Abstract
Background
Elevated intracranial pressure due to cerebral edema is associated with very poor survival in patients with acute liver failure (ALF). Placing an intracranial pressure monitor (ICPm) aids in management of intracranial hypertension, but is associated with potentially fatal hemorrhagic complications related to the severe coagulopathy associated with ALF.
Methods
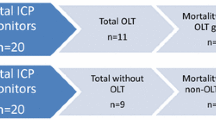
An institutional Acute Liver Failure Clinical Protocol (ALF-CP) was created to correct ALF coagulopathy prior to placing parenchymal ICP monitoring bolts. We aimed to investigate the frequency, severity, and clinical significance of hemorrhagic complications associated with ICPm bolt placement in the setting of an ALF-CP. All assessed patients were managed with the ALF-CP and had rigorous radiologic follow-up allowing assessment of the occurrence and chronology of hemorrhagic complications. We also aimed to compare our outcomes to other studies that were identified through a comprehensive review of the literature.
Results
Fourteen ALF patients were included in our analysis. There was no symptomatic hemorrhage after ICP monitor placement though four patients were found to have minor intraparenchymal asymptomatic hemorrhages after liver transplant when the ICP monitor had been removed, making the rate of radiographically identified clinically asymptomatic hemorrhage 28.6%. These results compare favorably to those found in a comprehensive review of the literature which revealed rates as high as 17.5% for symptomatic hemorrhages and 30.4% for asymptomatic hemorrhage.
Conclusion
This study suggests that an intraparenchymal ICPm can be placed safely in tertiary referral centers which utilize a protocol such as the ALF-CP that aggressively corrects coagulopathy. The ALF-CP led to advantageous outcomes for ICPm placement with a 0% rate of symptomatic and low rate of asymptomatic hemorrhagic complications, which compares well to results reported in other series. A strict ICPm placement protocol in this setting facilitates management of ALF patients with cerebral edema during the wait time to transplantation or spontaneous recovery.


Similar content being viewed by others
References
The American Association for the Study of Liver Diseases Position Paper: The management of Acute Liver Failure: Update 2011. 2011. https://www.aasld.org/sites/default/files/guideline_documents/alfenhanced.pdf. Accessed 24 Apr 2017.
Bernal W, Hall C, Karvellas CJ, Auzinger G, Sizer E, Wendon J. Arterial ammonia and clinical risk factors for encephalopathy and intracranial hypertension in acute liver failure. Hepatology. 2007;46:1844–52.
Meerman L, Zijlstra JG, Schweizer JJ, Verwer R, Slooff MJ, Haagsma EB. Acute liver failure: spontaneous recovery or transplantation? Scand J Gastroenterol Suppl. 1997;223:55–9.
Reddy KR, Ellerbe C, Schilsky M, et al. Determinants of outcome among patients with acute liver failure listed for liver transplantation in the United States. Liver Transplant. 2016;22:505–15.
Kodali S, McGuire BM. Diagnosis and management of hepatic encephalopathy in fulminant hepatic failure. Clin Liver Dis. 2015;19:565–76.
Bass NM. Monitoring and treatment of intracranial hypertension. Liver Transplant. 2000;6:S21–6.
Donovan JP, Shaw BW, Langnas AN, Sorrell MF. Brain water and acute liver failure: the emerging role of intracranial pressure monitoring. Hepatology. 1992;16:267–8.
Rabinstein AA. Treatment of brain edema in acute liver failure. Curr Treat Options Neurol. 2010;12:129–41.
Fortea JI, Bañares R, Vaquero J. Intracranial pressure in acute liver failure: to bolt or not to bolt—that is the question. Crit Care Med. 2014;42:1304–5.
Blei AT, Olafsson S, Webster S, Levy R. Complications of intracranial pressure monitoring in fulminant hepatic failure. The Lancet. 1993;341:157–8.
Shami VM, Caldwell SH, Hespenheide EE, Arseneau KO, Bickston SJ, Macik BG. Recombinant activated factor VII for coagulopathy in fulminant hepatic failure compared with conventional therapy. Liver Transplant. 2003;9:138–43.
