo paradigma. Rev Bras Odontol 69(1):67
Liang K, Huang X, Chen H, Qiu L, Zhuang Y, Zou C et al (2020) Tongue diagnosis and treatment in traditional Chinese medicine for severe COVID-19: a case report. Ann Palliat Med
Shu Z, Zhou Y, Chang K, Liu J, Min X, Zhang Q et al (2020) Clinical features and the traditional Chinese medicine therapeutic characteristics of 293 COVID-19 inpatient cases. Front Med 1–16
Pang W, Zhang D, Zhang J, Li N, Zheng W, Wang H et al (2020) Tongue features of patients with coronavirus disease 2019: a retrospective cross-sectional study. Integr Med Res 9(3):100493
McGrath EE, Bardsley P, Basran G (2008) Black hairy tongue: what is your call? CMAJ 178(9):1137–1138
Lavric CE, Dumitrescu SV (2018) Black hairy tongue due to antibiotic intake. RJMM 121(3):61
Tamam L, Annagur BB (2006) Black hairy tongue associated with olanzapine treatment. Mt Sinai J Med 73(6):891–894
Nisa L, Giger R (2011) Black hairy tongue. Am J Med 124(9):816–817
Khasawneh FA, Moti DF, Zorek JA (2013) Linezolid-induced black hairy tongue: a case report. J Med Case Rep 7(1):1–4
Giri VP, Datta D, Devi P (2017) Olanzapine-induced black hairy tongue: a rare case. Int J Basic Clin Pharmacol 6(8):2091
Del Barrio-Díaz P, Meza-Romero R, Vera-Kellet C (2017) Black hairy tongue. J Gen Intern Med 32(11):1266
Rajarammohan K, Narayanan M, Ravikumar P, Fenn SM, Gokulraj S (2020) Hairy Tongue—a series of 4 cases. J Evol Med Dent Sci 9(35):2567–2571
Wang Z, Zhou J, Marshall B, Rekaya R, Ye K, Liu H-X (2020) SARS-CoV-2 receptor ACE2 is enriched in a subpopulation of mouse tongue epithelial cells in nongustatory papillae but not in taste buds or embryonic oral epithelium. ACS Pharmacol Transl Sci 3(4):749–758
Riad A, Kassem I, Hockova B, Badrah M, Klugar M (2020) Halitosis in COVID‐19 patients. Special Care Dent
Farshidfar N, Hamedani S (2020) Hyposalivation as a potential risk for SARS‐CoV‐2 infection: inhibitory role of saliva. Oral Dis
Babu S, Rajesh E, Malathi L, Babu NA, Masthan K (2019) Xerostomia-causes, diagnosis and management—a review. Indian J Public Health Res Dev 10(11)
Fantozzi PJ, Pampena E, Di Vanna D, Pellegrino E, Corbi D, Mammucari S et al (2020) Xerostomia, gustatory and olfactory dysfunctions in patients with COVID-19. Am J Otolaryngol 41(6):102721
Vinayachandran D, Balasubramanian S (2020) Is gustatory impairment the first report of an oral manifestation in COVID‐19? Oral Dis
Dziedzic A, Wojtyczka R (2020) The impact of coronavirus infectious disease 19 (COVID‐19) on oral health. Oral Dis
周耿标, 黄东晖, 蔡彦, 黄凯锋, 谢东平 (2020) Relationship between tongue features and clinical classification of patients with novel coronavirus pneumonia. 中医杂志
Mousquer CR, Della Bona A, Milani DC, Callegari-Jacques SM, Ishikawa K, Mayer MPA et al (2020) Are Lactobacillus salivarius G60 and inulin more efficacious to treat patients with oral halitosis and tongue coating than the probiotic alone and placebo? A randomized clinical trial. J Periodontol 91(6):775–783
Abdul MSM, Fatima U, Khanna SS, Bhanot R, Sharma A, Srivastava AP (2020) Oral manifestations of Covid-19-are they the introductory symptoms? J Adv Med Dent Sci Res 8(5):41–43
Boscolo-Rizzo P, Polesel J, Spinato G, Fabbris C, Calvanese L, Menegaldo A et al (2020) Predominance of an altered sense of smell or taste among long-lasting symptoms in patients with mildly symptomatic COVID-19. Rhinology
Elias MD, McCrindle BW, Larios G, Choueiter NF, Dahdah N, Harahsheh AS et al (2020) Management of multisystem inflammatory syndrome in children associated with COVID-19: a survey from the International Kawasaki Disease Registry. CJC Open 2(6):632–640
Cariati P, Aporta LM, Martinez MAJ (2019) Lengua negra vellosa. Manejo clínico. Black hairy tongue. Clin Manag EMERGENCIAS 31(4)
Handler MZ, Butler DF, Eisen D, Burgess J, Lynch DP, Stafford GL (2017) Hairy tongue
Acknowledgements
The authors thank the Clinical Research Development Center of Imam Reza Hospital, Kermanshah University of Medical Sciences, and the Infectious Diseases and Tropical Medicine Research Center of Babol University of Medical Sciences.
Author information
Authors and Affiliations
Contributions
ZMA and AB were involved in review concepts, design, and critical revision for important intellectual content. MB, BS, AJ, and SE performed the literature search and drafted the manuscript. MB and AB were involved in critical revision of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
All authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mohseni Afshar, Z., Barary, M., Ebrahimpour, S. et al. Pathophysiology and Management of Tongue Involvement in COVID-19 Patients. Indian J Otolaryngol Head Neck Surg 74 (Suppl 2), 3235–3238 (2022). https://doi.org/10.1007/s12070-021-03052-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-021-03052-3