Abstract
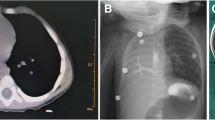
Congenital lung and foregut malformations have been described in literature, but most articles are from the Western world. There are a separate set of problems which are faced in our country especially with the misdiagnosis of these problems which has not so much been addressed in writing. We retrospectively reviewed records of all patients with above thoracic lesions treated at a tertiary care hospital in Delhi from March 2017 to December 2019. Twenty patients were found. Eight of 20 patients were detected antenatally but none monitored serially. Age at presentation ranged from 5 days to 18 months. Eight patients presented with respiratory distress at birth. Three of these were congenital lobar emphysema wrongly diagnosed as pneumothorax and brought with intercostal drainage tube inserted. Eight suffered from pneumonia, 4 of which had history of previous hospital admission but undetected congenital pathology. All underwent surgery and had good outcome. There was radiological evidence of compensatory lung growth in all patients at 6 months follow-up. Thus, we conclude that the antenatal detection of congenital lung and foregut malformations may have increased but proper serial monitoring is still missing. There is scope of increasing index of suspicion for these lesions among pediatricians and surgeons. With modern-day safe anesthesia, proactive resection of congenital lung and foregut malformations is associated with good outcome. Delaying treatment predisposes the child to infective complications and makes surgery difficult.



Similar content being viewed by others
References
Andrade CF, da Costa Ferreira HP, Fischer GB. Congenital lung malformations. J Bras Pneumol. 2011;37:259–71. https://doi.org/10.1590/S1806-37132011000200017
Yong PJ, Von Dadelszen P, Carpara D, et al. Prediction of pediatric outcome after prenatal diagnosis and expectant antenatal management of congenital cystic adenomatoid malformation. Fetal Diagn Ther. 2012;31:94–102. https://doi.org/10.1159/000331936
Gulla KM, Parihar MS, Jat KR, Agarwala S, Lodha R, Kabra SK. Congenital lung malformations: experience from a tertiary care center in India. Indian Pediatr. 2021;58:129–33.
Bush A. Rare lung diseases: congenital malformations. Indian J Pediatr. 2015;82:833–40. https://doi.org/10.1007/s12098-015-1800-9
Calvert JK, Lakhoo K. Antenatally suspected congenital cystic adenomatoid malformation of the lung: postnatal investigation and timing of surgery. J Pediatr Surg. 2007;42:411–4. https://doi.org/10.1016/j.jpedsurg.2006.10.015
Annunziata F, Bush A, Borgia F, et al. Congenital lung malformations: unresolved issues and unanswered questions. Front Pediatr. 2019;7:239. https://doi.org/10.3389/fped.2019.00239
Montella S, Corcione A, Santamaria F. Recurrent pneumonia in children: a reasoned diagnostic approach and a single centre experience. Int J Mol Sci. 2017;18:296. https://doi.org/10.3390/ijms18020296
Seear M, Townsend J, Hoepker A, et al. A review of congenital lung malformations with a simplified classification system for clinical and research use. Pediatr Surg Int. 2017;33:657–64. https://doi.org/10.1007/s00383-017-4062-y
Sueyoshi R, Okazaki T, Urushihara N, et al. Managing prenatally diagnosed asymptomatic congenital cystic adenomatoid malformation. Pediatr Surg Int. 2008;24:1111–5. https://doi.org/10.1007/s00383-008-2227-4
Criss CN, Musili N, Matusko N, Baker S, Geiger JD, Kunisaki SM. Asymptomatic congenital lung malformations: is nonoperative management a viable alternative? J Pediatr Surg. 2018;53:1092–7. https://doi.org/10.1016/j.jpedsurg.2018.02.065
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
Ethical approval was waived by the local Ethics Committee of University in view of the retrospective nature of the study and all the procedures being performed were part of the routine care.
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Informed consent
Not applicable (retrospective analysis of all collected data from patient records, all procedures performed were a part of routine care).
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Singh, V., Shoor, G., Acharya, S.K. et al. Spectrum of congenital lung and foregut malformations: scope for awareness and prompt management—a case series. Indian J Thorac Cardiovasc Surg 38, 307–311 (2022). https://doi.org/10.1007/s12055-021-01300-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12055-021-01300-3