Abstract
Haemoptysis is a frequently encountered presentation in thoracic surgery practice. Most of the patients present with chronic haemoptysis while 5% of them will present with life-threatening acute haemoptysis. Emergency surgery used to be the first-line management in acute life-threatening haemoptysis which resulted in significant morbidity and mortality. With advancements in interventional procedures, most of these acute presentations are now being managed conservatively by interventionists. In a country like India with a high incidence of tuberculosis and other infectious diseases of the lungs, haemoptysis is even more common. While interventional procedures help to tide over the crisis and earn valuable time to stabilise a haemorrhaging patient, surgical resection is the definitive management most of the time. This review will endeavour to establish the definition, aetiology, emergency, and definitive management of a patient who presents with haemoptysis.







Similar content being viewed by others
References
Dweik RA, Stoller JK. Role of bronchoscopy in massive hemoptysis. Clin Chest Med. 1999;20:89–105. https://doi.org/10.1016/s0272-5231(05)70129-5.
Jin F, Li Q, Bai C, Wang H, Li S, Song Y, et al. Chinese Expert recommendation for diagnosis and treatment of massive hemoptysis. Respiration. 2020;99:83–92. https://doi.org/10.1159/000502156.
Radchenko C, Alraiyes AH, Shojaee S. A systematic approach to the management of massive hemoptysis. J Thorac Dis. 2017;9:S1069–S1086. https://doi.org/10.21037/jtd.2017.06.41.
Ibrahim WH. Massive haemoptysis: the definition should be revised. Eur Respir J. 2008;32:1131–2. https://doi.org/10.1183/09031936.00080108.
Prasad R, Garg R, Singhal S, Srivastava P. Lessons from patients with hemoptysis attending a chest clinic in India. Ann Thorac Med. 2009;4:10–2. https://doi.org/10.4103/1817-1737.43062.
Bhalla A, Pannu AK, Suri V. Etiology and outcome of moderate-to-massive hemoptysis: experience from a tertiary care center of North India. Int J Mycobacteriol. 2017;6:307–10. https://doi.org/10.4103/ijmy.ijmy_54_17.
Panda A, Bhalla AS, Goyal A. Bronchial artery embolization in hemoptysis: a systematic review. DiagnIntervRadiol. 2017;23:307–17. https://doi.org/10.5152/dir.2017.16454.
Ittrich H, Bockhorn M, Klose H, Simon M. The diagnosis and treatment of hemoptysis. DtschArztebl Int. 2017;114:371–81. https://doi.org/10.3238/arztebl.2017.0371.
Halezeroğlu S, Okur E. Thoracic surgery for haemoptysis in the context of tuberculosis: what is the best management approach? J Thorac Dis. 2014;6:182–5. https://doi.org/10.3978/j.issn.2072-1439.2013.12.25.
Sameer M, David N, Rao VM, Benjamin SR, Gnanamuthu BR, Mohammad A, et al. Surgical management of pulmonary aspergilloma-12 years’ experience from a tertiary care centre in India. Indian J Thorac Cardiovasc Surg. 2021;37:402–10. https://doi.org/10.1007/s12055-021-01181-6.
Benjamin SR, Narayanan D, Chandy ST, Gnanamuthu BR, Michael JS, Kodiatte TA. Pulmonary mucormycosis-a case series. Indian J Thorac Cardiovasc Surg. 2022;38:177–82. https://doi.org/10.1007/s12055-021-01272-4.
Singh SK, Tiwari KK. Etiology of hemoptysis: a retrospective study from a tertiary care hospital from northern Madhya Pradesh, India Indian J Tuberc. 2016;63:44–7. https://doi.org/10.1016/j.ijtb.2016.02.007.
Fink G, Krelbaum T, Yellin A, Bendayan D, Saute M, Glazer M, et al. Pulmonary carcinoid: presentation, diagnosis, and outcome in 142 cases in Israel and review of 640 cases from the literature. Chest. 2001;119:1647–51. https://doi.org/10.1378/chest.119.6.1647.
Gershman E, Guthrie R, Swiatek K, Shojaee S. Management of hemoptysis in patients with lung cancer. Ann Transl Med. 2019;7:358. https://doi.org/10.21037/atm.2019.04.91.
Kitamura N, Ojima T. Peripheral pulmonary hamartoma with haemoptysis from the non-adjacent bronchus. Respirol Case Rep. 2020;8:e00553. https://doi.org/10.1002/rcr2.553.
Liu J, Tian B, Zeng Q, Chen C, Zhou C, Li H, et al. Mediastinal teratoma presenting with hemoptysis and pleuritis misdiagnosed as tuberculosis (empyema). BMC Pediatr. 2018;18:382. https://doi.org/10.1186/s12887-018-1357-7.
