Abstract
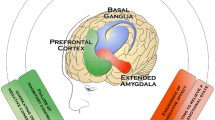
There exists a continuous spectrum of overeating, where at the extremes there are casual overindulgences and at the other a ‘pathological’ drive to consume palatable foods. It has been proposed that pathological eating behaviors may be the result of addictive appetitive behavior and loss of ability to regulate the consumption of highly processed foods containing refined carbohydrates, fats, salt, and caffeine. In this review, we highlight the genetic similarities underlying substance addiction phenotypes and overeating compulsions seen in individuals with binge eating disorder. We relate these similarities to findings from neuroimaging studies on reward processing and clinical diagnostic criteria based on addiction phenotypes. The abundance of similarities between compulsive overeating and substance addictions puts forth a case for a ‘food addiction’ phenotype as a valid, diagnosable disorder.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
James W. The epidemiology of obesity: the size of the problem. J Intern Med. 2008;263(4):336–52.
Sorof J, Daniels S. Obesity hypertension in children a problem of epidemic proportions. Hypertension. 2002;40(4):441–7.
Landsberg L, Aronne LJ, Beilin LJ, Burke V, Igel LI, Lloyd‐Jones D, et al. Obesity‐related hypertension: pathogenesis, cardiovascular risk, and treatment—a position paper of the obesity society and the American society of hypertension. Obesity. 2013;21(1):8–24.
Eckel RH, Kahn SE, Ferrannini E, Goldfine AB, Nathan DM, Schwartz MW, et al. Obesity and type 2 diabetes: what can be unified and what needs to be individualized? J Clin Endocrinol Metab. 2011;96(6):1654–63.
Littleton SW. Impact of obesity on respiratory function. Respirology. 2012;17(1):43–9.
Nikolopoulou A, Kadoglou NP. Obesity and metabolic syndrome as related to cardiovascular disease. Expert Rev Cardiovasc Ther. 2012;10(7):933–9.
Fock KM, Khoo J. Diet and exercise in management of obesity and overweight. J Gastroenterol Hepatol. 2013;28 Suppl 4:59–63.
Davis C. From passive overeating to food addiction: a spectrum of compulsion and severity. ISRN Obesity. 2013;2013:20. This review describes the dimensional scale of compulsive overeating. It also considers the overlapping symptomology between compulsive overeating and addiction phenotypes, in both human and animal studies.
Vancampfort D, Vanderlinden J, De Hert M, Adamkova M, Skjaerven LH, Catalan-Matamoros D, et al. A systematic review on physical therapy interventions for patients with binge eating disorder. Disabil Rehabil. 2013;35(26):2191–6.
Brownley KA, Berkman ND, Sedway JA, Lohr KN, Bulik CM. Binge eating disorder treatment: a systematic review of randomized controlled trials. Int J Eat Disord. 2007;40(4):337–48.
Davis C, Curtis C, Levitan RD, Carter JC, Kaplan AS, Kennedy JL. Evidence that ‘food addiction’ is a valid phenotype of obesity. Appetite. 2011;57(3):711–7. This article to validates the Yale Food Addiction Scale (YFAS) in a sample of obese adults, providing further evidence of the association between YFAS scores and the ‘food addiction’ phenotype. Individuals presenting with ‘food addiction’ showed greater impulsivity, emotional reactivity and comorbidity with attention-deficit/ hyperactivity disorder, binge eating disorder and depression.
Ifland J, Preuss H, Marcus M, Rourke K, Taylor W, Burau K, et al. Refined food addiction: a classic substance use disorder. Med Hypotheses. 2009;72(5):518–26.
Davis C, Carter JC. Compulsive overeating as an addiction disorder. A review of theory and evidence. Appetite. 2009;53(1):1–8.
Volkow ND, Wang G-J, Fowler JS, Telang F. Overlapping neuronal circuits in addiction and obesity: evidence of systems pathology. Philos Trans Royal Soc London B: Biol Sci. 2008;363(1507):3191–200.
Berridge KC. Liking’ and ‘wanting’ food rewards: brain substrates and roles in eating disorders. Physiol Behav. 2009;97(5):537–50.
Davis C. Evolutionary and neuropsychological perspectives on addictive behaviors and addictive substances: relevance to the “food addiction” construct. Subst Abuse Rehab. 2014;5:129.
Bellisari A. Evolutionary origins of obesity. Obesity Rev: Off J Int Assoc Study Obesity. 2008;9(2):165–80.
