Abstract
Background
In order to deliver specialized neurocritical care (NCC) without a dedicated neurological intensive care unit (ICU), we established a virtual NCC unit within an existing mixed level III ICU. This initiative required changes to patient allocation, physician staffing, and care protocols. In advance of its implementation, we gaged readiness, assessed barriers, and solicited feedback from staff.
Methods
Clinicians at our academic hospital and trauma centre in Toronto, Ontario were the subjects of this concurrent mixed methods study. Eighteen stakeholders were individually interviewed. 116 of 217 eligible ICU staff participated in the survey and 36 staff attended the focus group sessions.
Results
From the survey, the most significant barriers to this reorganization were staff anxiety about coping (28 %) and a concern that patients would not receive better care (24 %). Noteworthy obstacles about the use of protocols were their lack of flexibility (19 %) and that implementation was seen as impractical (16 %). Seventeen barriers were proposed through an open-ended survey question. Content analysis revealed general resistance, educational challenges, workflow adjustment to a diagnosis-based rounding pattern and coordination conflicts to be the central barriers. These findings were confirmed in focus group discussions, with a lack of resources as an additional important challenge.
Conclusions
A new workable model for NCC has been developed, facilitated by this analysis. Steps to overcome barriers demonstrated in this study include additional educational measures, changes to the rounding protocols, and patient allocation algorithms.





Similar content being viewed by others
References
Thenayan EA, Bolton C, Jichici D, Savard M, Teitelbaum J, Young B, et al. Neurocritical care in Canada: evolving streams in a new discipline. Can J Neurol Sci. 2008;35(4):405–8.
Patel HC, Menon DK, Tebbs S, Hawker R, Hutchinson PJ, Kirkpatrick PJ. Specialist neurocritical care and outcome from head injury. Intensive Care Med. 2002;28(5):547–53.
Smith MI. Neurocritical care: has it come of age? Br J Anaesth. 2004;93(6):753–5.
Varelas PN, Eastwood D, Yun HJ, Spanaki MV, Hacein Bey L, Kessaris C, et al. Impact of a neurointensivist on outcomes in patients with head trauma treated in a neurosciences intensive care unit. J Neurosurg. 2006;104(5):713–9.
Josephson SA, Douglas VC, Lawton MT, English JD, Smith WS, Ko NU. Improvement in intensive care unit outcomes in patients with subarachnoid hemorrhage after initiation of neurointensivist co-management. J Neurosurg. 2010;112(3):626–30.
Knopf L, Staff I, Gomes J, McCullough L. Impact of a neurointensivist on outcomes in critically ill stroke patients. Neurocrit Care. 2012;16(1):63–71.
Diringer MN, Edwards DF. Admission to a neurologic/neurosurgical intensive care unit is associated with reduced mortality rate after intracerebral hemorrhage. Crit Care Med. 2001;29(3):635–40.
Varelas PN, Schultz L, Conti M, Spanaki M, Genarrelli T, Hacein-Bey L. The impact of a neuro-intensivist on patients with stroke admitted to a neurosciences intensive care unit. Neurocrit Care. 2008;9(3):293–9.
Helmy A, Vizcaychipi M, Gupta AK. Traumatic brain injury: intensive care management. Br J Anaesth. 2007;99(1):32–42.
Brain Trauma Foundation, American Association of Neurological Surgeons, Congress of Neurological Surgeons. Guidelines for the management of severe traumatic brain injury. J Neurotrauma. 2007;24(Suppl 1):S1–106.
Morgenstern LB, Hemphill JC, Anderson C, Becker K, Broderick JP, Connolly ES Jr, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2010;41(9):2108–29.
Brophy GM, Bell R, Claassen J, Alldredge B, Bleck TP, Glauser T, et al. Guidelines for the evaluation and management of status epilepticus. Neurocrit Care. 2012;17(1):3–23.
Maas AI, Menon DK, Lingsma HF, Pineda JA, Sandel ME, Manley GT. Re-orientation of clinical research in traumatic brain injury: report of an international workshop on comparative effectiveness research. J Neurotrauma. 2012;29(1):32–46.
