Abstract
Background
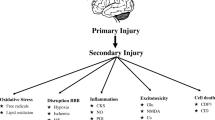
Traumatic brain injury (TBI) can cause rapid brain inflammation. There is debate over the safety and efficacy of anti-inflammatory agents in its treatment. With a particular focus on cyclooxygenase 2 (COX2) selective inhibition, we sought to determine the impact of celecoxib versus no celecoxib treatment on outcomes in patients with TBI and compare these with outcomes associated with nonselective COX inhibition (ibuprofen) and corticosteroid (dexamethasone) treatment.
Methods
This retrospective cohort study used TriNetX, a large publicly available global health research network, to gather clinical data extracted from the electronic medical records. Using International Classification of Diseases, Tenth Revision and pharmacy codes, we identified patients with TBI who were and were not treated with celecoxib, ibuprofen, and dexamethasone. Analysis was performed on propensity-matched and unmatched cohorts, which were matched on demographics, comorbidities, and neurological injuries. Our primary end point was 1-year survival. Secondary end points were ventilator and tracheostomy dependence, gastrostomy tube placement, seizures, and craniotomy.
Results
After propensity score matching, a total of 1443 patients were identified in both the celecoxib and no celecoxib cohorts. Ninety-two (6.4%) patients in the celecoxib cohort died within 1 year following TBI versus 145 (10.0%) in the no celecoxib cohort (odds ratio 0.61; 95% confidence interval 0.46–0.80; p = 0.0003). The 1-year survival rate was 96.1% in the celecoxib cohort versus 93.1% in the no celecoxib cohort (p < 0.0001). At the end of the 1-year period, celecoxib was associated with significantly lower gastrostomy tube dependence (p = 0.017), seizure activity (p = 0.027), and myocardial infarction (p = 0.021) compared with the control cohort. Ibuprofen was also associated with higher 1-year survival probability and lower rates of post-TBI complications. Dexamethasone was broadly associated with higher morbidity but was associated with higher 1-year survival probability compared with the no dexamethasone cohort.
Conclusions
Early celecoxib and ibuprofen use within 5 days post TBI was associated with higher 1-year survival probabilities and fewer complications. With emerging yet controversial preclinical evidence to suggest that COX inhibition improves TBI outcomes, this population-level study offers suggestive support for these drugs’ clinical benefit, which should be pursued in prospective clinical studies.



Similar content being viewed by others
References
Simon DW, McGeachy MJ, Bayır H, Clark RSB, Loane DJ, Kochanek PM. The far-reaching scope of neuroinflammation after traumatic brain injury. Nat Rev Neurol. 2017;13(9):572. https://doi.org/10.1038/nrneurol.2017.116.
Pearn ML, Niesman IR, Egawa J, et al. Pathophysiology associated with traumatic brain injury: current treatments and potential novel therapeutics. Cell Mol Neurobiol. 2017;37(4):571–85. https://doi.org/10.1007/s10571-016-0400-1.
Rodney T, Osier N, Gill J. Pro- and anti-inflammatory biomarkers and traumatic brain injury outcomes: a review. Cytokine. 2018;110:248–56. https://doi.org/10.1016/j.cyto.2018.01.012.
Webster KM, Sun M, Crack P, O’Brien TJ, Shultz SR, Semple BD. Inflammation in epileptogenesis after traumatic brain injury. J Neuroinflammation. 2017;14(1):10. https://doi.org/10.1186/s12974-016-0786-1.
Hickey RW, Adelson PD, Johnnides MJ, et al. Cyclooxygenase-2 activity following traumatic brain injury in the developing rat. Pediatr Res. 2007;62(3):271–6. https://doi.org/10.1203/PDR.0b013e3180db2902.
Bergold PJ. Treatment of traumatic brain injury with anti-inflammatory drugs. Exp Neurol. 2016;275(Pt 3):367–80. https://doi.org/10.1016/j.expneurol.2015.05.024.
Russo MV, McGavern DB. Inflammatory neuroprotection following traumatic brain injury. Science. 2016;353(6301):783–5. https://doi.org/10.1126/science.aaf6260.
Levant S, Chari K, DeFrances C. National hospital care survey demonstration projects: traumatic brain injury. Natl Health Stat Report. 2016;97:1–16.
Tardif PA, Moore L, Boutin A, et al. Hospital length of stay following admission for traumatic brain injury in a Canadian integrated trauma system: a retrospective multicenter cohort study. Injury. 2017;48(1):94–100. https://doi.org/10.1016/j.injury.2016.10.042.
Chaudhry R, Kukreja N, Tse A, et al. Trends and outcomes of early versus late percutaneous endoscopic gastrostomy placement in patients with traumatic brain injury: nationwide population-based study. J Neurosurg Anesthesiol. 2018;30(3):251–7. https://doi.org/10.1097/ANA.0000000000000434.
Robba C, Galimberti S, Graziano F, et al. Tracheostomy practice and timing in traumatic brain-injured patients: a CENTER-TBI study. Intensive Care Med. 2020;46(5):983–94. https://doi.org/10.1007/s00134-020-05935-5.
Harhangi BS, Kompanje EJ, Leebeek FW, Maas AI. Coagulation disorders after traumatic brain injury. Acta Neurochir (Wien) 2008;150(2):165–75; discussion 175. https://doi.org/10.1007/s00701-007-1475-8.