Ferenci P, Lockwood A, Mullen K, Tarter R, Weissenborn K, Blei AT. Hepatic encephalopathy—definition, nomenclature, diagnosis, and quantification: final report of the working party at the 11th World Congresses of Gastroenterology, Vienna, 1998. Hepatology. 2002;35:716–21.
Ascher NL, Lake JR, Emond JC, Roberts JP. Liver transplantation at the University of California, San Francisco. Clin Transplant. 1993:175–7.
Poca MA, Sahuquillo J, Topczewski T, Penarrubia MJ, Muns A. Is intracranial pressure monitoring in the epidural space reliable? Fact Fict J Neurosurg. 2007;106:548–56.
Rajajee V, Fontana RJ, Courey AJ, Patil PG. Protocol based invasive intracranial pressure monitoring in acute liver failure: feasibility, safety and impact on management. Crit Care. 2017;21:178.
Lidofsky SD, Bass NM, Prager MC, et al. Intracranial pressure monitoring and liver transplantation for fulminant hepatic failure. Hepatology. 1992;16:1–7.
Rabadan AT, Spaho N, Hernandez D, Gadano A, de Santibanes E. Intraparenchymal intracranial pressure monitoring in patients with acute liver failure. Arq Neuropsiquiatr. 2008;66:374–7.
Le TV, Rumbak MJ, Liu SS, Alsina AE, van Loveren H, Agazzi S. Insertion of intracranial pressure monitors in fulminant hepatic failure patients: early experience using recombinant factor VII. Neurosurgery. 2010;66:455–8.
Maloney PR, Mallory GW, Atkinson JL, Wijdicks EF, Rabinstein AA, Van Gompel JJ. Intracranial pressure monitoring in acute liver failure: institutional case series. Neurocrit Care. 2016;25:86–93.
Raschke RA, Curry SC, Rempe S, et al. Results of a protocol for the management of patients with fulminant liver failure. Crit Care Med. 2008;36:2244–8.
Daas M, Plevak DJ, Wijdicks EF, et al. Acute liver failure: results of a 5-year clinical protocol. Liver Transplant. 1995;1:210–9.
Vaquero J, Fontana RJ, Larson AM, et al. Complications and use of intracranial pressure monitoring in patients with acute liver failure and severe encephalopathy. Liver Transplant. 2005;11:1581–9.
Karvellas CJ, Fix OK, Battenhouse H, Durkalski V, Sanders C, Lee WM. Outcomes and complications of intracranial pressure monitoring in acute liver failure: a retrospective cohort study. Crit Care Med. 2014;42:1157.
Keays RT, Alexander GJ, Williams R. The safety and value of extradural intracranial pressure monitors in fulminant hepatic failure. J Hepatol. 1993;18:205–9.
Feng Z-Y, Xu X, Zhu S-M, Bein B, Zheng S-S. Effects of low central venous pressure during preanhepatic phase on blood loss and liver and renal function in liver transplantation. World J Surg. 2010;34:1864–73.
Polson J, Lee WM. AASLD position paper: the management of acute liver failure. Hepatology. 2005;41:1179–97.
Kamat P, Kunde S, Vos M, et al. Invasive intracranial pressure monitoring is a useful adjunct in the management of severe hepatic encephalopathy associated with pediatric acute liver failure. Pediatr Crit Care Med. 2012;13:e33.
Stravitz RT, Kramer AH, Davern T, et al. Intensive care of patients with acute liver failure: recommendations of the US Acute Liver Failure Study Group. Crit Care Med. 2007;35:2498–508.
Acknowledgements
We confirm that this manuscript complies with all instructions to authors. Authorship requirements have been met, and the final manuscript was approved by all authors. This manuscript has not been published elsewhere and is not under consideration by another journal. We have adhered to ethical guidelines and have IRB approval with waiver of consent. This study does not require completion of a checklist. There are no funding sources that directly conflict with the completion of this manuscript.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
All authors have made a substantial contribution to the information and material submitted for publication and all have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Informed Consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jinadasa, S.P., Ruan, Q.Z., Bayoumi, A.B. et al. Hemorrhagic Complications of Invasive Intracranial Pressure Monitor Placement in Acute Liver Failure: Outcomes of a Single-Center Protocol and Comprehensive Literature Review. Neurocrit Care 35, 87–102 (2021). https://doi.org/10.1007/s12028-020-01143-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-020-01143-7