Abstract
Background
Traumatic brain injury (TBI) is a major cause of morbidity and mortality in the United States. Older adults represent an understudied and growing TBI population. Current Brain Trauma Foundation guidelines support prophylactic antiseizure medication (ASM) administration to reduce the risk of early posttraumatic seizures (within 7 days of injury) in patients with severe TBI. Whether ASM decreases mortality or early seizure risk in this population remains unclear. This study addresses the knowledge gap regarding the impact of ASM administration on the risk of seizure or mortality after TBI in patients more than 65 years of age.
Methods
This retrospective cohort study used a publicly available data set from the Medical Information Mart for Intensive Care-III from the Massachusetts Institute of Technology. Our cohort included patients 65 years or older with a primary exposure of early ASM administration with TBI resulting in an intensive care unit (ICU) admission in a level I trauma center from 2001 to 2012. A double-robust inverse propensity scale weighted model on the basis of proportional hazard and logistic regression models was created to assess the association between ASM administration and risk of death within 7 days of admission to the ICU. Secondary outcomes included 30-day mortality and 1-year mortality, early posttraumatic seizures, ICU length of stay, and hospital length of stay.
Results
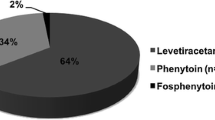
Of 1145 patients 65 years or older with TBI admitted to an ICU, 783 (68.4%) received ASM within the first 24 h. Patients meeting inclusion criteria were predominantly white (83.8%) and were male (52.3%), with a median (interquartile range) age of 81 (74–86) years. TBI severity, classified by Glasgow Coma Score, was predominantly mild (71.2%), followed by moderate (16.8%) and severe (11.3%). Patients who received ASM were less likely to have died at 7 days (adjusted death hazard ratio [HR] = 0.48 [95% confidence interval {CI} 0.28–0.88], P = 0.005), at 30 days (adjusted HR 0.67 [95% CI 0.45–0.99], P = 0.045), and at 1 year (adjusted HR 0.72 [95% CI 0.54–0.97], P = 0.029). Groups were not different in regard to seizure (adjusted seizure odds ratio 1.18 [95% CI 0.61–2.26]) compared with those who did not receive ASM.
Conclusions
Early ASM administration was associated with reduced mortality at 7 days, 30 days, and 1 year but did not decrease the risk of early seizures among older adults who presented with TBI at an ICU. This benefit was observed in mild, moderate, and severe TBI assessed by Glasgow Coma Score on presentation among patients 65 years old and older and suggests broader recommendations for the use of ASM in older adults who present with TBI of any severity at an ICU.



Similar content being viewed by others
References
Rutland-Brown W, Langlois JA, Thomas KE, Xi YL. Incidence of traumatic brain injury in the United States, 2003. J Head Trauma Rehabil. 2006;21(6):544–8.
Ritter AC, Wagner AK, Fabio A, et al. Incidence and risk factors of posttraumatic seizures following traumatic brain injury: a Traumatic Brain Injury Model Systems Study. Epilepsia. 2016;57(12):1968–77.
Vespa PM, Boscardin J, Hovda D, et al. Continuous EEG monitoring in patients with traumatic brain injury as detected by continuous electroencephalographic monitoring. J Neurosurg. 1999;91:750–60.
Ronne-Engstrom E, Winkler T. Continuous EEG monitoring in patients with traumatic brain injury reveals a high incidence of epileptiform activity. Acta Neurol Scand. 2006;114:47–43.
Agrawal A, Timothy J, Pandit L, Manju M. Post-traumatic epilepsy: an overview. Clin Neurol Neurosurg. 2006;108(5):433–9.
Foreman B, Lee H, Mizrahi MA, et al. Seizures and cognitive outcome after traumatic brain injury: a post hoc analysis. Neurocrit Care. 2021. https://doi.org/10.1007/s12028-021-01267-4.
Dhakar MB, Sivakumar S, Bhattacharya P, et al. A retrospective cross-sectional study of the prevalence of generalized status epilepticus in traumatic brain injury: United States 2002–2010. Seizure. 2015;32:16–22.
Temkin NR, Dikmen SS, Wilensky AJ, Keihm J, Chabal S, Winn HR. A randomized, double-blind study of phenytoin for the prevention of post-traumatic seizures. N Engl J Med. 1990;323(8):497–502.
