Abstract
Purpose
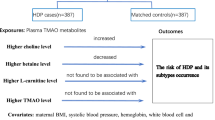
To investigate the associations of choline, betaine, dimethylglycine (DMG), L-carnitine, and Trimethylamine-N-oxide (TMAO) with the risk of Gestational diabetes mellitus (GDM) as well as the markers of glucose homeostasis.
Methods
We performed a case-control study including 200 diagnosed GDM cases and 200 controls matched by maternal age (±2 years) and gestational age (±2 weeks). Concentrations of serum metabolites were measured by the high-performance liquid chromatography - tandem mass spectrometry (HPLC-MS/MS).
Results
Compared to the control group, GDM group had significantly lower serum betaine concentration and betaine/choline ratio, and higher DMG concentration. Furthermore, decreased betaine concentration and betaine/choline ratio, increased DMG concentration showed significant association with the risk of GDM. In addition, serum betaine concentrations were negatively associated with blood glucose levels at 1-h post-glucose load (OGTT-1h), and both betaine and L-carnitine concentrations were positively associated with 1,5-anhydroglucitol levels. Betaine/choline ratio was negatively associated with OGTT-1h and blood glucose levels at 2-h post-glucose load (OGTT-2h) and serum choline concentrations were negatively associated with fasting blood glucose and positively associated with OGTT-2h.
Conclusion
Decreased serum betaine concentrations and betaine/choline ratio, and elevated DMG concentrations could be significant risk factors for GDM. Furthermore, betaine may be associated with blood glucose regulation and short-term glycemic fluctuations.

Similar content being viewed by others
References
P. Chen, S. Wang, J. Ji et al. Risk factors and management of gestational diabetes. Cell Biochem. Biophys. 71(2), 689–694 (2015)
E.C. Johns, F.C. Denison, J.E. Norman et al. Gestational diabetes mellitus: mechanisms, treatment, and complications. Trends Endocrinol. Metab. 29(11), 743–754 (2018)
B. Wicklow, R. Retnakaran, Gestational diabetes mellitus and its implications across the life span. Diabetes Metab J 47(3), 333–344 (2023).
W. Ye, C. Luo, J. Huang et al. Gestational diabetes mellitus and adverse pregnancy outcomes: systematic review and meta-analysis. BMJ 377, e67946 (2022)
M.S. Paulo, N.M. Abdo, R. Bettencourt-Silva et al. Gestational diabetes mellitus in Europe: a systematic review and meta-analysis of prevalence studies. Front. Endocrinol. 12, 691033 (2021)
A. Sweeting, J. Wong, H.R. Murphy et al. A clinical update on gestational diabetes mellitus. Endocr. Rev. 43(5), 763–793 (2022)
J. Leng, P. Shao, C. Zhang et al. Prevalence of gestational diabetes mellitus and its risk factors in Chinese pregnant women: a prospective population-based study in Tianjin, china. Plos One 10(3), e121029 (2015)
H.D. Mcintyre, P. Catalano, C. Zhang et al. Gestational diabetes mellitus. Nat. Rev. Dis. Primers 5(1), 47 (2019)
J. Wan, J. Ma, Efficacy of dietary supplements targeting gut microbiota in the prevention and treatment of gestational diabetes mellitus. Front. Microbiol. 13, 927883 (2022)
M. Lever, S. Slow, The clinical significance of betaine, an osmolyte with a key role in methyl group metabolism. Clin. Biochem. 43(9), 732–744 (2010)
D. Fennema, I.R. Phillips, E.A. Shephard, Trimethylamine and trimethylamine n-oxide, a flavin-containing monooxygenase 3 (fmo3)-mediated host-microbiome metabolic axis implicated in health and disease. Drug Metab. Dispos. 44(11), 1839–1850 (2016)
P. Gatarek, J. Kaluzna-Czaplinska, Trimethylamine n-oxide (tmao) in human health. Excli. J. 20, 301–319 (2021)
Y. Heianza, D. Sun, X. Li et al. Gut microbiota metabolites, amino acid metabolites and improvements in insulin sensitivity and glucose metabolism: the pounds lost trial. Gut 68(2), 263–270 (2019)
N. Friedrich, T. Skaaby, M. Pietzner et al. Identification of urine metabolites associated with 5-year changes in biomarkers of glucose homoeostasis. Diabetes Metab. 44(3), 261–268 (2018)
S. Qi, L. Liu, S. He et al. Trimethylamine n-oxide and related metabolites in the serum and risk of type 2 diabetes in the Chinese population: a case-control study. Diabetes Metab. Syndr. Obes. 16, 547–555 (2023)
