Abstract
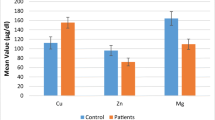
Trace elements, through their interaction with biomolecules, can play an important role in the pathophysiology of bipolar disorder and protect against oxidative stress effects. The purpose of this study is to examine plasma concentration levels of zinc (Zn) and copper (Cu) of Algerian patients, diagnosed with bipolar disorder, and to compare these levels with those of healthy controls. The Cu/Zn ratio was calculated to explore a possible correlation between these elements and lipid peroxidation in the study groups. A total of 33 patients diagnosed with bipolar disorder and 38 healthy subjects participated in this study. Plasma copper and zinc concentrations were measured using a polarographic analyzer. The marker of plasma lipid peroxidation (Malondialdehyde: MDA) was determined by UV spectrophotometry. Plasma Cu concentrations were higher in patients compared to controls (p < 0.05), while the Zn level was significantly lower. Consequently, the Cu/Zn ratio was significantly different between patients and controls. Regarding MDA, no significant difference was noticed between the two study groups. However, in patients, a negative correlation was found between MDA and Cu/Zn ratio (r= −0.38, p= 0.027). These results suggested that an elevated Cu/Zn ratio is associated with attenuated lipid peroxidation in our bipolar patients.


Similar content being viewed by others
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Sussulini A, Banzato CE, Arruda MA (2011) Exploratory analysis of the serum ionomic profile for bipolar disorder and lithium treatment. Int J Mass Spectrom 307:182–184. https://doi.org/10.1016/j.ijms.2010.11.013
Eroglu MZ, Karakus G, Tamam L (2013) Bipolar disorder and suicide. Dusunen Adam 26:139. https://doi.org/10.5350/DAJPN2013260203
Rowland TA, Marwaha S (2018) Epidemiology and risk factors for bipolar disorder. Ther Adv Psychopharmacol 8:251–269. https://doi.org/10.1177/2045125318769235
Esan O, Esan A (2016) Epidemiology and burden of bipolar disorder in Africa: a systematic review of data from Africa. Soc Psychiatry Psychiatr Epidemiol 51:93–100. https://doi.org/10.1007/s00127-015-1091-5
Świądro M, Ordon K, Herman M, Dudek D, Wietecha-Posłuszny R (2021) Copper and Zinc as Potential Biomarkers of Mood Disorders and Pandemic Syndrome. Molecules 27:91. https://doi.org/10.3390/molecules27010091
Siwek M, Sowa-Kućma M, Styczeń K, Szewczyk B, Reczyński W et al (2016) Decreased serum zinc concentration during depressive episode in patients with bipolar disorder. J Affect Disord 190:272–277. https://doi.org/10.1016/j.jad.2015.10.026
Styczeń K, Sowa-Kućma M, Siwek M, Dudek D, Reczyński W et al (2016) Study of the serum copper levels in patients with major depressive disorder. Biol Trace Elem Res 174:287–293. https://doi.org/10.1007/s12011-016-0720-5
Mravunac M, Szymlek-Gay EA, Daly RM, Roberts BR, Formica M et al (2019) Greater circulating copper concentrations and copper/zinc ratios are associated with lower psychological distress, but not cognitive performance, in a sample of Australian older adults. Nutrients 11:2503. https://doi.org/10.3390/nu11102503
Andreazza AC, Wang JF, Salmasi F, Shao L, Young LT (2013) Specific subcellular changes in oxidative stress in prefrontal cortex from patients with bipolar disorder. J Neurochem 127:552–561. https://doi.org/10.1111/jnc.12316
Jiménez-Fernández S, Gurpegui M, Garrote-Rojas D, Gutiérrez-Rojas L, Carretero MD et al (2021) Oxidative stress parameters and antioxidants in patients with bipolar disorder: Results from a meta-analysis comparing patients, including stratification by polarity and euthymic status, with healthy controls. Bipolar Disord 23:117–129. https://doi.org/10.1111/bdi.12980
Liu T, Zhong S, Liao X, Chen J, He T et al (2015) A meta-analysis of oxidative stress markers in depression. PLoS One 10:e0138904. https://doi.org/10.1371/journal.pone.0138904
Maes M, Landucci Bonifacio K, Morelli NR, Vargas HO, Barbosa DS, et al. (2019) Major differences in neurooxidative and neuronitrosative stress pathways between major depressive disorder and types I and II bipolar disorder. Mol Neurobiol 56: 141-156. https://doi.org/10.1007/s12035-018-1051-7.