Cummins S, Macintyre S. Food environments and obesity—neighbourhood or nation? Int J Epidemiol. 2006;35(1):100–4.
Morland KB, Evenson KR. Obesity prevalence and the local food environment. Health Place. 2009;15(2):491–5.
Rainer G. Behavioral flexibility and the frontal lobe. Neuron. 2007;53(3):321–3.
Uchibe E, Doya K. Finding intrinsic rewards by embodied evolution and constrained reinforcement learning. Neural Netw. 2008;21(10):1447–55.
Kalivas PW, Volkow ND. The neural basis of addiction: a pathology of motivation and choice. Am J Psych. 2014.
Volkow ND, Wang GJ, Tomasi D, Baler RD. Obesity and addiction: neurobiological overlaps. Obes Rev. 2013;14(1):2–18. This article reviews the similarities between compulsive overeating and substance use disorders, with a particular focus on evidence from neuroimaging in areas contributing to reward processing, incentive motivation, self-inhibition and other aspects of reward processing.
Baudonnat M, Huber A, David V, Walton ME. Heads for learning, tails for memory: reward, reinforcement and a role of dopamine in determining behavioral relevance across multiple timescales. Frontiers Neurosci. 2013;7.
Robinson TE, Berridge KC. Review. The incentive sensitization theory of addiction: some current issues. Philos Trans R Soc Lond Ser B Biol Sci. 2008;363(1507):3137–46.
Berridge KC, Robinson TE, Aldridge JW. Dissecting components of reward: ‘liking’, ‘wanting’, and learning. Curr Opin Pharmacol. 2009;9(1):65–73.
Berridge KC. Motivation concepts in behavioral neuroscience. Physiol Behav. 2004;81(2):179–209.
Volkow ND, Fowler JS, Wang G-J, Goldstein RZ. Role of dopamine, the frontal cortex and memory circuits in drug addiction: insight from imaging studies. Neurobiol Learn Mem. 2002;78(3):610–24.
Volkow ND, Wang G-J, Telang F, Fowler JS, Logan J, Childress A-R, et al. Cocaine cues and dopamine in dorsal striatum: mechanism of craving in cocaine addiction. J Neurosci. 2006;26(24):6583–8.
Kühn S, Gallinat J. Common biology of craving across legal and illegal drugs—a quantitative meta-analysis of cue-reactivity brain response. Eur J Neurosci. 2011;33(7):1318–26.
Gearhardt AN, Yokum S, Orr PT, Stice E, Corbin WR, Brownell KD. The neural correlates of “food addiction. Arch Gen Psychiatry. 2011;68(8):808–16. This fMRI investigation provides further evidence for the similarities in neural networks implicated in substance use disorders and ‘food addiction’. Researchers showed that individuals with higher food addiction scores showed greater activation of the anterior cingulate cortex (ACC), medial orbitofrontal cortex (OFC), and amygdala in response to food reward anticipation. Interestingly, these individuals also showed less activation of the lateral OFC after receiving a food reward.
Meule A, Lutz A, Vögele C, Kübler A. Women with elevated food addiction symptoms show accelerated reactions, but no impaired inhibitory control, in response to pictures of high-calorie food-cues. Eat Behav. 2012;13(4):423–8.
Wise RA, Koob GF. The development and maintenance of drug addiction. Neuropsychopharmacology. 2014;39(2):254–62.
Volkow ND, Wang GJ, Fowler JS, Tomasi D, Telang F, Baler R. Addiction: decreased reward sensitivity and increased expectation sensitivity conspire to overwhelm the brain’s control circuit. Bioessays. 2010;32(9):748–55.
Gardner EL. Addiction and brain reward and antireward pathways. 2011.
Stice E, Spoor S, Ng J, Zald DH. Relation of obesity to consummatory and anticipatory food reward. Physiol Behav. 2009;97(5):551–60.
Burger KS, Stice E. Variability in reward responsivity and obesity: evidence from brain imaging studies. Current Drug Abuse Rev. 2011;4(3):182.
Parylak SL, Koob GF, Zorrilla EP. The dark side of food addiction. Physiol Behav. 2011;104(1):149–56.
Bromberg-Martin ES, Matsumoto M, Hikosaka O. Dopamine in motivational control: rewarding, aversive, and alerting. Neuron. 2010;68(5):815–34.