K. Szkudelska, T. Szkudelski, The anti-diabetic potential of betaine. Mechanisms of action in rodent models of type 2 diabetes. Biomed. Pharmacother. 150, 112946 (2022)
J. Du, L. Shen, Z. Tan et al. Betaine supplementation enhances lipid metabolism and improves insulin resistance in mice fed a high-fat diet. Nutrients 10(2), 131 (2018)
X. Gao, X. Liu, J. Xu et al. Dietary trimethylamine n-oxide exacerbates impaired glucose tolerance in mice fed a high fat diet. J. Biosci. Bioeng. 118(4), 476–481 (2014)
X. Huo, J. Li, Y. Cao et al. Trimethylamine n-oxide metabolites in early pregnancy and risk of gestational diabetes: a nested case-control study. J. Clin. Endocrinol. Metab. 104(11), 5529–5539 (2019)
E. Barzilay, A. Moon, L. Plumptre et al. Fetal one-carbon nutrient concentrations may be affected by gestational diabetes. Nutr. Res. 55, 57–64 (2018)
I.B. Hirsch, Glycemic variability and diabetes complications: does it matter? Of course it does! Diabetes Care 38(8), 1610–1614 (2015)
M.J. Kim, H.S. Jung, Y. Hwang-Bo et al. Evaluation of 1, 5-anhydroglucitol as a marker for glycemic variability in patients with type 2 diabetes mellitus. Acta Diabetol. 50, 505–510 (2013)
D.A. American, Standards of medical care in diabetes—2014. Diabetes Care 37(Supplement_1), S14–S80 (2014)
C. Steuer, P. Schütz, L. Bernasconi et al. Simultaneous determination of phosphatidylcholine-derived quaternary ammonium compounds by a lc–ms/ms method in human blood plasma, serum and urine samples. J. Chromatogr. B 1008, 206–211 (2016)
M.F. Mujica-Coopman, A. Tan, T.H. Schroder et al. Serum betaine and dimethylglycine are higher in South Asian compared with European pregnant women in Canada, with betaine and total homocysteine inversely associated in early and midpregnancy, independent of ethnicity. J. Nutr. 149(12), 2145–2155 (2019)
U. Keller, C. van der Wal, G. Seliger et al. Carnitine status of pregnant women: effect of carnitine supplementation and correlation between iron status and plasma carnitine concentration. Eur. J. Clin. Nutr. 63(9), 1098–1105 (2009)
I.Y. Ozarda, G. Uncu, I.H. Ulus, Free and phospholipid-bound choline concentrations in serum during pregnancy, after delivery and in newborns. Arch. Physiol. Biochem. 110(5), 393–399 (2002)
X. Gong, Y. Du, X. Li et al. Maternal plasma betaine in middle pregnancy was associated with decreased risk of gdm in twin pregnancy: a cohort study. Diabetes Metab. Syndr. Obes. 14, 2495–2504 (2021)
E. Kathirvel, K. Morgan, G. Nandgiri et al. Betaine improves nonalcoholic fatty liver and associated hepatic insulin resistance: a potential mechanism for hepatoprotection by betaine. Am. J. Physiol. Gastr. L. 299(5), G1068–G1077 (2010)
L. Xu, D. Huang, Q. Hu et al. Betaine alleviates hepatic lipid accumulation via enhancing hepatic lipid export and fatty acid oxidation in rats fed with a high-fat diet. Brit. J. Nutr. 113(12), 1835–1843 (2015)
A. Ejaz, L. Martinez-Guino, A.B. Goldfine et al. Dietary betaine supplementation increases fgf21 levels to improve glucose homeostasis and reduce hepatic lipid accumulation in mice. Diabetes 65(4), 902–912 (2016)
L. Zhang, Y. Qi, Z. Aluo et al. Betaine increases mitochondrial content and improves hepatic lipid metabolism. Food Funct. 10(1), 216–223 (2019)
S.H. Zeisel, C.K. Da, Choline: an essential nutrient for public health. Nutr. Rev. 67(11), 615–623 (2009)
P.J. Raubenheimer, M.J. Nyirenda, B.R. Walker, A choline-deficient diet exacerbates fatty liver but attenuates insulin resistance and glucose intolerance in mice fed a high-fat diet. Diabetes 55(7), 2015–2020 (2006)
X. Li, Y. Chen, J. Liu et al. Serum metabolic variables associated with impaired glucose tolerance induced by high-fat-high-cholesterol diet in macaca mulatta. Exp. Biol. Med. (Maywood) 237(11), 1310–1321 (2012)
G. Wu, L. Zhang, T. Li et al. Choline deficiency attenuates body weight gain and improves glucose tolerance in ob/ob mice. J. Obes. 2012, 319172 (2012)
Y.M. Chen, Y. Liu, R.F. Zhou et al. Associations of gut-flora-dependent metabolite trimethylamine-n-oxide, betaine and choline with non-alcoholic fatty liver disease in adults. Sci. Rep. 6, 19076 (2016)
