Abstract
Background
The objective of this study was to validate the value of the Status Epilepticus Severity Score (STESS) in the prediction of the risk of in-hospital mortality in patients with nonhypoxic status epilepticus (SE) using a machine learning analysis.
Methods
We included consecutive patients with nonhypoxic SE (aged ≥ 16 years) admitted from 2013 to 2021 at the Modena Academic Hospital. A decision tree analysis was performed using in-hospital mortality as a dependent variable and the STESS predictors as input variables. We evaluated the accuracy of STESS in predicting in-hospital mortality using the area under the receiver operating characteristic curve (AUROC) with 95% confidence interval (CI).
Results
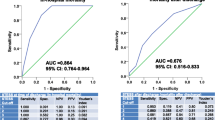
Among 629 patients with SE, the in-hospital mortality rate was 23.4% (147 of 629). The median STESS in the entire cohort was 2.9 (SD 1.6); it was lower in surviving compared with deceased patients (2.7, SD 1.5 versus 3.9, SD 1.6; p < 0.001). Of deceased patients, 82.3% (121 of 147) had scores of 3–6, whereas 17.7% (26 of 147) had scores of 0–2 (p < 0.001). STESS was accurate in predicting mortality, with an AUROC of 0.688 (95% CI 0.641–0.734) only slightly reduced after bootstrap resampling. The most significant predictor was the seizure type, followed by age and level of consciousness at SE onset. Nonconvulsive SE in coma and age ≥ 65 years predicted a higher risk of mortality, whereas generalized convulsive SE and age < 65 years were associated with a lower risk of death. The decision tree analysis using STESS variables correctly classified 90% of survivors and 34% of nonsurvivors after the SE, with an overall risk of error of 23.1%.
Conclusions
This validation study using a machine learning system showed that STESS is a valuable prognostic tool. The score appears particularly accurate and effective in identifying patients who are alive at discharge (high negative predictive value), whereas it has a lower predictive value for in-hospital mortality.


Similar content being viewed by others
Data Availability
On request from qualified investigators, we will share anonymized data.
References
Trinka E, Cock H, Hesdorffer D, et al. A definition and classification of status epilepticus–report of the ILAE task force on classification of status epilepticus. Epilepsia. 2015;56(10):1515–23. https://doi.org/10.1111/epi.13121.
Leitinger M, Trinka E, Zimmermann G, Granbichler CA, Kobulashvili T, Siebert U. Epidemiology of status epilepticus in adults: apples, pears, and oranges - a critical review. Epilepsy Behav. 2020;103(Pt A): 106720. https://doi.org/10.1016/j.yebeh.2019.106720.
Neligan A, Shorvon SD. Frequency and prognosis of convulsive status epilepticus of different causes: a systematic review. Arch Neurol. 2010;67(8):931–40. https://doi.org/10.1001/archneurol.2010.169.
Giovannini G, Monti G, Tondelli M, et al. Mortality, morbidity and refractoriness prediction in status epilepticus: comparison of STESS and EMSE scores. Seizure. 2017;46:31–7. https://doi.org/10.1016/j.seizure.2017.01.004.
Yuan F, Gao Q, Jiang W. Prognostic scores in status epilepticus-a critical appraisal. Epilepsia. 2018;59(Suppl 2):170–5. https://doi.org/10.1111/epi.14483.
Rossetti AO, Logroscino G, Bromfield EB. A clinical score for prognosis of status epilepticus in adults. Neurology. 2006;66(11):1736–8. https://doi.org/10.1212/01.wnl.0000223352.71621.97.
Rossetti AO, Logroscino G, Milligan TA, Michaelides C, Ruffieux C, Bromfield EB. Status epilepticus severity score (STESS): a tool to orient early treatment strategy. J Neurol. 2008;255(10):1561–6. https://doi.org/10.1007/s00415-008-0989-1.
Goyal MK, Chakravarthi S, Modi M, Bhalla A, Lal V. Status epilepticus severity score (STESS): a useful tool to predict outcome of status epilepticus. Clin Neurol Neurosurg. 2015;139:96–9. https://doi.org/10.1016/j.clineuro.2015.09.010.
Pacha MS, Orellana L, Silva E, et al. Role of EMSE and STESS scores in the outcome evaluation of status epilepticus. Epilepsy Behav. 2016;64(Pt A):140–2. https://doi.org/10.1016/j.yebeh.2016.09.036.
Aukland P, Lando M, Vilholm O, Christiansen EB, Beier CP. Predictive value of the status epilepticus severity score (STESS) and its components for long-term survival. BMC Neurol. 2016;16(1):213. https://doi.org/10.1186/s12883-016-0730-0.
