Abstract
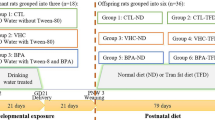
Di-2-ethylhexyl phthalate (DEHP), a ubiquitous endocrine disruptor and plasticizer of polyvinyl chloride, is being used in the manufacture of consumer and medical products as well as in children’s toys. Fetuses and newborns are more sensitive to endocrine disruption. DEHP is a lipophilic substance, which could easily be transferred to the developing offspring through placenta or breast milk. DEHP alters the metabolism of the endocrine organs, which leads to energy imbalance associated with increased risk of insulin resistance, obesity and cardiovascular disease. The heart is an insulin-responsive organ. The effect of DEHP on the cardiac muscle insulin signaling remains obscure. Since the developmental period is more vulnerable to the adverse effect of DEHP, the present study was framed to study the impact of lactational exposure of DEHP on insulin signaling molecules in the cardiac muscle of F1 progeny female albino rat (postnatal day 60). Healthy dams were treated with DEHP orally (0, 1, 10 and 100 mg/kg body weight/day, respectively) from the postpartum day 1–21. Both low and high doses are relevant to the human exposure, and hence, both were used in this study. At a low dose (1 mg/kg body weight/day), obvious differences were observed in the fasting blood glucose and the insulin signaling molecule when compared to control. But marked differences were observed in the cardiac tissue insulin signaling molecules of animals treated with high doses. In conclusion, the DEHP treatment significantly increased the fasting blood glucose level and decreased the insulin receptor (IR), insulin receptor substrate (IRS-1), p-IRS-1Tyr632, p-AktSer473, plasma membrane glucose transporter (GLUT4), 14C-2-deoxyglucose uptake and the 14C-glucose oxidation. Conversely, Akt and GLUT4 protein in cytosol remained unaltered compared to control. Lactational exposure of DEHP impairs insulin signal transduction and glucose oxidation in the cardiac muscle of the F1 female albino rats, suggesting its possible role in the development of type 2 diabetes.










Similar content being viewed by others
Abbreviations
- ATP:
-
Adenosine triphosphate
- Atf-4:
-
Activating transcription factor 4
- Atf-6:
-
Activating transcription factor 6
- Bip:
-
Binding immunoglobulin protein
- CPM:
-
Counts per minute
- FSH:
-
Follicle-stimulating hormone
- GLUT4:
-
Glucose transporter 4
- IR:
-
Insulin receptor
- IRS-1:
-
Insulin receptor substrate 1
- IU:
-
International units
- JNK:
-
C-Jun N-terminal kinase
- MEHP:
-
Mono-(-2-ethylhexyl phthalate)
- MEHHP:
-
Mono-(2-ethyl-5-hydroxyhexyl) phthalate
- MEOHP:
-
Mono-(2-ethyl-5-oxohexyl) phthalate
- mM:
-
Millimolar
- nM:
-
Nanomolar
- OECD:
-
Organization for economic cooperation and development
- Pdx1:
-
Pancreatic duodenal homeobox-1
- PPARγ:
-
Peroxisome proliferator-activated receptor γ
- PPARα:
-
Peroxisome proliferator-activated receptor α
- Ucp2:
-
Uncoupling protein-2
- μCi:
-
Microcurie
References
Eckardt, K., Taube, A., & Eckel, J. (2011). Obesity-associated insulin resistance in skeletal muscle: Role of lipid accumulation and physical inactivity. Reviews in Endocrine and Metabolic Disorders, 12, 163–172.
Hectors, T. L., Vanparys, C., van der Ven, K., Martens, G. A., Jorens, P. G., Van Gaal, L. F., et al. (2011). Environmental pollutants and type 2 diabetes: A review of mechanisms that can disrupt beta cell function. Diabetologia, 54, 1273–1290.