Mohammad A, Benjamin SR, Mallampati S, Gnanamuthu BR. Hydatid necessitans—an unusual entity. JTCVS Techniques,2022 (ONLINE). https://doi.org/10.1016/j.xjtc.2022.03.010.
Mohammad A, Benjamin SR, Narayanan D, Rao VM, Malampati S, Andugala SS, et al. Thoracic hydatid cysts: an analysis of surgical management in a tertiary care centre in India. Indian J Thorac Cardiovasc Surg. 2022;38: 17–27. https://doi.org/10.1007/s12055-021-01294-y.
Jean-Baptiste E. Clinical assessment and management of massive hemoptysis. Crit Care Med. 2000;28:1642–7. https://doi.org/10.1097/00003246-200005000-00066.
Gagnon S, Quigley N, Dutau H, Delage A, Fortin M. Approach to hemoptysis in the modern era. Can Respir J. 2017;2017:1565030. https://doi.org/10.1155/2017/1565030.
Davidson K, Shojaee S. Managing massive hemoptysis. Chest. 2020;157:77–88. https://doi.org/10.1016/j.chest.2019.07.012.
Son JH, Kim DH, Lee SK. Successful use of an EZ-blocker for lung isolation and management in a hemoptysis patient. Ann Transl Med. 2019;7:701.
Revel MP, Fournier LS, Hennebicque AS, Cuenod CA, Meyer G, Reynaud P, et al. Can CT replace bronchoscopy in the detection of the site and cause of bleeding in patients with large or massive hemoptysis?. AJR Am J Roentgenol. 2002;179:1217–1224. https://doi.org/10.2214/ajr.179.5.1791217.
Sakr L, Dutau H. Massive hemoptysis: an update on the role of bronchoscopy in diagnosis and management. Respiration. 2010;80:38–58.
Andréjak C, Parrot A, Bazelly B, Ancel PY, Djibré M, Khalil A, et al. Surgical lung resection for severe hemoptysis. Ann Thorac Surg. 2009;88:1556–65.
Cordovilla R, Bollo de Miguel E, Nuñez Ares A, Cosano Povedano FJ, Herráez Ortega I, Jiménez Merchán R. Diagnosis and treatment of hemoptysis. Arch Bronconeumol. 2016;52:368–77.
Conlan AA, Hurwitz SS. Management of massive haemoptysis with the rigid bronchoscope and cold saline lavage. Thorax. 1980;35:901–4.
Prutsky G, Domecq JP, Salazar CA, Accinelli R. Antifibrinolytic therapy to reduce haemoptysis from any cause. Cochrane Tobacco Addiction Group, editor. Cochrane Database Syst Rev [Internet]. 2016 Nov 2 [cited 2022 Jun 26];2016(11). Available from: https://doi.org/10.1002/14651858.CD008711.pub3.
Myers SP, Kutcher ME, Rosengart MR, Sperry JL, Peitzman AB, Brown JB, et al. Tranexamic acid administration is associated with an increased risk of posttraumatic venous thromboembolism. J Trauma Acute Care Surg. 2019;86:20–7.
Taeuber I, Weibel S, Herrmann E, Neef V, Schlesinger T, Kranke P, et al. Association of intravenous tranexamic acid with thromboembolic events and mortality: a systematic review, meta-analysis, and meta-regression. JAMA Surg. 2021;156: e210884.
Steinfort DP, Herth FJF, Eberhardt R, Irving LB. Potentially fatal arrhythmia complicating endobronchial epinephrine for control of iatrogenic bleeding. Am J Respir Crit Care Med. 2012;185:1028–30.
Dutau H, Palot A, Haas A, Decamps I, Durieux O. Endobronchial embolization with a silicone spigot as a temporary treatment for massive hemoptysis: a new bronchoscopic approach of the disease. Respiration. 2006;73:830–2.
Valipour A, Kreuzer A, Koller H, Koessler W, Burghuber OC. Bronchoscopy-guided topical hemostatic tamponade therapy for the management of life-threatening hemoptysis. Chest. 2005;127:2113–8.
Chawla RK, Madan A, Mehta D, Chawla A. Glue therapy in hemoptysis: a new technique. Lung India. 2012;29:293-4.
de Gracia J, de la Rosa D, Catalán E, Alvarez A, Bravo C, Morell F. Use of endoscopic fibrinogen–thrombin in the treatment of severe hemoptysis. Respir Med. 2003;97:790–5.
Dumon JF, Reboud E, Garbe L, Aucomte F, Meric B. Treatment of tracheobronchial lesions by laser photoresection. Chest. 1982;81:278–84.