Kazi Tani LS, Gourlan AT, Dennouni-Medjati N, Telouk P, Dali-Sahi M et al (2021) Copper isotopes and copper to zinc ratio as possible biomarkers for thyroid cancer. Front Med 8:698167. https://doi.org/10.3389/fmed.2021.698167
Malavolta M, Piacenza F, Basso A, Giacconi R, Costarelli L et al (2015) Serum copper to zinc ratio: Relationship with aging and health status. Mech Ageing Dev 151:93–100. https://doi.org/10.1016/j.mad.2015.01.004
Attar T, Dennouni-Medjati N, Harek Y, Larabi L (2013) Determination of zinc levels in healthy adults from the west of algeria by differential pulse anodic stripping voltammetry. J Adv Chem 6:855–860. https://doi.org/10.24297/jac.v6i1.964
Attar T, Harek Y, Larabi L (2014) Determination of copper in whole blood by differential pulse adsorptive stripping voltammetry. Mediterr J Chem 2:691–700. https://doi.org/10.13171/mjc.2.6.2014.21.02.25
Nourooz-Zadeh J (1999) Ferrous ion oxidation in presence of xylenol orange for detection of lipid hydroperoxides in plasma. In: Methods in enzymology. Elsevier, pp 58–62
Ivanova ID, Pal A, Simonelli I, Atanasova B, Ventriglia M et al (2022) Evaluation of zinc, copper, and Cu: Zn ratio in serum, and their implications in the course of COVID-19. J Trace Elem Med Biol 71:126944. https://doi.org/10.1016/j.jtemb.2022.126944
Caroli S, Alimonti A, Coni E, Petrucci F, Senofonte O et al (1994) The assessment of reference values for elements in human biological tissues and fluids: a systematic review. Crit Rev Anal Chem 24:363–398. https://doi.org/10.1080/10408349408048824
Linter C (1985) Neuropsychiatric aspects of trace elements. Br J Hosp Med (Lond) 34:361–365
Mustak MS, Rao TS, Shanmugavelu P, Sundar NS, Menon RB et al (2008) Assessment of serum macro and trace element homeostasis and the complexity of inter-element relations in bipolar mood disorders. Clin Chim Acta 394:47–53. https://doi.org/10.1016/j.cca.2008.04.003
Prakash A, Bharti K, Majeed ABA (2015) Zinc: indications in brain disorders. Fundam Clin Pharmacol 29:131–149. https://doi.org/10.1111/fcp.12110
Islam MR, Islam MR, Shalahuddin Qusar M, Islam MS, Kabir MH et al (2018) Alterations of serum macro-minerals and trace elements are associated with major depressive disorder: a case-control study. BMC Psychiatry 18:1–7. https://doi.org/10.1186/s12888-018-1685-z
Chowdhury MI, Hasan M, Islam MS, Sarwar MS, Amin MN et al (2017) Elevated serum MDA and depleted non-enzymatic antioxidants, macro-minerals and trace elements are associated with bipolar disorder. J Trace Elem Med Biol 39:162–168. https://doi.org/10.1016/j.jtemb.2016.09.012
González-Estecha M, Trasobares EM, Tajima K, Cano S, Fernández C et al (2011) Trace elements in bipolar disorder. J Trace Elem Med Biol 25:S78–S83. https://doi.org/10.1016/j.jtemb.2010.10.015
Misztak P, Opoka W, Topór-Mądry R, Nowak G, Rybakowski JK (2017) The serum concentration of copper in bipolar disorder. Psychiatr Pol 51:469–481. https://doi.org/10.12740/PP/OnlineFirst/65250
Manser WW, Khan MA, Hasan KZ (1989) Trace element studies on Karachi population. Part IV: blood copper, zinc, magnesium and lead levels in psychiatric patients with depression, mental retardation and seizure disorders. J Pak Med Assoc 39:269–274
Heitland P, Köster HD (2006) Biomonitoring of 37 trace elements in blood samples from inhabitants of northern Germany by ICP–MS. J Trace Elem Med Biol 20:253–262. https://doi.org/10.1016/j.jtemb.2006.08.001