R.L. Jacobs, Y. Zhao, D.P. Koonen et al. Impaired de novo choline synthesis explains why phosphatidylethanolamine n-methyltransferase-deficient mice are protected from diet-induced obesity. J. Biol. Chem. 285(29), 22403–22413 (2010)
A.A. Noga, D.E. Vance, A gender-specific role for phosphatidylethanolamine n-methyltransferase-derived phosphatidylcholine in the regulation of plasma high density and very low density lipoproteins in mice. J. Biol. Chem. 278(24), 21851–21859 (2003)
S. Wan, J.N. van der Veen, N.J. Bakala et al. Hepatic pemt activity mediates liver health, weight gain, and insulin resistance. Faseb J. 33(10), 10986–10995 (2019)
J. Vangipurapu, L. Fernandes Silva, T. Kuulasmaa et al. Microbiota-related metabolites and the risk of type 2 diabetes. Diabetes Care 43(6), 1319–1325 (2020)
J.D. Finkelstein, Methionine metabolism in mammals. J. Nutr. Biochem. 1(5), 228–237 (1990)
M.D. Niculescu, S.H. Zeisel, Diet, methyl donors and DNA methylation: interactions between dietary folate, methionine and choline. J. Nutr. 132(8 Suppl), 2333S–2335S (2002)
H.D. Mcintyre, S. Colagiuri, G. Roglic et al. Diagnosis of gdm: a suggested consensus. Best Pract. Res. Clin. Obstet. Gynaecol. 29(2), 194–205 (2015)
L. Sun, X. Tan, X. Liang et al. Maternal betaine supplementation mitigates maternal high fat diet-induced NAFLD in offspring mice through gut microbiota. Nutrients 15(2), 284 (2023)
C.L. Meek, D. Tundidor, D.S. Feig et al. Novel biochemical markers of glycemia to predict pregnancy outcomes in women with type 1 diabetes. Diabetes Care 44(3), 681–689 (2021)
S.J. Loomis, A. Köttgen, M. Li et al. Rare variants in slc5a10 are associated with serum 1, 5-anhydroglucitol (1, 5-ag) in the atherosclerosis risk in communities (aric) study. Sci. Rep.-Uk. 9(1), 5941 (2019)
M. Dworacka, H. Winiarska, M. Szymanska et al. 1,5-anhydro-d-glucitol: a novel marker of glucose excursions. International journal of clinical practice. Supplement 129, 40–44 (2002)
K.M. Dungan, 1, 5-anhydroglucitol (glycomark™) as a marker of short-term glycemic control and glycemic excursions. Expert Rev. Mol. Diagn. 8(1), 9–19 (2008)
T. Yamanouchi, N. Ogata, T. Tagaya et al. Clinical usefulness of serum 1, 5-anhydroglucitol in monitoring glycaemic control. Lancet 347(9014), 1514–1518 (1996)
P. Salahi, M. Alirezaei, A. Kheradmand et al. Betaine: a promising micronutrient in diet intervention for ameliorating maternal blood biochemical alterations in gestational diabetes mellitus. Int. J. Pept. Res. Ther. 26(2), 1177–1184 (2020)
A.A. Sangouni, F. Pakravanfar, A. Ghadiri-Anari et al. The effect of l-carnitine supplementation on insulin resistance, sex hormone-binding globulin and lipid profile in overweight/obese women with polycystic ovary syndrome: a randomized clinical trial. Eur. J. Nutr. 61(3), 1199–1207 (2022)
Acknowledgements
We are very grateful for the cooperation of the pregnant women who participated in these studies.
Funding
The research was supported by basic research project of Shenzhen Science and Technology Research Projects (JCYJ20220530162412029), Shenzhen Science and Technology Innovation Committee (KJYY20180703173402020), Shenzhen City and Longgang District Science and Technology Innovation Projects (LGKCYLWS2022008) and Guangdong Basic and Applied Basic Research Foundation (2023A1515030168).
Author information
Authors and Affiliations
Contributions
Z.Z. study design, data analysis and manuscript preparation; Y.Y. methodology; Y.S., X.W., S.H., and J.H. investigation; L.W. and F.W. review and editing. The final manuscript was reviewed and approved by all authors.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Consent to participate
Informed consent was obtained from all subjects involved in the study.
Ethics approval
The current study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving research study participants were approved by the Ethical Committee of Longgang District Maternity & Child Healthcare Hospital of Shenzhen City (Approval NO. LGFYYXLLL-2022-039).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhou, Z., Yao, Y., Sun, Y. et al. Serum betaine and dimethylglycine in mid-pregnancy and the risk of gestational diabetes mellitus: a case-control study. Endocrine (2024). https://doi.org/10.1007/s12020-024-03732-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12020-024-03732-4