Reade MC, Angus DC. The clinical research enterprise in critical care: what’s right, what’s wrong, and what’s ahead? Crit Care Med. 2009;37(1 Suppl):S1–9.
Fakhry SM, Trask AL, Waller MA, Watts DD, IRTC Neurotrauma Task Force. Management of brain-injured patients by an evidence-based medicine protocol improves outcomes and decreases hospital charges. J Trauma. 2004;56(3):492–9 discussion 499–500.
Durbin CG Jr. Team model: advocating for the optimal method of care delivery in the intensive care unit. Crit Care Med. 2006;34(3 Suppl):S12–7.
Kurtz P, Fitts V, Sumer Z, Jalon H, Cooke J, Kvetan V, et al. How does care differ for neurological patients admitted to a neurocritical care unit versus a general ICU? Neurocrit Care. 2011;15(3):477–80.
Mirski MA, Chang CW, Cowan R. Impact of a neuroscience intensive care unit on neurosurgical patient outcomes and cost of care: evidence-based support for an intensivist-directed specialty ICU model of care. J Neurosurg Anesthesiol. 2001;13(2):83–92.
Teig M, Smith M. Where should patients with severe traumatic brain injury be managed? All patient should be managed in a neurocritical care unit. J Neurosurg Anesthesiol. 2010;22(4):357–9.
Kramer AH, Zygun DA. Do neurocritical care units save lives? Measuring the impact of specialized ICUs. Neurocrit Care. 2011;14(3):329–33.
Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211.
Fitzpatrick R, Boulton M. Qualitative methods for assessing health care. Qual Health Care. 1994;3(2):107–13.
Gallagher M, Hares T, Spencer J, Bradshaw C, Webb I. The nominal group technique: a research tool for general practice? Fam Pract. 1993;10(1):76–81.
Rubenfeld GD, Cooper C, Carter G, Thompson BT, Hudson LD. Barriers to providing lung-protective ventilation to patients with acute lung injury. Crit Care Med. 2004;32(6):1289–93.
Sinuff T, Cook D, Giacomini M, Heyland D, Dodek P. Facilitating clinician adherence to guidelines in the intensive care unit: a multicenter, qualitative study. Crit Care Med. 2007;35(9):2083–9.
Cochrane LJ, Olson CA, Murray S, Dupuis M, Tooman T, Hayes S. Gaps between knowing and doing: understanding and assessing the barriers to optimal health care. J Contin Educ Health Prof. 2007;27(2):94–102.
Nguyen YL, Wunsch H, Angus DC. Critical care: the impact of organization and management on outcomes. Curr Opin Crit Care. 2010;16(5):487–92.
Curtis JR, Cook DJ, Wall RJ, Angus DC, Bion J, Kacmarek R, et al. Intensive care unit quality improvement: a “how-to” guide for the interdisciplinary team. Crit Care Med. 2006;34(1):211–8.
Acknowledgments
Funding for this Project was provided through the Innovation Fund from Ontario’s Academic Health Science Centres’ Alternate Funding Plan (AHSC AFP). A.K.S. is supported by the Ontario Neurotrauma Foundation. Thanks to Eman Leung, Ph. D. who is the Manager of the Knowledge Translation Program at the Li Ka Shing Knowledge Institute at St. Michael’s Hospital for his advice on study design. The authors thank registered nurses Lars Kure, Katie Weaver, Andrea Fernandes, and Grace Walter for their efforts throughout the implementation process.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
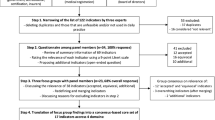
See Fig. 6.
Rights and permissions
About this article
Cite this article
Botting, M.J., Phan, N., Rubenfeld, G.D. et al. Using Barriers Analysis to Refine a Novel Model of Neurocritical Care. Neurocrit Care 20, 5–14 (2014). https://doi.org/10.1007/s12028-013-9905-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-013-9905-3