Lammel S, Ion Daniela I, Roeper J, Malenka RC. Projection-specific modulation of dopamine neuron synapses by aversive and rewarding stimuli. Neuron. 2011;70(5):855–62.
Volkow ND, Wang G-J, Tomasi D, Baler RD. The addictive dimensionality of obesity. Biol Psychiatry. 2013;73(9):811–8.
Baik J-H. Dopamine signaling in reward-related behaviors. Frontiers Neural Circ. 2013;7.
Beaulieu J-M, Gainetdinov RR. The physiology, signaling, and pharmacology of dopamine receptors. Pharmacol Rev. 2011;63(1):182–217.
Dichter GS, Damiano CA, Allen JA. Reward circuitry dysfunction in psychiatric and neurodevelopmental disorders and genetic syndromes: animal models and clinical findings. J Neurodev Disord. 2012;4(1):19.
Hurley SW, Johnson AK. The role of the lateral hypothalamus and orexin in ingestive behavior: a model for the translation of past experience and sensed deficits into motivated behaviors. Front Syst Neurosci. 2014;8:216.
Havel PJ. Peripheral signals conveying metabolic information to the brain: short-term and long-term regulation of food intake and energy homeostasis. Exp Biol Med. 2001;226(11):963–77.
Woods SC. Gastrointestinal satiety signals I. An overview of gastrointestinal signals that influence food intake. Am J Physiol-Gastrointestinal Liver Physiol. 2004;286(1):G7–G13.
Roth JD, Roland BL, Cole RL, Trevaskis JL, Weyer C, Koda JE, et al. Leptin responsiveness restored by amylin agonism in diet-induced obesity: evidence from nonclinical and clinical studies. Proc Natl Acad Sci. 2008;105(20):7257–62.
Wielinga PY, Löwenstein C, Muff S, Munz M, Woods SC, Lutz TA. Central amylin acts as an adiposity signal to control body weight and energy expenditure. Physiol Behav. 2010;101(1):45–52.
Woods SC, Seeley RJ. Adiposity signals and the control of energy homeostasis. Nutrition. 2000;16(10):894–902.
Geary N. Endocrine controls of eating: CCK, leptin, and ghrelin. Physiol Behav. 2004;81(5):719–33.
Schwartz MW, Woods SC, Seeley RJ, Barsh GS, Baskin DG, Leibel RL. Is the energy homeostasis system inherently biased toward weight gain? Diabetes. 2003;52(2):232–8.
Zigman JM, Elmquist JK. Minireview: from anorexia to obesity—the yin and yang of body weight control. Endocrinology. 2003;144(9):3749–56.
Opland DM, Leinninger GM, Myers Jr MG. Modulation of the mesolimbic dopamine system by leptin. Brain Res. 2010;1350:65–70.
Leinninger GM, Opland DM, Jo YH, Faouzi M, Christensen L, Cappellucci LA, et al. Leptin action via neurotensin neurons controls orexin, the mesolimbic dopamine system and energy balance. Cell Metab. 2011;14(3):313–23.
Mebel DM, Wong JC, Dong YJ, Borgland SL. Insulin in the ventral tegmental area reduces hedonic feeding and suppresses dopamine concentration via increased reuptake. Eur J Neurosci. 2012;36(3):2336–46.
Egecioglu E, Skibicka KP, Hansson C, Alvarez-Crespo M, Friberg PA, Jerlhag E, et al. Hedonic and incentive signals for body weight control. Rev Endocr Metab Disord. 2011;12(3):141–51.
Cone JJ, McCutcheon JE, Roitman MF. Ghrelin acts as an interface between physiological state and phasic dopamine signaling. J Neurosci: Off J Soc Neurosci. 2014;34(14):4905–13.
Volkow ND, Wang GJ, Baler RD. Reward, dopamine and the control of food intake: implications for obesity. Trends Cogn Sci. 2011;15(1):37–46.
Heber D, Carpenter CL. Addictive genes and the relationship to obesity and inflammation. Mol Neurobiol. 2011;44(2):160–5.
Sturgess JE, George TP, Kennedy JL, Heinz A, Muller DJ. Pharmacogenetics of alcohol, nicotine and drug addiction treatments. Addict Biol. 2011;16(3):357–76.
Nutt DJ, Lingford-Hughes A, Erritzoe D, Stokes PR. The dopamine theory of addiction: 40 years of highs and lows. Nat Rev Neurosci. 2015;16(5):305–12.