Shepherd RW, Radchenko C. Bronchoscopic ablation techniques in the management of lung cancer. Ann Transl Med. 2019;7:362.
Morice RC, Ece T, Ece F, Keus L. Endobronchial argon plasma coagulation for treatment of hemoptysis and neoplastic airway obstruction. Chest. 2001;119:781–7.
Zeng J, Wu X, Zhang M, Lin L, Ke M. Modified silicone stent for difficult-to-treat massive hemoptysis: a pilot study of 14 cases. J Thorac Dis. 2020;12:956–65.
Lalla U, Allwood BW, Sinha Roy S, Irusen EM, Koegelenberg CFN. Endobronchial valve used as salvage therapy in a mechanically ventilated patient with intractable life-threatening haemoptysis. Respiration. 2017;93:436–40.
Batra H, Yarmus L. Indications and complications of rigid bronchoscopy. Expert Rev Respir Med. 2018;12:509–20.
Fartoukh M, Demoule A, Sanchez O, Tuffet S, Bergot E, Godet C, et al. Randomised trial of first-line bronchial artery embolisation for non-severe haemoptysis of mild abundance. BMJ Open Respir Res. 2021;8: e000949.
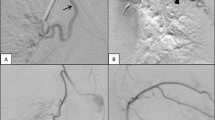
Zheng Z, Zhuang Z, Yang M, Luo J, Zhang W, Yan Z, et al. Bronchial artery embolization for hemoptysis: a systematic review and meta-analysis. J Interv Med. 2021;4:172–80.
Yoo DH, Yoon CJ, Kang SG, Burke CT, Lee JH, Lee CT. Bronchial and nonbronchial systemic artery embolization in patients with major hemoptysis: safety and efficacy of N-butyl cyanoacrylate. AJR Am J Roentgenol. 2011;196:W199-204.
Cauldwell EW, Siekert RG. The bronchial arteries; an anatomic study of 150 human cadavers. Surg Gynecol Obstet. 1948;86:395–412.
Osiro S, Wear C, Hudson R, Ma XX, Zurada A, Michalak M, et al. A friend to the airways: a review of the emerging clinical importance of the bronchial arterial circulation. Surg Radiol Anat. 2012;34:791–8.
McDonald DM. Angiogenesis and remodeling of airway vasculature in chronic inflammation. Am J Respir Crit Care Med. 2001;164:S39-45.
Yoon W, Kim JK, Kim YH, Chung TW, Kang HK. Bronchial and nonbronchial systemic artery embolization for life-threatening hemoptysis: a comprehensive review. Radiographics. 2002;22:1395–409.
Chan VL, So LK, Lam JY, Lau KY, Chan CS, Lin AW, et al. Major haemoptysis in Hong Kong: aetiologies, angiographic findings and outcomes of bronchial artery embolisation. Int J Tuberc Lung Dis. 2009;13:1167–73.
Ishikawa H, Ohbe H, Omachi N, Morita K, Yasunaga H. Spinal cord infarction after bronchial artery embolization for hemoptysis: a nationwide observational study in Japan. Radiology. 2021;298:673–9.
Dewan RK. Surgery for pulmonary tuberculosis - a 15-year experience. Eur J Cardiothorac Surg. 2010;37:473–7. https://doi.org/10.1016/j.ejcts.2009.08.026.
David N, Chandy ST, Benjamin SR, Mohammad A, Mallampati S, Kodiatte TA, et al. Pulmonary sclerosing pneumocytoma-a case series. Indian J Thorac Cardiovasc Surg. 2022;38:167–172. https://doi.org/10.1007/s12055-021-01269-z.
Prasad R, Garg R, Verma SK. Intralobar sequestration of lung. Lung India. 2009;26:159–61. https://doi.org/10.4103/0970-2113.56357.
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. The manuscript was written by Santhosh Regini Benjamin, Avinash Anil Nair, and Raj Kumar Joel. The surgeries were done by Birla Roy Gnanamuthu, Vinay Murahari Rao, Shalom Sylvester Andugala, and Santhosh Regini Benjamin. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The approval of the institutional review board is not required.
Informed consent
Written consent for studies and publication were obtained from the patients prior to the surgery, bronchoscopy, or BAE.
Human and animal rights
The study has been performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Conflict of interest
There was no conflict of interest in this study.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Presentation at a meeting
The manuscript is original and has not been submitted to any other journal for simultaneous consideration and never been published elsewhere in any form or language.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Benjamin, S.R., Nair, A.A., Joel, R.K. et al. An overview on the principles of management of haemoptysis. Indian J Thorac Cardiovasc Surg 39, 505–515 (2023). https://doi.org/10.1007/s12055-023-01547-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12055-023-01547-y