Squitti R, Pal A, Picozza M, Avan A, Ventriglia M et al (2020) Zinc Therapy in early Alzheimer’s disease: Safety and potential therapeutic efficacy. Biomolecules 10:1164. https://doi.org/10.3390/biom10081164
Kotzalidis GD, Ambrosi E, Simonetti A, Cuomo I, Casale AD et al (2015) Neuroinflammation in bipolar disorders. Neuroimmunol Neuroinflamm 2:252–262. https://doi.org/10.4103/2347-8659.167309
Bailey SL, Carpentier PA, McMahon EJ, Begolka WS, Miller SD (2006) Innate and adaptive immune responses of the central nervous system. Crit Rev Immunol 26:149–188. https://doi.org/10.1615/critrevimmunol.v26.i2.40
Bajramovic J (2011) Regulation of innate immune responses in the central nervous system. CNS Neurol Disord Drug Targets 10:4–24. https://doi.org/10.2174/187152711794488610
Kitazawa M, Hsu H-W, Medeiros R (2016) Copper exposure perturbs brain inflammatory responses and impairs clearance of amyloid-beta. Toxicol Sci 152:194–204. https://doi.org/10.1093/toxsci/kfw081
Hu Z, Yu F, Gong P, Qiu Y, Zhou W et al (2014) Subneurotoxic copper (II)-induced NF-κB-dependent microglial activation is associated with mitochondrial ROS. Toxicol Appl Pharmacol 276:95–103. https://doi.org/10.1016/j.taap.2014.01.020
Zucconi GG, Cipriani S, Scattoni R, Balgkouranidou I, Hawkins D et al (2007) Copper deficiency elicits glial and neuronal response typical of neurodegenerative disorders. Neuropathol Appl Neurobiol. 33:212–225. https://doi.org/10.1111/j.1365-2990.2006.00793.x
Brewer GJ Copper excess, zinc deficiency, and cognition loss in Alzheimer’s disease. BioFactors (Oxford, England) 38(2):107–113. https://doi.org/10.1002/biof.1005
Sarris J, Ravindran A, Yatham LN, Marx W, Rucklidge JJ et al (2022) Clinician guidelines for the treatment of psychiatric disorders with nutraceuticals and phytoceuticals: The World Federation of Societies of Biological Psychiatry (WFSBP) and Canadian Network for Mood and Anxiety Treatments (CANMAT) Taskforce. World J Biol Psychiatry 23:424–455. https://doi.org/10.1080/15622975.2021.2013041
Kabzinska-Milewska K, Czajeczny D, Wójciak RW (2021) Effect of lithium treatment on the content of lithium, copper, calcium, magnesium, zinc and iron in the hair of patients with bipolar disorder. J Elem 26. https://doi.org/10.5601/jelem.2021.26.3.2172
Beyer JL, Payne ME (2016) Nutrition and bipolar depression. Psychiatric. Clinics 39:75–86. https://doi.org/10.1016/j.psc.2015.10.003
Alpers DH (2017) Les limites pharmacocinétiques pour définir la dose adéquate de la supplémentation en zinc. Bull Acad Natl Med 201:431–438. https://doi.org/10.1016/S0001-4079(19)30512-6
Wolf TL, Kotun J, Meador-Woodruff JH (2006) Plasma copper, iron, ceruloplasmin and ferroxidase activity in schizophrenia. Schizophr Res 86:167–171. https://doi.org/10.1016/j.schres.2006.05.027
Vacheron-Trystram M-N, Braitman A, Cheref S, Auffray L (2004) Antipsychotiques et troubles bipolaires. L'Encéphale 30:417–424. https://doi.org/10.1016/S0013-7006(04)95456-5
Khadir S, Lafendi M (2020) Intérêt du Suivi Thérapeutique Pharmacologique des thymorégulateurs dans la prise en charge des patients bipolaires du Service de Psychiatrie du CHU-Tlemcen. Thèse pour l’obtention du diplôme de docteur en pharmacie, Université de Tlemcen. http://dspace.univ-tlemcen.dz/handle/112/18370
