Abstract
Background
Although small series have suggested that younger age is associated with less favorable outcome after severe traumatic brain injury (TBI), confounders and biases have limited our understanding of this relationship. We hypothesized that there would be an association between age and mortality in children within an ongoing observational, cohort study.
Methods
The first 200 subjects from the Approaches and Decisions for Acute Pediatric TBI trial were eligible for this analysis (inclusion criteria: severe TBI (Glasgow Coma Scale [GCS] score ≤ 8], age 18 years, and intracranial pressure (ICP) monitor placed; exclusion: pregnancy). Children with suspected abusive head trauma (AHT) were excluded to avoid bias related to the association between AHT and mortality. Demographics, and prehospital and resuscitation events were collected/analyzed, and children were stratified based on age at time of injury (< 5, 5–< 11, 11–18 years) and presented as mean ± standard error of the mean (SEM). Analyses of variance were used to test the equality of the means across the group for continuous variable, and Chi-square tests were used to compare percentages for discrete variables (post hoc comparisons were made using t test and Bonferroni corrections, as needed). Kaplan–Meier curves were generated for each age subgroup describing the time of death, and log-rank was used to compare the curves. Cox proportional hazards regression models were used to assess the effect of age on time to death while controlling for covariates.
Results
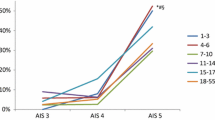
In the final cohort (n = 155, 45 excluded for AHT), overall age was 9.2 years ± 0.4 and GCS was 5.3 ± 0.1. Mortality was similar between strata (14.0, 20.0, 20.9%, respectively, p = 0.58). Motor vehicle accidents were the most common mechanism across all strata, while falls tended to be more common in the youngest stratum (p = 0.08). The youngest stratum demonstrated increased incidence of spontaneous hypothermia at presentation and decreased hemoglobin concentrations and coagulopathies, while the oldest demonstrated lower platelet counts.
Conclusions
In contrast to previous reports, we failed to detect mortality differences across age strata in children with severe TBI. We have discerned novel associations between age and various markers of injury—unrelated to AHT—that may lead to testable hypotheses in the future.
Similar content being viewed by others
References
CDC. Traumatic Brain Injury in the United States, emergency department visits, hospitalizations, and deaths. [cited January 7, 2016] http://www.cdc.gov/traumaticbraininjury/pdf/blue_book.pdf.
CDC. Traumatic brain injury in the United States: Fact Sheet.
Stanley RM, Bonsu BK, Zhao W, et al. US estimates of hospitalized children with severe traumatic brain injury: implications for clinical trials. Pediatrics. 2012;129(1):e24–30.
Carney NA, Chesnut R, Kochanek PM. Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents. Pediatr Crit Care Med. 2003;4(3 Suppl):S1.
Kochanek PM, Carney N, Adelson PD, et al. Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents–second edition. Pediatr Crit Care Med. 2012;13(Suppl 1):S1–82.
Dean NP, Boslaugh S, Adelson PD, et al. Physician agreement with evidence-based recommendations for the treatment of severe traumatic brain injury in children. J Neurosurg. 2007;107(5 Suppl):387–91.
Tosetti P, Hicks RR, Theriault E, et al. Toward an international initiative for traumatic brain injury research. J Neurotrauma. 2013;30(14):1211–22.
Taylor HG, Alden J. Age-related differences in outcomes following childhood brain insults: an introduction and overview. J Int Neuropsychol Soc. 1997;3(6):555–67.
Anderson V, Catroppa C, Morse S, et al. Functional plasticity or vulnerability after early brain injury? Pediatrics. 2005;116(6):1374–82.
Ducrocq SC, Meyer PG, Orliaguet GA, et al. Epidemiology and early predictive factors of mortality and outcome in children with traumatic severe brain injury: experience of a French pediatric trauma center. Pediatr Crit Care Med. 2006;7:461–7.
Tude Melo JR, DiRocco F, Blanot S, et al. Mortality in children with severe head trauma: predictive factors and proposal for a new predictive scale. Neurosurgery. 2010;67:1542–7.
Levin HS, Aldrich EF, Saydjari C, et al. Severe head injury in children: experience of the Traumatic Coma Data Bank. Neurosurgery. 1992;31(3):435–43 (discussion 443–434).
Berger MS, Pitts LH, Lovely M, et al. Outcome from severe head injury in children and adolescents. J Neurosurg. 1985;62(2):194–9.
Crowe LM, Catroppa C, Babl FE, et al. Timing of traumatic brain injury in childhood and intellectual outcome. J Pediatr Psychol. 2012;37(7):745–54.