Michaelides M, Thanos PK, Volkow ND, Wang GJ. Dopamine-related frontostriatal abnormalities in obesity and binge-eating disorder: emerging evidence for developmental psychopathology. Int Rev Psychiatry (Abingdon, England). 2012;24(3):211–8.
Thompson J, Thomas N, Singleton A, Piggot M, Lloyd S, Perry E, et al. D2 dopamine receptor gene (DRD2) Taql A polymorphism: reduced dopamine D2 receptor binding in the human striatum associated with the A1 allele. Pharmacogenet Genomics. 1997;7(6):479–84.
Peciña M, Mickey BJ, Love T, Wang H, Langenecker SA, Hodgkinson C, et al. DRD2 polymorphisms modulate reward and emotion processing, dopamine neurotransmission and openness to experience. Cortex. 2013;49(3):877–90.
Noble EP. Addiction and its reward process through polymorphisms of the D2 dopamine receptor gene: a review. Eur Psychiatry. 2000;15(2):79–89.
Chen AL, Blum K, Chen TJ, Giordano J, Downs BW, Han D, et al. Correlation of the Taq 1 dopamine D2 receptor gene and percent body fat in obese and screened control subjects: a preliminary report. Food Func. 2012;3(1):40–8.
Davis C, Levitan RD, Kaplan AS, Carter J, Reid C, Curtis C, et al. Reward sensitivity and the D2 dopamine receptor gene: a case–control study of binge eating disorder. Prog Neuro-Psychopharmacol Biol Psychiatry. 2008;32(3):620–8.
Epstein LH, Temple JL, Neaderhiser BJ, Salis RJ, Erbe RW, Leddy JJ. Food reinforcement, the dopamine D(2) receptor genotype, and energy intake in obese and nonobese humans. Behav Neurosci. 2007;121(5):877–86.
Lett TA, Wallace TJ, Chowdhury NI, Tiwari AK, Kennedy JL, Muller DJ. Pharmacogenetics of antipsychotic-induced weight gain: review and clinical implications. Mol Psychiatry. 2012;17(3):242–66.
Kao AC, Müller DJ. Genetics of antipsychotic-induced weight gain: update and current perspectives. Pharmacogenomics. 2013;14(16):2067–83.
Fuke S, Suo S, Takahashi N, Koike H, Sasagawa N, Ishiura S. The VNTR polymorphism of the human dopamine transporter (DAT1) gene affects gene expression. Pharmacogenomics J. 2001;1(2):152–6.
van Dyck CH, Malison RT, Jacobsen LK, Seibyl JP, Staley JK, Laruelle M, et al. Increased dopamine transporter availability associated with the 9-repeat allele of the SLC6A3 gene. J Nucl Med. 2005;46(5):745–51.
van de Giessen EM, de Win MM, Tanck MW, van den Brink W, Baas F, Booij J. Striatal dopamine transporter availability associated with polymorphisms in the dopamine transporter gene SLC6A3. J Nucl Med. 2009;50(1):45–52.
Shumay E, Wang G-J, Volkow N, Telang F, Jayne M, Wong C, et al. Exploring the links between the brain dopamine transporter availability, DAT1 genotype and body mass index. J Nucl Med Meeting Abst. 2012;53(1_MeetingAbstracts):195.
Davis C, Levitan RD, Kaplan AS, Carter J, Reid C, Curtis C, et al. Dopamine transporter gene (DAT1) associated with appetite suppression to methylphenidate in a case–control study of binge eating disorder. Neuropsychopharmacology. 2007;32(10):2199–206.
Nathan PJ, Bullmore ET. From taste hedonics to motivational drive: central μ-opioid receptors and binge-eating behaviour. 7. 2009.
Smith DG, Robbins TW. The neurobiological underpinnings of obesity and binge eating: a rationale for adopting the food addiction model. Biol Psychiatry. 2013;73(9):804–10.
Haerian BS, Haerian MS. OPRM1 rs1799971 polymorphism and opioid dependence: evidence from a meta-analysis. Pharmacogenomics. 2013;14(7):813–24.
Davis C, Zai C, Levitan RD, Kaplan AS, Carter JC, Reid-Westoby C, et al. Opiates, overeating and obesity: a psychogenetic analysis. Int J Obesity (2005). 2011;35(10):1347–54.