Edwards P, Arango M, Balica L, et al. Final results of MRC CRASH, a randomised placebo-controlled trial of intravenous corticosteroid in adults with head injury-outcomes at 6 months. Lancet. 2005;365(9475):1957–9. https://doi.org/10.1016/S0140-6736(05)66552-X.
Hawryluk GWJ, Rubiano AM, Totten AM, et al. Guidelines for the management of severe traumatic brain injury: 2020 update of the decompressive craniectomy recommendations. Neurosurgery. 2020;87(3):427–34. https://doi.org/10.1093/neuros/nyaa278.
Keshavarzi Z, Khaksari M, Razmi Z, Soltani Hekmat A, Naderi V, Rostami S. The effects of cyclooxygenase inhibitors on the brain inflammatory response following traumatic brain injury in rats. Iran J Basic Med Sci. 2012;15(5):1102–5.
Dash PK, Mach SA, Moore AN. Regional expression and role of cyclooxygenase-2 following experimental traumatic brain injury. J Neurotrauma. 2000;17(1):69–81. https://doi.org/10.1089/neu.2000.17.69.
Hiskens M, Vella R, Schneiders A, Fenning A. Celecoxib in a preclinical model of repetitive mild traumatic brain injury: hippocampal learning deficits persist with inflammatory and excitotoxic neuroprotection. Trauma Care. 2021;1(1):23–37. https://doi.org/10.3390/traumacare1010003.
Hakan T, Toklu HZ, Biber N, et al. Effect of COX-2 inhibitor meloxicam against traumatic brain injury-induced biochemical, histopathological changes and blood-brain barrier permeability. Neurol Res. 2010;32(6):629–35. https://doi.org/10.1179/016164109X12464612122731.
Girgis H, Palmier B, Croci N, Soustrat M, Plotkine M, Marchand-Leroux C. Effects of selective and non-selective cyclooxygenase inhibition against neurological deficit and brain oedema following closed head injury in mice. Brain Res. 2013;1491:78–87. https://doi.org/10.1016/j.brainres.2012.10.049.
Dehlaghi Jadid K, Davidsson J, Lidin E, et al. COX-2 inhibition by diclofenac is associated with decreased apoptosis and lesion area after experimental focal penetrating traumatic brain injury in rats. Front Neurol. 2019;10:811. https://doi.org/10.3389/fneur.2019.00811.
Thau-Zuchman O, Shohami E, Alexandrovich AG, Trembovler V, Leker RR. The anti-inflammatory drug carprofen improves long-term outcome and induces gliogenesis after traumatic brain injury. J Neurotrauma. 2012;29(2):375–84. https://doi.org/10.1089/neu.2010.1673.
Gopez JJ, Yue H, Vasudevan R, et al. Cyclooxygenase-2-specific inhibitor improves functional outcomes, provides neuroprotection, and reduces inflammation in a rat model of traumatic brain injury. Neurosurgery. 2005;56(3):590–604. https://doi.org/10.1227/01.neu.0000154060.14900.8f.
Cernak I, O’Connor C, Vink R. Activation of cyclo-oxygenase-2 contributes to motor and cognitive dysfunction following diffuse traumatic brain injury in rats. Clin Exp Pharmacol Physiol. 2001;28(11):922–5. https://doi.org/10.1046/j.1440-1681.2001.03549.x.
Cernak I, O’Connor C, Vink R. Inhibition of cyclooxygenase 2 by nimesulide improves cognitive outcome more than motor outcome following diffuse traumatic brain injury in rats. Exp Brain Res. 2002;147(2):193–9. https://doi.org/10.1007/s00221-002-1245-z.
Karabekir HS, Balci C, Aktepe F, Tokyol C, Dilek H. Which is more effective in reducing secondary brain damage resulting from cyclooxygenase expression following traumatic brain injury: calcium channel blockers or cox inhibitors? Neurosciences (Riyadh). 2008;13(3):239–43.
Schwab JM, Beschorner R, Meyermann R, Gözalan F, Schluesener HJ. Persistent accumulation of cyclooxygenase-1-expressing microglial cells and macrophages and transient upregulation by endothelium in human brain injury. J Neurosurg. 2002;96(5):892–9. https://doi.org/10.3171/jns.2002.96.5.0892.
Shang JL, Cheng Q, Yang WF, Zhang M, Cui Y, Wang YF. Possible roles of COX-1 in learning and memory impairment induced by traumatic brain injury in mice. Braz J Med Biol Res. 2014;47(12):1050–6.
Author information
Authors and Affiliations
Contributions
Conceptualization: DRH, DB, ER, JCZ; methodology: DRH, DB, JS; software: DRH, DB; formal analysis: DRH, DB, JS; investigation: DRH, DB, JS; resources: DRH, DB, JS, JCZ, ER; data curation: DRH; writing (original draft preparation): DRH, DB, JS; writing (review and editing): DRH, ER, JCZ; visualization: DRH, DB, JS; supervision: DRH, ER, JCZ.
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest to disclose.
Ethical Approval/Informed Consent
The authors confirm adherence to ethical guidelines and indicate ethical approvals, including institutional review board policies.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.



Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bhanja, D., Hallan, D.R., Staub, J. et al. Early Celecoxib use in Patients with Traumatic Brain Injury. Neurocrit Care (2023). https://doi.org/10.1007/s12028-023-01827-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12028-023-01827-w