Abstract
Purpose of Review
The purpose of this review article is to highlight the current role of diagnostic imaging in the assessment of inflammatory myopathies.
Recent Findings
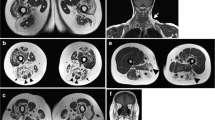
Recent research demonstrates that imaging plays an important role in evaluating patients with symptoms of an inflammatory myopathy. In general, MRI is the pivotal imaging modality for assessing inflammatory myopathies, revealing precise anatomic details because of changes in the signal intensity of the muscles. Whole-body MR imaging has become increasingly important over the last several years. US is also a valuable imaging modality for scanning muscles.
Summary
Together with the clinical history, familiarity with the imaging features of inflammatory myopathies is essential for formulating an accurate diagnosis.











Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
•• Dalakas MC. Inflammatory muscle diseases. N Engl J Med. 2015;373:393–4 In this study Dalaks provides a thorough description of the inflammatory muscle diseases.
Murphy WA, Totty WG, Carroll JE. MRI of normal and pathologic skeletal muscle. AJR Am J Roentgenol. 1986;146:565–74.
Wattjes MP, Kley RA, Fischer D. Neuromuscular imaging in inherited muscle diseases. Eur Radiol. 2010;20:2447–60.
Lenk S, Fischer S, Kotter I, Claussen CD, Schlemmer HP. Possibilities of whole-body MRI for investigating musculoskeletal diseases. Radiologe. 2004;44:844–53.
Filli L, Maurer B, Manoliu A, Andreisek G, Guggenberger R. Whole-body MRI in adult inflammatory myopathies: do we need imaging of the trunk? Eur Radiol. 2015;25:3499–507.
Bashir WA, O’Donnell P. The myositides: the role of imaging in diagnosis and treatment. Semin Musculoskelet Radiol. 2010;14:217–26.
Garcia J. MRI in inflammatory myopathies. Skelet Radiol. 2000;29:425–38.
May DA, Disler DG, Jones EA, Balkissoon AA, Manaster BJ. Abnormal signal intensity in skeletal muscle at MR imaging: patterns, pearls, and pitfalls. Radiographics 2000;20 Spec No:S295–S315.
Van De Vlekkert J, Maas M, Hoogendijk JE, De Visser M, Van Schaik IN. Combining MRI and muscle biopsy improves diagnostic accuracy in subacute-onset idiopathic inflammatory myopathy. Muscle Nerve. 2015;51:253–8.
Del Grande F, Carrino JA, Del Grande M, Mammen AL, Stine LC. Magnetic resonance imaging of inflammatory myopathies. Top Magn Reson Imaging. 2011;22:39–43.
Boutry N, Hachulla E, Zanetti-Musielak C, Morel M, Demondion X, Cotten A. Imaging features of musculoskeletal involvement in systemic sclerosis. Eur Radiol. 2007;17:1172–80.
Schick F. Whole-body MRI at high field: technical limits and clinical potential. Eur Radiol. 2005;15:946–59.
Sookhoo S, Mackinnon I, Bushby K, Chinnery PF, Birchall D. MRI for the demonstration of subclinical muscle involvement in muscular dystrophy. Clin Radiol. 2007;62:160–5.
Shelly MJ, Bolster F, Foran P, Crosbie I, Kavanagh EC, Eustace SJ. Whole-body magnetic resonance imaging in skeletal muscle disease. Semin Musculoskelet Radiol. 2010;14:47–56.
•• Day J, Patel S, Limaye V. The role of magnetic resonance imaging techniques in evaluation and management of the idiopathic inflammatory myopathies. Semin Arthritis Rheum. 2017;46:642–9 This study examines the role of MRI in evaluation of the idiopathic inflammatory myopathies and shows that MRI has a clear role in aiding diagnosis of these conditions, guiding muscle biopsy, differentiating subtypes a pattern-based approach, and monitoring disease activity in a longitudinal fashion. Also shows that whole body MRI is an emerging technique that offers several advantages over regional MRI.
Adler RS, Garofalo G. Ultrasound in the evaluation of the inflammatory myopathies. Curr Rheumatol Rep. 2009;11:302–8.
Connell DA, Schneider-Kolsky ME, Hoving JL, Malara F, Buchbinder R, Koulouris G, et al. Longitudinal study comparing sonographic and MRI assessments of acute and healing hamstring injuries. AJR Am J Roentgenol. 2004;183:975–84.
Vilela VS, Prieto-Gonzalez S, Milisenda JC, Selva OCA, Grau JM. Polymyositis, a very uncommon isolated disease: clinical and histological re-evaluation after long-term follow-up. Rheumatol Int. 2015;35:915–20.