Bach P, Vollsta Dt-Klein S, Kirsch M, Hoffmann S, Jorde A, Frank J et al. Increased mesolimbic cue-reactivity in carriers of the mu-opioid-receptor gene OPRM1 A118G polymorphism predicts drinking outcome: a functional imaging study in alcohol dependent subjects. European neuropsychopharmacology : the journal of the European College of Neuropsychopharmacology. 2015.
Haghighi A, Melka MG, Bernard M, Abrahamowicz M, Leonard GT, Richer L, et al. Opioid receptor mu 1 gene, fat intake and obesity in adolescence. Mol Psychiatry. 2014;19(1):63–8.
Clarke TK, Crist RC, Kampman KM, Dackis CA, Pettinati HM, O’Brien CP, et al. Low frequency genetic variants in the mu-opioid receptor (OPRM1) affect risk for addiction to heroin and cocaine. Neurosci Lett. 2013;542:71–5.
Carpenter CL, Wong AM, Li Z, Noble EP, Heber D. Association of dopamine D2 receptor and leptin receptor genes with clinically severe obesity. Obesity. 2013;21(9):E467–E73.
Hardman CA, Rogers PJ, Timpson NJ, Munafo MR. Lack of association between DRD2 and OPRM1 genotypes and adiposity. Int J Obes. 2014;38(5):730–6.
Zhang Y, Picetti R, Butelman ER, Ho A, Blendy JA, Kreek MJ. Mouse model of the OPRM1 (A118G) polymorphism: differential heroin self-administration behavior compared with wild-type mice. Neuropsychopharmacology. 2015;40(5):1091–100.
Nogueiras R, Seeley RJ. Our evolving understanding of the interaction between leptin and dopamine system to regulate ingestive behaviors. Mol Metab. 2012;1(1–2):8–9.
Kern A, Albarran-Zeckler R, Walsh HE, Smith RG. Apo-ghrelin receptor forms heteromers with DRD2 in hypothalamic neurons and is essential for anorexigenic effects of DRD2 agonism. Neuron. 2012;73(2):317–32.
Davis JF, Choi DL, Schurdak JD, Fitzgerald MF, Clegg DJ, Lipton JW, et al. Leptin regulates energy balance and motivation through action at distinct neural circuits. Biol Psychiatry. 2011;69(7):668–74.
al’Absi M, Hooker S, Fujiwara K, Kiefer F, von der Goltz C, Cragin T, et al. Circulating leptin levels are associated with increased craving to smoke in abstinent smokers. Pharmacol Biochem Behav. 2011;97(3):509–13.
Morrison CD. Leptin signaling in brain: a link between nutrition and cognition? Biochim Biophys Acta (BBA) - Mol Basis Dis. 2009;1792(5):401–8.
Davis JF. Adipostatic regulation of motivation and emotion. Discov Med. 2010;9(48):462–7.
van Rossum CTM, Hoebee B, van Baak MA, Mars M, Saris WHM, Seidell JC. Genetic variation in the leptin receptor gene, leptin, and weight gain in young Dutch adults. Obes Res. 2003;11(3):377–86.
Voisey J, Carroll L, van Daal A. Melanocortins and their receptors and antagonists. Curr Drug Targets. 2003;4(7):586–97.
Cui H, Mason BL, Lee C, Nishi A, Elmquist JK, Lutter M. Melanocortin 4 receptor signaling in dopamine 1 receptor neurons is required for procedural memory learning. Physiol Behav. 2012;106(2):201–10.
Hsu R, Taylor JR, Newton SS, Alvaro JD, Haile C, Han G, et al. Blockade of melanocortin transmission inhibits cocaine reward. Eur J Neurosci. 2005;21(8):2233–42.
Shelkar GP, Kale AD, Singh U, Singru PS, Subhedar NK, Kokare DM. Alpha-melanocyte stimulating hormone modulates ethanol self-administration in posterior ventral tegmental area through melanocortin-4 receptors. Addict Biol. 2015;20(2):302–15.
Thorleifsson G, Walters GB, Gudbjartsson DF, Steinthorsdottir V, Sulem P, Helgadottir A, et al. Genome-wide association yields new sequence variants at seven loci that associate with measures of obesity. Nat Genet. 2009;41(1):18–24.
Xi B, Chandak GR, Shen Y, Wang Q, Zhou D. Association between common polymorphism near the MC4R gene and obesity risk: a systematic review and meta-analysis. PLoS One. 2012;7(9), e45731.