Carney N, Totten AM, O’Reilly C, et al. Guidelines for the management of severe traumatic brain injury. Neurosurgery. 2017;80(1):6–15.
Chang BS, Lowenstein DH. Practice parameter: Antiepileptic drug prophylaxis in severe traumatic brain injury: report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2003;60(1):10–6.
Faul M, Xu L, Wald MM, Coronado V, Dellinger AM. Traumatic brain injury in the United States: national estimates of prevalence and incidence, 2002–2006. Inj Prev. 2010;16(Suppl 1):A268–A268.
Haltiner AM, Newell DW, Temkin NR, Dikmen SS, Winn HR. Side effects and mortality associated with use of phenytoin for early posttraumatic seizure prophylaxis. J Neurosurg. 1999;91(4):588–92. https://doi.org/10.3171/jns.1999.91.4.0588.
Johnson AEW, Pollard TJ, Shen L, et al. MIMIC-III, a freely accessible critical care database. Sci Data. 2016;3(1):160035. https://doi.org/10.1038/sdata.2016.35.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335(7624):806–8.
van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009;47(6):626–33.
Vansteelandt S, Daniel RM. On regression adjustment for the propensity score. Stat Med. 2014;33:4053–72.
R: The R Project for Statistical Computing. https://www.r-project.org/.
Thompson K, Pohlmann-Eden B, Campbell LA, Abel H. Pharmacological treatments for preventing epilepsy following traumatic head injury. Cochrane Database Syst Rev. 2015. https://doi.org/10.1002/14651858.CD009900.pub2.
Glötzner FL, Haubitz I, Miltner F, Kapp G, Pflughaupt KW. Seizure prevention using carbamazepine following severe brain injuries. Neurochirurgia (Stuttg). 1983;26(3):66–79.
Pechadre JC, Lauxerois M, Colnet G, et al. Prevention of late post-traumatic epilepsy by phenytoin in severe brain injuries. 2 years’ follow-up. Presse Med. 1991;20(18):841–5.
Young B, Rapp RP, Norton JA, Haack D, Tibbs PA, Bean JR. Failure of prophylactically administered phenytoin to prevent late posttraumatic seizures. J Neurosurg. 1983;58(2):236–41.
Young KD, Okada PJ, Sokolove PE, et al. A randomized, double-blinded, placebo-controlled trial of phenytoin for the prevention of early posttraumatic seizures in children with moderate to severe blunt head injury. Ann Emerg Med. 2004;43(4):435–46.
Wat R, Mammi M, Paredes J, et al. The effectiveness of antiepileptic medications as prophylaxis of early seizure in patients with traumatic brain injury compared with placebo or no treatment: a systematic review and meta-analysis. World Neurosurg. 2019;122:433–40. https://doi.org/10.1016/j.wneu.2018.11.076.
Khor D, Wu J, Hong Q, et al. Early seizure prophylaxis in traumatic brain injuries revisited: a prospective observational study. World J Surg. 2018;42(6):1727–32.
Funding
There were no sources of funding for this study.
Author information
Authors and Affiliations
Contributions
ACG: acquisition of data, analysis, interpretation, drafting and revision of article, and shared first-authorship. JHK: conception and design, analysis, interpretation, drafting and revision of article, and shared first-authorship. PM-C: statistical analysis, interpretation, and drafting and revision of article. AT: critically revising article and intellectual content. MVA: critically revising article and intellectual content. LB: critically revising article and intellectual content. SS: critically revising article and intellectual content. AP: critically revising article and intellectual content. MDB: conception and design, analysis, interpretation, drafting and revision of the article, and intellectual content. The final manuscript was approved by all authors.
Corresponding author
Ethics declarations
Conflicts of interest
No conflicts of interest to disclose (all authors). Individual disclosures documented and stored with the corresponding author. Available on request.
Ethical Approval/Informed Consent
This retrospective study adheres to ethical guidelines, and use of the Medical Information Mart for Intensive Care-III database was approved by the Institutional Review Boards of the Massachusetts Institute of Technology and Beth Israel Deaconess Medical Center. Access to this database was granted to two of the authors (ACG and JHK).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Glaser, A.C., Kanter, J.H., Martinez-Camblor, P. et al. The Effect of Antiseizure Medication Administration on Mortality and Early Posttraumatic Seizures in Critically Ill Older Adults with Traumatic Brain Injury. Neurocrit Care 37, 538–546 (2022). https://doi.org/10.1007/s12028-022-01531-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-022-01531-1