Kobayashi, K., Miyagawa, M., Wang, R. S., Suda, M., Sekiguchi, S., & Honma, T. (2006). Effects of in utero and lactational exposure to di(2-ethylhexyl)phthalate on somatic and physical development in rat offspring. Industrial Health, 44, 652–660.
Fay, M., Donohue, J. M., & De Rosa, C. (1999). ATSDR evaluation of health effects of chemicals. VI. Di(2-ethylhexyl)phthalate. Agency for toxic substances and disease registry. Toxicology and Industrial Health, 15, 651–746.
FDA. (2002). Safety assessment of Di(2-ethylhexyl)phthalate (DEHP) released from PVC medical devices, (Administration, F.a.D., ed).
ATSDR. (2002). Toxicological Profile for Di(2-ethylhexyl)phthalate (DEHP). Atlanta, GA: Agency for toxic substances and disease registry. Available: http://www.atsdr.cdc.gov/toxprofiles/tp9.html (Accessed 11 August 2003).
NTP-CERHR. (2006). NTP-CERHR monograph on the potential human reproductive and developmental effects of Di(2-Ethylhexyl) Phthalate (DEHP), U.S. Department of Health and Human Services.
Desvergne, B., Feige, J. N., & Casals-Casas, C. (2009). PPAR-mediated activity of phthalates: A link to the obesity epidemic? Molecular and Cellular Endocrinology, 304, 43–48.
Martinelli, M. I., Mocchiutti, N. O., & Bernal, C. A. (2006). Dietary di(2-ethylhexyl)phthalate-impaired glucose metabolism in experimental animals. Human and Experimental Toxicology, 25, 531–538.
Stahlhut, R. W., van Wijngaarden, E., Dye, T. D., Cook, S., & Swan, S. H. (2007). Concentrations of urinary phthalate metabolites are associated with increased waist circumference and insulin resistance in adult U.S. males. Environmental Health Perspectives, 115, 876–882.
Hatch, E. E., Nelson, J. W., Qureshi, M. M., Weinberg, J., Moore, L. L., Singer, M., et al. (2008). Association of urinary phthalate metabolite concentrations with body mass index and waist circumference: A cross-sectional study of NHANES data, 1999–2002. Environmental Health: A Global Access Science Source, 7, 27.
Rengarajan, S., Parthasarathy, C., Anitha, M., & Balasubramanian, K. (2007). Diethylhexyl phthalate impairs insulin binding and glucose oxidation in Chang liver cells. Toxicology In Vitro: An International Journal Published in Association With BIBRA, 21, 99–102.
Srinivasan, C., Khan, A. I., Balaji, V., Selvaraj, J., & Balasubramanian, K. (2011). Diethyl hexyl phthalate-induced changes in insulin signaling molecules and the protective role of antioxidant vitamins in gastrocnemius muscle of adult male rat. Toxicology and Applied Pharmacology, 257, 155–164.
Rajesh, P., Sathish, S., Srinivasan, C., Selvaraj, J., & Balasubramanian, K. (2013). Phthalate is associated with insulin resistance in adipose tissue of male rat: Role of antioxidant vitamins. Journal of Cellular Biochemistry, 114, 558–569.
Calafat, A. M., Slakman, A. R., Silva, M. J., Herbert, A. R., & Needham, L. L. (2004). Automated solid phase extraction and quantitative analysis of human milk for 13 phthalate metabolites. Journal of Chromatography B, Analytical Technologies in the Biomedical and Life Sciences, 805, 49–56.
Latini, G., De Felice, C., Presta, G., Del Vecchio, A., Paris, I., Ruggieri, F., et al. (2003). In utero exposure to di-(2-ethylhexyl)phthalate and duration of human pregnancy. Environmental Health Perspectives, 111, 1783–1785.
Latini, G. (2000). Potential hazards of exposure to di-(2-ethylhexyl)-phthalate in babies. A Review. Biology of the Neonate, 78, 269–276.
WHO. (2002). Global assessment of the state-of-the-science of endocrine disruptors.