Yilmaz Z, Davis C, Loxton NJ, Kaplan AS, Levitan RD, Carter JC, et al. Association between MC4R rs17782313 polymorphism and overeating behaviors. Int J Obesity (2005). 2015;39(1):114–20.
Porfirio MC, Giovinazzo S, Cortese S, Giana G, Lo-Castro A, Mouren MC, et al. Role of ADHD symptoms as a contributing factor to obesity in patients with MC4R mutations. Med Hypotheses. 2015;84(1):4–7.
Zheng H, Lenard N, Shin A, Berthoud H-R. Appetite control and energy balance regulation in the modern world: reward-driven brain overrides repletion signals. Int J Obes. 2009;33:S8–S13.
Association AP. Diagnostic and statistical manual of mental disorders: DSM-5. ManMag; 2003.
Cassin SE, von Ranson KM. Is binge eating experienced as an addiction? Appetite. 2007;49(3):687–90.
Gearhardt AN, Corbin WR, Brownell KD. Preliminary validation of the Yale food addiction scale. Appetite. 2009;52(2):430–6. This article reports the first validation of the Yale Food Addiction Scale (YFAS), developed to assess a ‘food addiction’ phenotype. In a sample of young adults, the YFAS predicted binge-eating behavior better than other psychometric tools.
Association AP, Association AP. Diagnostic and statistical manual-text revision (DSM-IV-TRim, 2000). Am Psych Assoc; 2000.
Brunault P, Ballon N, Gaillard P, Réveillère C, Courtois R. Validation of the french version of the Yale food addiction scale: an examination of its factor structure, reliability, and construct validity in a nonclinical sample. Can J Psychiatry. 2014;59(5):276–84.
Chen G, Tang Z, Guo G, Liu X, Xiao S. The Chinese version of the Yale food addiction scale: an examination of its validation in a sample of female adolescents. Eat Behav. 2015;18:97–102.
Clark SM, Saules KK. Validation of the Yale food addiction scale among a weight-loss surgery population. Eat Behav. 2013;14(2):216–9.
Swendsen J, Conway KP, Degenhardt L, Glantz M, Jin R, Merikangas KR, et al. Mental disorders as risk factors for substance use, abuse and dependence: results from the 10‐year follow‐up of the national comorbidity survey. Addiction. 2010;105(6):1117–28.
Eichen DM, Lent MR, Goldbacher E, Foster GD. Exploration of “food addiction” in overweight and obese treatment-seeking adults. Appetite. 2013;67:22–4.
Gearhardt AN, Roberto CA, Seamans MJ, Corbin WR, Brownell KD. Preliminary validation of the Yale food addiction scale for children. Eat Behav. 2013;14(4):508–12.
Meule A, Hermann T, Kubler A. Food addiction in overweight and obese adolescents seeking weight-loss treatment. Eur Eating Disord Rev: J Eating Disord Assoc. 2015;23(3):193–8.
Burrows T, Meule A. Food addiction’. What happens in childhood? Appetite. 2015;89:298–300.
Meule A. Food addiction and body-mass-index: a non-linear relationship. Med Hypotheses. 2012;79(4):508–11.
Davis C, Loxton NJ. A psycho-genetic study of hedonic responsiveness in relation to “food addiction. Nutrients. 2014;6(10):4338–53.
Meule A, Gearhardt AN. Food addiction in the light of DSM-5. Nutrients. 2014;6(9):3653–71. This article provides a detailed comparison between currently proposed dimensions of ‘food addiction’ and new criteria for substance use disorders (SUDs) diagnoses according to the DSM-5.
Meule A. How prevalent is “Food Addiction”? Frontiers Psych. 2011;2.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Nina Carlier, Victoria S. Marshe, Jana Cmorejova, Caroline Davis, and Daniel J. Müller declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Genetic Disorders
Nina Carlier and Victoria S. Marshe contributed equally to this work.
Rights and permissions
About this article
Cite this article
Carlier, N., Marshe, V.S., Cmorejova, J. et al. Genetic Similarities between Compulsive Overeating and Addiction Phenotypes: A Case for “Food Addiction”?. Curr Psychiatry Rep 17, 96 (2015). https://doi.org/10.1007/s11920-015-0634-5
Published:
DOI: https://doi.org/10.1007/s11920-015-0634-5