González-Cuevas M, Santamarina E, Toledo M, et al. A new clinical score for the prognosis of status epilepticus in adults. Eur J Neurol. 2016;23(10):1534–40. https://doi.org/10.1111/ene.13073.
Sutter R, Kaplan PW, Rüegg S. Independent external validation of the status epilepticus severity score. Crit Care Med. 2013;41(12):e475–9. https://doi.org/10.1097/CCM.0b013e31829eca06.
Leitinger M, Höller Y, Kalss G, et al. Epidemiology-based mortality score in status epilepticus (EMSE). Neurocrit Care. 2015;22(2):273–82. https://doi.org/10.1007/s12028-014-0080-y.
Kang BS, Kim DW, Kim KK, et al. Prediction of mortality and functional outcome from status epilepticus and independent external validation of STESS and EMSE scores. Crit Care. 2016;20:25. https://doi.org/10.1186/s13054-016-1190-z.
Wang P, Guan Y, Lin X, et al. Diagnostic value of status epilepticus severity score for survival conditions of patients with status epilepticus: a PRISMA-compliant systematic review and meta-analysis. Epilepsy Behav. 2018;82:104–10. https://doi.org/10.1016/j.yebeh.2018.02.033.
Leitinger M, Kalss G, Rohracher A, et al. Predicting outcome of status epilepticus. Epilepsy Behav. 2015;49:126–30. https://doi.org/10.1016/j.yebeh.2015.04.066.
Song YY, Lu Y. Decision tree methods: applications for classification and prediction. Shanghai Arch Psychiatry. 2015;27:130–5.
Shirali GA, Noroozi MV, Malehi AS. Predicting the outcome of occupational accidents by CART and CHAID methods at a steel factory in Iran. J Public Health Res. 2018;7:1361.
Brigo F, Turcato G, Lattanzi S, et al. Machine-learning validation through decision-tree analysis of the epidemiology-based mortality score in status epilepticus. Epilepsia. 2022. https://doi.org/10.1111/epi.17372.
Leitinger M, Beniczky S, Rohracher A, et al. Salzburg consensus criteria for non-convulsive status epilepticus–approach to clinical application. Epilepsy Behav. 2015;49:158–63. https://doi.org/10.1016/j.yebeh.2015.05.007.
Leitinger M, Trinka E, Gardella E, et al. Diagnostic accuracy of the Salzburg EEG criteria for non-convulsive status epilepticus: a retrospective study. Lancet Neurol. 2016;15(10):1054–62. https://doi.org/10.1016/S1474-4422(16)30137-5.
Brophy GM, Bell R, Claassen J, et al. Guidelines for the evaluation and management of status epilepticus. Neurocrit Care. 2012;17(1):3–23. https://doi.org/10.1007/s12028-012-9695-z.
Glauser T, Shinnar S, Gloss D, et al. Evidence-based guideline: treatment of convulsive status epilepticus in children and adults: report of the guideline committee of the American epilepsy society. Epilepsy Curr. 2016;16(1):48–61. https://doi.org/10.5698/1535-7597-16.1.48.
Minicucci F, Ferlisi M, Brigo F, et al. Management of status epilepticus in adults position paper of the Italian League against epilepsy. Epilepsy Behav. 2020;102:106675. https://doi.org/10.1016/j.yebeh.2019.106675.
Hajian-Tilaki K. Receiver operating characteristic (ROC) curve analysis for medical diagnostic test evaluation. Caspian J Intern Med. 2013;4(2):627–35.
Park SH, Goo JM, Jo CH. Receiver operating characteristic (ROC) curve: practical review for radiologists. Korean J Radiol. 2004;5(1):11–8.
Turcato G, Zaboli A, Pfeifer N, et al. Decision tree analysis to predict the risk of intracranial haemorrhage after mild traumatic brain injury in patients taking DOACs. Am J Emerg Med. 2021;50:388–93.
Song YY, Lu Y. Decision tree methods: applications for classification and prediction. Shanghai Arch Psychiatry. 2015;27(2):130–5. https://doi.org/10.11919/j.issn.1002-0829.215044.
Shirali GA, Noroozi MV, Malehi AS. Predicting the outcome of occupational accidents by CART and CHAID methods at a steel factory in Iran. J Public Health Res. 2018;7(2):1361. https://doi.org/10.4081/jphr.2018.1361.
Towne AR, Pellock JM, Ko D, DeLorenzo RJ. Determinants of mortality in status epilepticus. Epilepsia. 1994;35(1):27–34. https://doi.org/10.1111/j.1528-1157.1994.tb02908.x.
Logroscino G, Hesdorffer DC, Cascino G, Annegers JF, Hauser WA. Short-term mortality after a first episode of status epilepticus. Epilepsia. 1997;38(12):1344–9. https://doi.org/10.1111/j.1528-1157.1997.tb00073.x.