Keenan HT, Runyan DK, Marshall SW, et al. A population-based comparison of clinical and outcome characteristics of young children with serious inflicted and noninflicted traumatic brain injury. Pediatrics. 2004;114(3):633–9.
Prasad MR, Ewing-Cobbs L, Swank PR, et al. Predictors of outcome following traumatic brain injury in young children. Pediatr Neurosurg. 2002;36(2):64–74.
Ewing-Cobbs L, Kramer L, Prasad M, et al. Neuroimaging, physical, and developmental findings after inflicted and noninflicted traumatic brain injury in young children. Pediatrics. 1998;102(2 Pt 1):300–7.
Hymel KP, Makoroff KL, Laskey AL, et al. Mechanisms, clinical presentations, injuries, and outcomes from inflicted versus noninflicted head trauma during infancy: results of a prospective, multicentered, comparative study. Pediatrics. 2007;119(5):922–9.
Michaud LJ, Rivara FP, Grady MS, et al. Predictors of survival and severity of disability after severe brain injury in children. Neurosurgery. 1992;31(2):254–64.
Goldman PS, Galkin TW. Prenatal removal of frontal association cortex in the fetal rhesus monkey: anatomical and functional consequences in postnatal life. Brain Res. 1978;152(3):451–85.
Kennard MA. Age and other factors in motor recovery from precentral lesions in monkeys. Am J Physiol. 1936;115(1):138–46.
Kolb B, Gibb R. Possible anatomical basis of recovery of function after neonatal frontal lesions in rats. Behav Neurosci. 1993;107(5):799–811.
Villablanca JR, Carlson-Kuhta P, Schmanke TD, et al. A critical maturational period of reduced brain vulnerability to developmental injury. I. Behavioral studies in cats. Brain Res Dev Brain Res. 1998;105(2):309–24.
Anderson V, Spencer-Smith M, Wood A. Do children really recover better? Neurobehavioural plasticity after early brain insult. Brain. 2011;134(Pt 8):2197–221.
Bittigau P, Sifringer M, Pohl D, et al. Apoptotic neurodegeneration following trauma is markedly enhanced in the immature brain. Ann Neurol. 1999;45(6):724–35.
Giza CC, Prins ML. Is being plastic fantastic? Mechanisms of altered plasticity after developmental traumatic brain injury. Dev Neurosci. 2006;28(4–5):364–79.
Kolb B, Cioe J, Whishaw IQ. Is there an optimal age for recovery from motor cortex lesions? I. Behavioral and anatomical sequelae of bilateral motor cortex lesions in rats on postnatal days 1, 10, and in adulthood. Brain Res. 2000;882(1–2):62–74.
Kolb B, Gibb R, van der Kooy D. Neonatal frontal cortical lesions in rats alter cortical structure and connectivity. Brain Res. 1994;645(1–2):85–97.
Sifringer M, Stefovska V, Zentner I, et al. The role of matrix metalloproteinases in infant traumatic brain injury. Neurobiol Dis. 2007;25(3):526–35.
Morrison WE, Arbelaez JJ, Fackler JC, et al. Gender and age effects on outcome after pediatric traumatic brain injury. Pediatr Crit Care Med. 2004;5(2):145–51.
Ewing-Cobbs L, Prasad M, Kramer L, et al. Acute neuroradiologic findings in young children with inflicted or noninflicted traumatic brain injury. Childs Nerv Syst. 2000;16(1):25–33 (discussion 34).
Davies FC, Coats TJ, Fisher R, et al. A profile of suspected child abuse as a subgroup of major trauma patients. Emerg Med J. 2015;32(12):921–5.
Adelson PD, Wisniewski SR, Beca J, et al. Comparison of hypothermia and normothermia after severe traumatic brain injury in children (Cool Kids): a phase 3, randomised controlled trial. Lancet Neurol. 2013;12(6):546–53.
Hutchison JS, Ward RE, Lacroix J, et al. Hypothermia therapy after traumatic brain injury in children. New Engl J Med. 2008;358(23):2447–56.
Adelson PD, Ragheb J, Kanev P, et al. Phase II clinical trial of moderate hypothermia after severe traumatic brain injury in children. Neurosurgery. 2005;56(4):740–54 (discussion 740–754).
Moran LM, Babikian T, Del Piero L, et al. The UCLA study of predictors of cognitive functioning following moderate/severe pediatric traumatic brain injury. J Int Neuropsychol Soc. 2016;22(5):512–9.
Treble-Barna A, Zang H, Zhang N, et al. Observed parent behaviors as time-varying moderators of problem behaviors following traumatic brain injury in young children. Dev Psychol. 2016;52(11):1777–92.