Chahin N, Engel AG. Correlation of muscle biopsy, clinical course, and outcome in PM and sporadic IBM. Neurology. 2008;70:418–24.
Smitaman E, Flores DV, Gomez CM, Pathria MN. MR imaging of atraumatic muscle disorders. Radiographics. 2018;38:500–22.
Huang ZG, Gao BX, Chen H, Yang MX, Chen XL, Yan R, et al. An efficacy analysis of whole-body magnetic resonance imaging in the diagnosis and follow-up of polymyositis and dermatomyositis. PLoS One. 2017;12:e0181069.
Verschuuren J, Cox FM, van Engelen B, de Visser M, Badrising UA. Inflammatory myopathies. In: Wattjes MP, Fischer D, editors. Neuromuscular imaging. New York: Springer Science; 2013. p. 321–34.
O’Connell MJ, Powell T, Brennan D, Lynch T, McCarthy CJ, Eustace SJ. Whole-body MR imaging in the diagnosis of polymyositis. AJR Am J Roentgenol. 2002;179:967–71.
Tomasova SJ, Charvat F, Jarosova K, Vencovsky J. The role of MRI in the assessment of polymyositis and dermatomyositis. Rheumatology. 2007;46:1174–9.
Muro Y, Sugiura K, Akiyama M. Cutaneous manifestations in dermatomyositis: key clinical and serological features—a comprehensive review. Clin Rev Allergy Immunol. 2016;51:293–302.
Engel AG, Hohlfeld R. The polymyositis and dermatomyositis complex. In: Engel AG, Franzini-Armstrong C, editors. Myology. New York: McGraw-Hill; 2008. p. 1335–83.
Ghirardello A, Zampieri S, Iaccarino L, Tarricone E, Bendo R, Gambari PF, et al. Anti-Mi-2 antibodies. Autoimmunity. 2005;38:79–83.
Schulze M, Kotter I, Ernemann U, Fenchel M, Tzaribatchev N, Claussen CD, et al. MRI findings in inflammatory muscle diseases and their noninflammatory mimics. AJR Am J Roentgenol. 2009;192:1708–16.
Zheng Y, Liu L, Wang L, Xiao J, Wang Z, Lv H, et al. Magnetic resonance imaging changes of thigh muscles in myopathy with antibodies to signal recognition particle. Rheumatology. 2015;54:1017–24.
Pipitone N, Notarnicola A, Levrini G, Spaggiari L, Scardapane A, Iannone F, et al. Do dermatomyositis and polymyositis affect different thigh muscle groups? A comparative MRI-based study. Ann Rheum Dis. 74.
Hesla RB, Karlson LK, McCauley RG. Milk of calcium fluid collection in dermatomyositis: ultrasound findings. Pediatr Radiol. 1990;20:344–6.
de Castro TC, Guarniero R, Giacomin MF, Meneghin MB, Martins GB, Lotufo Sde A. “Milk of calcium”: a rare presentation of calcinosis. Rev Bras Reumatol. 2014;54:65–7.
Suzuki S, Nishikawa A, Kuwana M, Nishimura H, Watanabe Y, Nakahara J, et al. Inflammatory myopathy with anti-signal recognition particle antibodies: case series of 100 patients. Orphanet J Rare Dis. 2015;10:61.
Watanabe Y, Uruha A, Suzuki S, Nakahara J, Hamanaka K, Takayama K, et al. Clinical features and prognosis in anti-SRP and anti-HMGCR necrotising myopathy. J Neurol Neurosurg Psychiatry. 2016;87:1038–44.
Pinal-Fernandez I, Casal-Dominguez M, Carrino JA, Lahouti AH, Basharat P, Albayda J, et al. Thigh muscle MRI in immune-mediated necrotising myopathy: extensive oedema, early muscle damage and role of anti-SRP autoantibodies as a marker of severity. Ann Rheum Dis. 2017;76:681–7.
Pelissou C, Lerolle N, Labeyrie C, Durand E, Besson FL. 18F-FDG PET/CT and MRI in necrotizing autoimmune myopathy: “the scarface sign”. Clin Nucl Med. 2018;43:147–9.
Pinal-Fernandez I, Casal-Dominguez M, Mammen AL. Immune-mediated necrotizing myopathy. Curr Rheumatol Rep. 2018;20:21.