Koubeissi M, Alshekhlee A. In-hospital mortality of generalized convulsive status epilepticus: a large US sample. Neurology. 2007;69(9):886–93. https://doi.org/10.1212/01.wnl.0000269791.96189.70.
Leitinger M, Trinka E, Giovannini G, et al. Epidemiology of status epilepticus in adults: a population-based study on incidence, causes, and outcomes. Epilepsia. 2019;60(1):53–62. https://doi.org/10.1111/epi.14607.
Logroscino G, Hesdorffer DC, Cascino G, Annegers JF, Hauser WA. Time trends in incidence, mortality, and case-fatality after first episode of status epilepticus. Epilepsia. 2001;42(8):1031–5. https://doi.org/10.1046/j.1528-1157.2001.0420081031.x.
Lattanzi S, Giovannini G, Brigo F, Orlandi N, Trinka E, Meletti S. Status epilepticus with prominent motor symptoms clusters into distinct electroclinical phenotypes. Eur J Neurol. 2021;28(8):2694–9. https://doi.org/10.1111/ene.14891.
Sutter R, Kaplan PW. The neurophysiologic types of nonconvulsive status epilepticus: EEG patterns of different phenotypes. Epilepsia. 2013;54(Suppl 6):23–7.
Sutter R, Semmlack S, Kaplan PW. Nonconvulsive status epilepticus in adults - insights into the invisible. Nat Rev Neurol. 2016;12(5):281–93.
Sutter R. Are we prepared to detect subtle and nonconvulsive status epilepticus in critically Ill patients? J Clin Neurophysiol. 2016;33(1):25–31.
Kinney MO, Craig JJ, Kaplan PW. Hidden in plain sight: Non-convulsive status epilepticus—recognition and management. Acta Neurol Scand. 2017;136:280–92.
Teasdale G, Jennett B. Assessment of coma and impaired consciousness A practical scale. Lancet. 1974;2(7872):81–4. https://doi.org/10.1016/s0140-6736(74)91639-0.
Lattanzi S, Giovannini G, Brigo F, Orlandi N, Trinka E, Meletti S. Clinical phenotypes within nonconvulsive status epilepticus. Epilepsia. 2021;62(9):e129–34. https://doi.org/10.1111/epi.16999.
Semmlack S, Kaplan PW, Spiegel R, et al. Illness severity scoring in status epilepticus-when STESS meets APACHE II, SAPS II, and SOFA. Epilepsia. 2019;60(2):189–200.
Sutter R, Semmlack S, Opić P, et al. Untangling operational failures of the Status Epilepticus Severity Score (STESS). Neurology. 2019;92(17):e1948–56.
Yechoor N, Adeli A, Hafeez S. External validation of the epidemiology-based mortality score in status epilepticus in an American intensive care population. Epilepsy Res. 2018;148:32–6. https://doi.org/10.1016/j.eplepsyres.2018.10.001.
Huang TH, Lai MC, Chen YS, Huang CW. Status epilepticus mortality risk factors and a correlation survey with the newly modified STESS. Healthcare (Basel). 2021;9(11):1570.
Funding
This research received funding from the Italian MOH (“Status epilepticus: improving therapeutic and quality of care intervention in the Emilia-Romagna region”; project code: RF-2016–02,361,365) and by the MIUR (grant “Dipartimenti di eccellenza 2018–2022” to the Department of Biomedical, Metabolic, and Neural Sciences, University of Modena and Reggio-Emilia).
Author information
Authors and Affiliations
Contributions
FB: conceptualization, methodology, original draft preparation. GT: conceptualization, formal analysis, methodology, original draft preparation. SL: methodology, review and editing. NO: data curation, investigation, review and editing. GT: data curation, investigation, review and editing. AZ: methodology, visualization, review and editing. GG: data curation, investigation, review and editing. SM: review and editing, supervision, validation.
Corresponding author
Ethics declarations
Conflicts of interest
None of the authors has any conflicts of interest to disclose.
Ethical Approval/Informed Consent
The study was approved by the local ethical committee (ethics committee approval number 556/2018/OSS/AOUMO–RF‐2016‐02,361,365) and was conducted according to the ethical principles for medical research involving human subjects in the Declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Brigo, F., Turcato, G., Lattanzi, S. et al. Retrospective External Validation of the Status Epilepticus Severity Score (STESS) to Predict In-hospital Mortality in Adults with Nonhypoxic Status Epilepticus: A Machine Learning Analysis. Neurocrit Care 38, 254–262 (2023). https://doi.org/10.1007/s12028-022-01610-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-022-01610-3