Lin, Y., Wei, J., Li, Y., Chen, J., Zhou, Z., Song, L., et al. (2011). Developmental exposure to di(2-ethylhexyl) phthalate impairs endocrine pancreas and leads to long-term adverse effects on glucose homeostasis in the rat. American Journal of Physiology. Endocrinology and Metabolism, 301, E527–E538.
Gillum, N., Karabekian, Z., Swift, L. M., Brown, R. P., Kay, M. W., & Sarvazyan, N. (2009). Clinically relevant concentrations of di (2-ethylhexyl) phthalate (DEHP) uncouple cardiac syncytium. Toxicology and Applied Pharmacology, 236, 25–38.
Posnack, N. G., Lee, N. H., Brown, R., & Sarvazyan, N. (2011). Gene expression profiling of DEHP-treated cardiomyocytes reveals potential causes of phthalate arrhythmogenicity. Toxicology, 279, 54–64.
Johnson, A. D., & Turner, P. C. (1971). Epididymal carbohydrate metabolism. I. Glucose-1-14-C and glucose-6-14-C metabolism by mouse, rat and rabbit tissues. Comparative Biochemistry and Physiology A, Comparative Physiology, 39, 599–604.
Kraft, L. A., & Johnson, A. D. (1972). Epididymal carbohydrate metabolism. II. Substrates and pathway utilization of caput and cauda epididymal tissue from the rabbit, rat and mouse. Comparative Biochemistry and Physiology B, Comparative Biochemistry, 42, 451–461.
Ishizuka, T., Kajita, K., Miura, A., Ishizawa, M., Kanoh, Y., Itaya, S., et al. (1999). DHEA improves glucose uptake via activations of protein kinase C and phosphatidylinositol 3-kinase. The American Journal of Physiology, 276, E196–E204.
Dombrowski, L., Roy, D., Marcotte, B., & Marette, A. (1996). A new procedure for the isolation of plasma membranes, T tubules, and internal membranes from skeletal muscle. The American journal of physiology, 270, E667–E676.
Kristiansen, S., Nielsen, J. N., Bourgoin, S., Klip, A., Franco, M., & Richter, E. A. (2001). GLUT-4 translocation in skeletal muscle studied with a cell-free assay: Involvement of phospholipase D. American Journal of Physiology. Endocrinology and Metabolism, 281, E608–E618.
Lowry, O. H., Rosebrough, N. J., Farr, A. L., & Randall, R. J. (1951). Protein measurement with the Folin phenol reagent. The Journal of Biological Chemistry, 193, 265–275.
Laemmli, U. K. (1970). Cleavage of structural proteins during the assembly of the head of bacteriophage T4. Nature, 227, 680–685.
Latini, G., De Felice, C., & Verrotti, A. (2004). Plasticizers, infant nutrition and reproductive health. Reproductive Toxicology, 19, 27–33.
Hauser, R., & Calafat, A. M. (2005). Phthalates and human health. Occupational and Environmental Medicine, 62, 806–818.
Faouzi, M. A., Dine, T., Gressier, B., Kambia, K., Luyckx, M., Pagniez, D., et al. (1999). Exposure of hemodialysis patients to di-2-ethylhexyl phthalate. International Journal of Pharmaceutics, 180, 113–121.
Shneider, B., Schena, J., Truog, R., Jacobson, M., & Kevy, S. (1989). Exposure to di(2-ethylhexyl)phthalate in infants receiving extracorporeal membrane oxygenation. The New England Journal of Medicine, 320, 1563.
Davis, B. J., Maronpot, R. R., & Heindel, J. J. (1994). Di-(2-ethylhexyl) phthalate suppresses estradiol and ovulation in cycling rats. Toxicology and Applied Pharmacology, 128, 216–223.
Treinen, K. A., Dodson, W. C., & Heindel, J. J. (1990). Inhibition of FSH-stimulated cAMP accumulation and progesterone production by mono(2-ethylhexyl) phthalate in rat granulosa cell cultures. Toxicology and Applied Pharmacology, 106, 334–340.