Acknowledgments
Research reported in this publication was supported by the National Institute of Neurological Disorders and Stroke of the National Institutes of Health under Award Number U01 NS081041. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Investigators for the ADAPT trial are Shruti Agrawal, Addenbrookes Hospital, Cambridge, UK; Sarah Mahoney, Alder Hey Children’s NHS Foundation Trust, Liverpool, UK; Deepak Gupta, All India Institute of Medical Sciences, New Delhi, India; John Beca, Auckland DHB Charitable Trust, Starship Children’s Hospital, Auckland, NZ; Laura Loftis, Baylor College of Medicine, Houston, TX; Kevin Morris, Birmingham Children’s Hospital NHS Foundation Trust, Birmingham, UK; Lauren Piper, Levine Children’s Hospital, Charlotte, NC; Anthony Slater, Children’s Health Queensland Hospital and Health Service, Brisbane, Australia; Karen Walson, Children’s Healthcare of Atlanta, Atlanta, GA; Tellen Bennett, Children’s Hospital Colorado, Aurora, CO; Todd Kilbaugh, Children’s Hospital of Philadelphia, Philadelphia, PA; AM Iqbal O’Meara, Children’s Hospital of Richmond, Richmond, VA; Nathan Dean, Children’s National Medical Center, Washington, DC; Ranjit S. Chima, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH; Katherine Biagas, Columbia University, New York, NY; Enno Wildschut, Erasmus Medical Center, Rotterdam, Netherlands; Mark Peters, Great Ormond St Hospital NHS Foundation Trust, London, UK; Kerri LaRovere, Boston Children’s Hospital, Boston, MA; Joan Balcells, Hospital Vall d’Hebron, Barcelona, Spain; Courtney Robertson, John Hopkins University, Baltimore, MD; Shira Gertz, Joseph M. Sanzari Children’s Hospital at Hackensack University Medical Center, Hackensack, NJ; Akash Deep, King’s College Hospital NHS Foundation Trust, London, UK; Sian Cooper, Leeds Teaching Hospitals NHS Trust, Leeds, UK; Mark Wainwright, Lurie Children’s Hospital, Chicago IL; Sarah Murphy, Massachusetts General Hospital, Boston, MA; John Kuluz, Miami Children’s Hospital, Miami, FL; Warwick Butt, Murdoch Children’s Research Institute, Royal Children’s Hospital, Melbourne, Australia; Nicole O’Brien, Nationwide Children’s Hospital, Columbus, OH; Neal Thomas, Pennsylvania State University, Hershey, PA; Sandra Buttram, Phoenix Children’s Hospital, Phoenix, AZ; Simon Erickson, Princess Margaret Hospital, Perth, Australia; J. Mahil Samuel, Royal Manchester Children’s Hospital NHS Foundation Trust, Manchester, UK; Rachel Agbeko, The Newcastle Upon Tyne Hospitals NHS Foundation Trust, Newcastle, UK; Richard Edwards, University Hospital Bristol NHS Foundation Trust, Bristol, UK; Kesava Ananth Ramakrishnan, University Hospital Southampton NHS Foundation Trust, Southampton, UK; Margaret Winkler and Santiago Borasino, University of Alabama at Birmingham, Birmingham, AL; Joanne Natale, University of California, Davis, Sacramento, CA; Christopher Giza, University of California, Los Angeles, Los Angeles, CA; Mary Hilfiker and David Shellington, University of California, San Diego, San Diego, CA; Anthony Figaji, Red Cross War Memorial Children’s Hospital, Cape Town, South Africa; Elizabeth Newell, University of Iowa Children’s Hospital, Iowa City, IA; Edward Truemper, University of Nebraska Medical Center and Nebraska Medical Center, Omaha, NE; Robert Clark, University of Pittsburgh, Pittsburgh, PA; Kit Newth, Children’s Hospital of Los Angeles, Los Angeles, CA; Nadeem Shafi, LeBonheur Children’s Hospital, Memphis, TN; Darryl Miles, University of Texas Southwestern Medical Center, Dallas, TX; Michelle Schober, University of Utah, Jerry Zimmerman, University of Washington, Seattle, WA; Peter Ferrazzano, University of Wisconsin, Madison, WI; Jose Pineda, Washington University–St. Louis, St. Louis, MO; and Ajit Sarnaik, Wayne State University, Detroit, MI.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sarnaik, A., Ferguson, N.M., O’Meara, A.I. et al. Age and Mortality in Pediatric Severe Traumatic Brain Injury: Results from an International Study. Neurocrit Care 28, 302–313 (2018). https://doi.org/10.1007/s12028-017-0480-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-017-0480-x