Kawahara M, Tanaka K-i, Kato-Negishi M (2022) Copper Biology in Health and Disease: Crosstalk of copper and zinc in the pathogenesis of vascular dementia. J Clin Biochem Nutr 71:7. https://doi.org/10.3164/jcbn.22-40
Kuloglu M, Ustundag B, Atmaca M, Canatan H, Tezcan AE et al (2002) Lipid peroxidation and antioxidant enzyme levels in patients with schizophrenia and bipolar disorder. Cell Biochem Funct 20:171–175. https://doi.org/10.1002/cbf.940
Maes M, Yirmyia R, Noraberg J, Brene S, Hibbeln J et al (2009) The inflammatory & neurodegenerative (I&ND) hypothesis of depression: leads for future research and new drug developments in depression. Metab Brain Dis 24:27–53. https://doi.org/10.1007/s11011-008-9118-1
Fornito A, Malhi G, Lagopoulos J, Ivanovski B, Wood SJ et al (2007) In vivo evidence for early neurodevelopmental anomaly of the anterior cingulate cortex in bipolar disorder. Acta Psychiatr Scand 116:467–472. https://doi.org/10.1111/j.1600-0447.2007.01069.x
Duan L, Cheng Y, Jin Y (2010) Effect of copper intake and copper-zinc ratio on rat lipid peroxidation in copper deficiency. Wei Sheng Yan Jiu= J Hyg Res 39:25–28
Roughead ZK, Johnson LK, Hunt JR (1999) Dietary copper primarily affects antioxidant capacity and dietary iron mainly affects iron status in a surface response study of female rats fed varying concentrations of iron, zinc and copper. J Nutr 129:1368–1376. https://doi.org/10.1093/jn/129.7.1368
Mezzetti A, Pierdomenico SD, Costantini F, Romano F, De Cesare D et al (1998) Copper/zinc ratio and systemic oxidant load: effect of aging and aging-related degenerative diseases. Free Radic Biol Med 25:676–681. https://doi.org/10.1016/S0891-5849(98)00109-9
Acknowledgements
We are grateful to the patients and healthy volunteers who participated in this study.
Funding
This work was supported by the General Direction of Scientific Research and Technological Development (DGRSDT), as part of the socio-economic research project entitled “Implication of micronutrients in the development of certain pathologies in western Algeria” (Project No. 12/Univ-Tlemcen/DGRSDT, 2019, Algeria).
Author information
Authors and Affiliations
Contributions
Nouria Dennouni-Medjati conceived the study design. Ikram Chebieb and Cherifa Benosman collected the sample and data via face-to-face interviews. Yahia Harek performed the Cu and Zn measurements. Ikram Chebieb and Baya Guermouche analyzed MDA. Ikram Chebieb and Youssouf Kachekouche performed the statistical analysis. Ikram Chebieb and Nouria Dennouni-Medjati prepared the first draft of the manuscript. Nouria Dennouni-Medjati and Majda Dali-Sahi corrected the final version. All authors read and approved the final version.
Corresponding author
Ethics declarations
Ethics Approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the scientific council of the faculty as well as the ethics and deontology committee of the University of Tlemcen (CEDUT 03/07/2018).
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Consent for Publication
Not applicable
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chebieb, I., Medjati, N.D., Harek, Y. et al. Imbalance of Plasma Copper and Zinc Levels and the Association Between the Cu/Zn Ratio and Lipid Peroxidation in Algerian Bipolar Patients. Biol Trace Elem Res 202, 2450–2456 (2024). https://doi.org/10.1007/s12011-023-03858-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-023-03858-y