Abstract
Background
It remains a challenge to judge whether comatose patients with acute intracerebral hemorrhage (ICH) can wake up. Here, we aimed to investigate the changes in right ventricle-pulmonary artery (RV-PA) coupling over time in these patients and to evaluate its performance for discriminating between those who woke up within 60 days and those who did not.
Methods
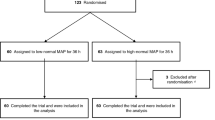
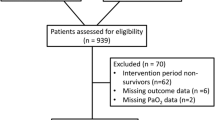
Thirty-five comatose patients with acute spontaneous ICH underwent bedside echocardiography on days 1, 3, and 5 after onset with the measurement of tricuspid annular plane systolic excursion and mean pulmonary artery pressure. The RV-PA coupling (the ratio of tricuspid annular plane systolic excursion to mean pulmonary artery pressure) was calculated.
Results
Within 60 days of the onset of coma, 11 individuals awakened and survived, and 24 individuals died. In awakened patients, RV-PA couplings did not differ among days 1, 3, and 5 (1.62 ± 0.38 vs. 1.61 ± 0.32 vs. 1.64 ± 0.25 mm/mm Hg, P > 0.05), whereas in unawakened patients, they decreased drastically from day 1 to day 3 and then to day 5 (1.26 ± 0.32 vs. 0.63 ± 0.05 vs. 0.43 ± 0.06 mm/mm Hg, P < 0.05). The area under receiver operating characteristic curve of 0.992 for the ratio of RV-PA coupling on day 5 to day 1 of the coma was superior to that for the Glasgow Coma Scale (area under receiver operating characteristic curve of 0.606) in the discrimination of comatose patients with ICH who woke up within 60 days from those who did not. The optimal cutoff value was 0.536, with a sensitivity of 100.00%, a specificity of 96.24%, and an accuracy of 97.13%.
Conclusions
Right ventricle-pulmonary artery coupling demonstrated a high performance for discriminating comatose patients with ICH who woke up within 60 days from those who did not.





Similar content being viewed by others
References
Edlow BL, Claassen J, Schiff ND, Greer DM. Recovery from disorders of consciousness: mechanisms, prognosis and emerging therapies. Nat Rev Neurol. 2021;17(3):135–56.
Larsen AM, Cote DJ, Karhade AV, Smith TR. Predictors of stroke and coma after neurosurgery: an ACS-NSQIP analysis. World Neurosurg. 2016;93:299–305.
Diouf FS, Mapoure NY, Ndiaye M, et al. Prognosis of intracerebral hemorrhage with coma in a neurological critical care unit in the tropics. Med Trop (Mars). 2008;68(6):606–10.
Weidler DJ. Myocardial damage and cardiac arrhythmias after intracranial haemorrhage. A critical review. Stroke. 1974;5(6):759–64.
Ali M, Lyden P, Sacco RL, et al. Natural history of complications after intracerebral haemorrhage. Eur J Neurol. 2009;16(5):624–30.
Xu M, Lin J, Wang D, Liu M, Hao Z, Lei C. Cardiac troponin and cerebral herniation in acute intracerebral hemorrhage. Brain Behav. 2017;7(6): e00697.
Qian R, Yang W, Wang X, Xu Z, Liu X, Sun B. Evaluation of cerebral-cardiac syndrome using echocardiography in a canine model of acute traumatic brain injury. Am J Cardiovasc Dis. 2015;5(1):72–6.
Krishnamoorthy V, Wilson T, Sharma D, Vavilala MS. Prolonged cardiac dysfunction after intraparenchymal hemorrhage and neurogenic stunned myocardium. A A Case Rep. 2016;6(1):3–5.
Rochester CL, Mohsenin V. Respiratory complications of stroke. Semin Respir Crit Care Med. 2002;23(3):248–60.
Sposato LA, Hilz MJ, Aspberg S, et al. Post-stroke cardiovascular complications and neurogenic cardiac injury: JACC state-of-the-art review. J Am Coll Cardiol. 2020;76(23):2768–85.
Putaala J, Lehto M, Meretoja A, et al. In-hospital cardiac complications after intracerebral hemorrhage. Int J Stroke. 2014;9(6):741–6.
Kurian C, Kaur K, Kaur G, et al. Assessment of the patient with intracerebral hemorrhage: a review of the literature. Cardiol Rev. 2021;29(1):20–5.
Johansson K, Jansson JH, Johansson L, et al. D-dimer is associated with first-ever intracerebral hemorrhage. Stroke. 2018;49(9):2034–9.
Zhou Q, Zhang D, Chen X, et al. Plasma D-dimer predicts poor outcome and mortality after spontaneous intracerebral hemorrhage. Brain Behav. 2021;11(1):462–8.
Prins KW, Weir EK, Archer SL, et al. Pulmonary pulse wave transit time is associated with right ventricular-pulmonary artery coupling in pulmonary arterial hypertension. Pulm Circ. 2016;6(4):576–85.
Dabestani A, Mahan G, Gardin JM, et al. Evaluation of pulmonary artery pressure and resistance by pulsed Doppler echocardiography. Am J Cardiol. 1987;59(6):662–8.
Zielinsky P, MagalhÃes GA, Zurita-Peralta J, et al. Improvement of fetal pulmonary hypertension and maturity after reversal of ductal constriction: a prospective cohort study. Ultrasound Obstet Gynecol. 2021;58(3):420–7.
Yip HK, Chang LT, Chang WN, et al. Level and value of circulating endothelial progenitor cells in patients after acute ischemic stroke. Stroke. 2008;39(1):69–74.
Markousis-Mavrogenis G, Sfikakis PP, Mavrogeni SI, Tektonidou MG. Combined brain/heart magnetic resonance imaging in antiphospholipid syndrome-two sides of the same coin. Clin Rheumatol. 2021;40(7):2559–68.
Acknowledgments
The authors gratefully acknowledge the technical assistance of Yan Zhu, Ya-Peng Li, Hong-Ye Wang, Lei Zhang, and Dan Huang from the Department of Ultrasound, Yangpu Hospital, School of Medicine, Tongji University, Shanghai, P.R. China.
Funding
This study was not supported by any financial and material support.
Author information
Authors and Affiliations
Contributions
S-HZ: conceived the project and main conceptual ideas, data acquisition, analysis, and writing of the article. L-NS: data acquisition, analysis, critical review. X-ZZ: conceived the project and main conceptual ideas and planned the study, data acquisition, analysis, result interpretation, study supervision, and took the lead in writing the article. All authors have read and approved of the final manuscript.
Corresponding author
Ethics declarations
Conflicts of Interest
We have no conflict of interest to disclose.
Ethical approval/informed consent
This study adherence to ethical guidelines and has been approved by the Ethics Committee of Yangpu Hospital, School of Medicine, Tongji University (ID: 20190001394).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zong, SH., Sun, LN. & Zheng, XZ. A Simple Echocardiographic Approach in Assessing the Prognosis of Comatose Patients with Acute Intracerebral Hemorrhage by Using Right Ventricle-Pulmonary Artery Coupling. Neurocrit Care 38, 633–639 (2023). https://doi.org/10.1007/s12028-022-01617-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-022-01617-w