Mastaglia FL, Phillips BA. Idiopathic inflammatory myopathies: epidemiology, classification, and diagnostic criteria. Rheum Dis Clin N Am. 2002;28:723–41.
de Camargo LV, de Carvalho MS, Shinjo SK, de Oliveira ASB, Zanoteli E. Clinical, histological, and immunohistochemical findings in inclusion body myositis. Biomed Res Int. 2018;2018:5069042.
Lloyd TE, Mammen AL, Amato AA, Weiss MD, Needham M, Greenberg SA. Evaluation and construction of diagnostic criteria for inclusion body myositis. Neurology. 2014;83:426–33.
Weihl CC, Mammen AL. Sporadic inclusion body myositis—a myodegenerative disease or an inflammatory myopathy. Neuropathol Appl Neurobiol. 2017;43:82–91.
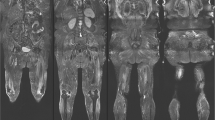
•• Guimaraes JB, Zanoteli E, Link TM, de Camargo LV, Facchetti L, Nardo L, et al. Sporadic inclusion body myositis: MRI findings and correlation with clinical and functional parameters. AJR Am J Roentgenol. 2017;209:1340–7 This study suggests that most patients with biopsy-proven sporadic IBM present with a typical pattern of muscle involvement at MRI and these findings strongly correlated with clinical and functional parameters.
Tasca G, Monforte M, De Fino C, Kley RA, Ricci E, Mirabella M. Magnetic resonance imaging pattern recognition in sporadic inclusion-body myositis. Muscle Nerve. 2015;52:956–62.
Escola-Verge L, Pinal-Fernandez I, Fernandez-Codina A, Callejas-Moraga EL, Espinosa J, Marin A, et al. Mixed connective tissue disease and epitope spreading: an historical cohort study. J Clin Rheumatol. 2017;23:155–9.
Trallero-Araguas E, Grau-Junyent JM, Labirua-Iturburu A, Garcia-Hernandez FJ, Monteagudo-Jimenez M, Fraile-Rodriguez G, et al. Clinical manifestations and long-term outcome of anti-Jo1 antisynthetase patients in a large cohort of Spanish patients from the GEAS-IIM group. Semin Arthritis Rheum. 2016;46:225–31.
Pinal-Fernandez I, Casal-Dominguez M, Huapaya JA, Albayda J, Paik JJ, Johnson C, et al. A longitudinal cohort study of the anti-synthetase syndrome: increased severity of interstitial lung disease in black patients and patients with anti-PL7 and anti-PL12 autoantibodies. Rheumatology. 2017;56:999–1007.
Noguchi E, Uruha A, Suzuki S, Hamanaka K, Ohnuki Y, Tsugawa J, et al. Skeletal muscle involvement in antisynthetase syndrome. JAMA Neurol. 2017;74:992–9.
Andersson H, Kirkhus E, Garen T, Walle-Hansen R, Merckoll E, Molberg O. Comparative analyses of muscle MRI and muscular function in anti-synthetase syndrome patients and matched controls: a cross-sectional study. Arthritis Res Ther. 2017;19:17.
Wattjes MP, Fischer D. Neuromuscular imaging. Berlin: Springer; 2013.
Dalakas MC. Toxic and drug-induced myopathies. J Neurol Neurosurg Psychiatry. 2009;80:832–8.
Pasnoor M, Barohn RJ, Dimachkie MM. Toxic myopathies. Curr Opin Neurol. 2018;31:575–82.
Pasnoor M, Barohn RJ, Dimachkie MM. Toxic myopathies. Neurol Clin. 2014;32:647–70 viii.
Mammen AL. Toxic myopathies. Continuum. 2013;19:1634–49.
Shulman LE. Diffuse fasciitis with hypergammaglobulinemia and eosinophilia: a new syndrome? J Rheumatol. 1984;11:569–70.
Helfman T, Falanga V. Eosinophilic fasciitis. Clin Dermatol. 1994;12:449–55.
Doyle JA, Ginsburg WW. Eosinophilic fasciitis. Med Clin N Am. 1989;73:1157–66.
Moulton SJ, Kransdorf MJ, Ginsburg WW, Abril A, Persellin S. Eosinophilic fasciitis: spectrum of MRI findings. AJR Am J Roentgenol. 2005;184:975–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Imaging
Rights and permissions
About this article
Cite this article
Guimarães, J.B., Nico, M.A., Omond, A.G. et al. Diagnostic Imaging of Inflammatory Myopathies: New Concepts and a Radiological Approach. Curr Rheumatol Rep 21, 8 (2019). https://doi.org/10.1007/s11926-019-0807-z
Published:
DOI: https://doi.org/10.1007/s11926-019-0807-z