Young, L. H. (2010). Diet-induced obesity obstructs insulin signaling in the heart. American Journal of Physiology. Heart and Circulatory Physiology, 298, H306–H307.
Belke, D. D., Betuing, S., Tuttle, M. J., Graveleau, C., Young, M. E., Pham, M., et al. (2002). Insulin signaling coordinately regulates cardiac size, metabolism, and contractile protein isoform expression. The Journal of Clinical Investigation, 109, 629–639.
Muniyappa, R., Montagnani, M., Koh, K. K., & Quon, M. J. (2007). Cardiovascular actions of insulin. Endocrine Reviews, 28, 463–491.
Gayathri, N. S., Dhanya, C. R., Indu, A. R., & Kurup, P. A. (2004). Changes in some hormones by low doses of di (2-ethyl hexyl) phthalate (DEHP), a commonly used plasticizer in PVC blood storage bags & medical tubing. The Indian Journal of Medical Research, 119, 139–144.
Livingstone, C., & Collison, M. (2002). Sex steroids and insulin resistance. Clinical Science, 102, 151–166.
Svensson, K., Hernandez-Ramirez, R. U., Burguete-Garcia, A., Cebrian, M. E., Calafat, A. M., Needham, L. L., et al. (2011). Phthalate exposure associated with self-reported diabetes among Mexican women. Environmental Research, 111, 792–796.
Ferre, P. (2004). The biology of peroxisome proliferator-activated receptors: Relationship with lipid metabolism and insulin sensitivity. Diabetes, 53(Suppl 1), S43–S50.
Brun, R. P., Kim, J. B., Hu, E., & Spiegelman, B. M. (1997). Peroxisome proliferator-activated receptor gamma and the control of adipogenesis. Current Opinion in Lipidology, 8, 212–218.
Tontonoz, P., Nagy, L., Alvarez, J. G., Thomazy, V. A., & Evans, R. M. (1998). PPARgamma promotes monocyte/macrophage differentiation and uptake of oxidized LDL. Cell, 93, 241–252.
Batista, T. M., Alonso-Magdalena, P., Vieira, E., Amaral, M. E., Cederroth, C. R., Nef, S., et al. (2012). Short-term treatment with bisphenol-A leads to metabolic abnormalities in adult male mice. PLoS One, 7, e33814.
Desrois, M., Sidell, R. J., Gauguier, D., King, L. M., Radda, G. K., & Clarke, K. (2004). Initial steps of insulin signaling and glucose transport are defective in the type 2 diabetic rat heart. Cardiovascular Research, 61, 288–296.
Pessin, J. E., & Saltiel, A. R. (2000). Signaling pathways in insulin action: Molecular targets of insulin resistance. The Journal of Clinical Investigation, 106, 165–169.
Santhosh, A., Nair, K. G., Arun, P., Deepadevi, K. V., Manojkumar, V., Lakshmi, L. R., et al. (1998). Effect of DEHP [di-(2-ethyl hexyl) phthalate] on lipid peroxidation in liver in rats and in primary cultures of rat hepatocytes. The Indian Journal of Medical Research, 108, 17–23.
Garcia-Arencibia, M., Davila, N., Campion, J., Carmen Carranza, M., & Calle, C. (2005). Identification of two functional estrogen response elements complexed with AP-1-like sites in the human insulin receptor gene promoter. The Journal of Steroid Biochemistry and Molecular Biology, 94, 1–14.
Xie, P., Liu, M. L., Gu, Y. P., Lu, J., Xu, X., Zeng, W. M., et al. (2003). Oestrogen improves glucose metabolism and insulin signal transduction in HepG2 cells. Clinical and Experimental Pharmacology and Physiology, 30, 643–648.
Khan, A. H., & Pessin, J. E. (2002). Insulin regulation of glucose uptake: a complex interplay of intracellular signalling pathways. Diabetologia, 45, 1475–1483.
Kaneto, H., Katakami, N., Matsuhisa, M., & Matsuoka, T. A. (2010). Role of reactive oxygen species in the progression of type 2 diabetes and atherosclerosis. Mediators of Inflammation, 2010, 453892.
Potashnik, R., Bloch-Damti, A., Bashan, N., & Rudich, A. (2003). IRS1 degradation and increased serine phosphorylation cannot predict the degree of metabolic insulin resistance induced by oxidative stress. Diabetologia, 46, 639–648.
Pirola, L., Johnston, A. M., & Van Obberghen, E. (2004). Modulation of insulin action. Diabetologia, 47, 170–184.
Rusyn, I., Kadiiska, M. B., Dikalova, A., Kono, H., Yin, M., Tsuchiya, K., et al. (2001). Phthalates rapidly increase production of reactive oxygen species in vivo: Role of Kupffer cells. Molecular Pharmacology, 59, 744–750.
Peraldi, P., Xu, M., & Spiegelman, B. M. (1997). Thiazolidinediones block tumor necrosis factor-alpha-induced inhibition of insulin signaling. The Journal of Clinical Investigation, 100, 1863–1869.
Teruel, T., Hernandez, R., & Lorenzo, M. (2001). Ceramide mediates insulin resistance by tumor necrosis factor-alpha in brown adipocytes by maintaining Akt in an inactive dephosphorylated state. Diabetes, 50, 2563–2571.
Slot, J. W., Geuze, H. J., Gigengack, S., James, D. E., & Lienhard, G. E. (1991). Translocation of the glucose transporter GLUT4 in cardiac myocytes of the rat. Proceedings of the National Academy of Sciences of the United States of America, 88, 7815–7819.
Uphues, I., Kolter, T., Goud, B., & Eckel, J. (1995). Failure of insulin-regulated recruitment of the glucose transporter GLUT4 in cardiac muscle of obese Zucker rats is associated with alterations of small-molecular-mass GTP-binding proteins. The Biochemical Journal, 311(Pt 1), 161–166.
Russell, R. R, 3rd, Bergeron, R., Shulman, G. I., & Young, L. H. (1999). Translocation of myocardial GLUT-4 and increased glucose uptake through activation of AMPK by AICAR. The American Journal of Physiology, 277, H643–H649.
Finck, B. N., Bernal-Mizrachi, C., Han, D. H., Coleman, T., Sambandam, N., LaRiviere, L. L., et al. (2005). A potential link between muscle peroxisome proliferator- activated receptor-alpha signaling and obesity-related diabetes. Cell Metabolism, 1, 133–144.
Lizunov, V. A., Matsumoto, H., Zimmerberg, J., Cushman, S. W., & Frolov, V. A. (2005). Insulin stimulates the halting, tethering, and fusion of mobile GLUT4 vesicles in rat adipose cells. The Journal of Cell Biology, 169, 481–489.
Lapinskas, P. J., Brown, S., Leesnitzer, L. M., Blanchard, S., Swanson, C., Cattley, R. C., et al. (2005). Role of PPARalpha in mediating the effects of phthalates and metabolites in the liver. Toxicology, 207, 149–163.
Park, S. Y., Cho, Y. R., Kim, H. J., Higashimori, T., Danton, C., Lee, M. K., et al. (2005). Unraveling the temporal pattern of diet-induced insulin resistance in individual organs and cardiac dysfunction in C57BL/6 mice. Diabetes, 54, 3530–3540.
Acknowledgments
Financial assistance from UGC-SAP-DRS, UGC-ASIST and DST-FIST programs are gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mangala Priya, V., Mayilvanan, C., Akilavalli, N. et al. Lactational Exposure of Phthalate Impairs Insulin Signaling in the Cardiac Muscle of F1 Female Albino Rats. Cardiovasc Toxicol 14, 10–20 (2014). https://doi.org/10.1007/s12012-013-9233-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12012-013-9233-z