Abstract
Purpose of Review
To describe the effects of type 1 diabetes on bone cells.
Recent findings
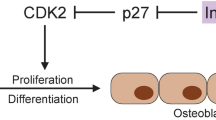
Type 1 diabetes (T1D) is associated with low bone mineral density, increased risk of fractures, and poor fracture healing. Its effects on the skeleton were primarily attributed to impaired bone formation, but recent data suggests that bone remodeling and resorption are also compromised. The hyperglycemic and inflammatory environment associated with T1D impacts osteoblasts, osteocytes, and osteoclasts. The mechanisms involved are complex; insulinopenia, pro-inflammatory cytokine production, and alterations in gene expression are a few of the contributing factors leading to poor osteoblast activity and survival and, therefore, poor bone formation. In addition, the observed sclerostin level increase accompanied by decreased osteocyte number and enhanced osteoclast activity in T1D results in uncoupling of bone remodeling.
Summary
T1D negatively impacts osteoblasts and osteocytes, whereas its effects on osteoclasts are not well characterized, although the limited studies available indicate increased osteoclast activity, favoring bone resorption.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Masse PG, Pacifique MB, Tranchant CC, Arjmandi BH, Ericson KL, Donovan SM, et al. Bone metabolic abnormalities associated with well-controlled type 1 diabetes (IDDM) in young adult women: a disease complication often ignored or neglected. J Am Coll Nutr. 2010;29(4):419–29.
Loureiro MB, Ururahy MA, Freire-Neto FP, Oliveira GH, Duarte VM, Luchessi AD, et al. Low bone mineral density is associated to poor glycemic control and increased OPG expression in children and adolescents with type 1 diabetes. Diabetes Res Clin Pract. 2014;103(3):452–7. doi:10.1016/j.diabres.2013.12.018.
Khan TS, Fraser LA. Type 1 diabetes and osteoporosis: from molecular pathways to bone phenotype. 2015;2015:174186. doi:10.1155/2015/174186.
Lu H, Kraut D, Gerstenfeld LC, Graves DT. Diabetes interferes with the bone formation by affecting the expression of transcription factors that regulate osteoblast differentiation. Endocrinology. 2003;144(1):346–52. doi:10.1210/en.2002-220072.
Fowlkes JL, Bunn RC, Liu L, Wahl EC, Coleman HN, Cockrell GE, et al. Runt-related transcription factor 2 (RUNX2) and RUNX2-related osteogenic genes are down-regulated throughout osteogenesis in type 1 diabetes mellitus. Endocrinology. 2008;149(4):1697–704. doi:10.1210/en.2007-1408.
Komori T. Regulation of osteoblast differentiation by transcription factors. J Cell Biochem. 2006;99(5):1233–9. doi:10.1002/jcb.20958.
Wu H, Whitfield TW, Gordon JA, Dobson JR, Tai PW, van Wijnen AJ, et al. Genomic occupancy of Runx2 with global expression profiling identifies a novel dimension to control of osteoblastogenesis. Genome Biol. 2014;15(3):R52. doi:10.1186/gb-2014-15-3-r52.
Botolin S, Faugere MC, Malluche H, Orth M, Meyer R, McCabe LR. Increased bone adiposity and peroxisomal proliferator-activated receptor-gamma2 expression in type I diabetic mice. Endocrinology. 2005;146(8):3622–31. doi:10.1210/en.2004-1677.
Botolin S, McCabe LR. Bone loss and increased bone adiposity in spontaneous and pharmacologically induced diabetic mice. Endocrinology. 2007;148(1):198–205. doi:10.1210/en.2006-1006. This study demonstrated the beneficial effects of zinc supplementation on bone morphology and strength as well as on bone formation parameters.
Hie M, Iitsuka N, Otsuka T, Tsukamoto I. Insulin-dependent diabetes mellitus decreases osteoblastogenesis associated with the inhibition of Wnt signaling through increased expression of Sost and Dkk1 and inhibition of Akt activation. Int J Mol Med. 2011;28(3):455–62. doi:10.3892/ijmm.2011.697.
Bortolin RH, da Graca Azevedo Abreu BJ, Abbott Galvao Ururahy M, de Souza KS C, Bezerra JF, Loureiro MB, et al. Protection against T1DM-induced bone loss by zinc supplementation: biomechanical, histomorphometric, and molecular analyses in STZ-induced diabetic rats. PloS one. 2015;10(5):e0125349. doi:10.1371/journal.pone.0125349.
Iitsuka N, Hie M, Tsukamoto I. Zinc supplementation inhibits the increase in osteoclastogenesis and decrease in osteoblastogenesis in streptozotocin-induced diabetic rats. Eur J Pharmacol. 2013;714(1–3):41–7. doi:10.1016/j.ejphar.2013.05.020.
Botolin S, McCabe LR. Inhibition of PPARgamma prevents type I diabetic bone marrow adiposity but not bone loss. J Cell Physiol. 2006;209(3):967–76. doi:10.1002/jcp.20804.
Palta M, LeCaire TJ, Sadek-Badawi M, Herrera VM, Danielson KK. The trajectory of IGF-1 across age and duration of type 1 diabetes. Diabet/Metab Res Rev. 2014;30(8):777–83. doi:10.1002/dmrr.2554. This longitudinal study followed IGF-1 levels in patients with Type 1 diabetes and confirmed lower IGF-1 levels compared to normal individuals with a delayed peak of IGF-1 in adolecent females with Type 1 diabetes and highlighted the effect of glycemic control during adolecense on IGF-1 levels.
Zhao YF, Zeng DL, Xia LG, Zhang SM, Xu LY, Jiang XQ, et al. Osteogenic potential of bone marrow stromal cells derived from streptozotocin-induced diabetic rats. Int J Mol Med. 2013;31(3):614–20. doi:10.3892/ijmm.2013.1227.
Xian L, Wu X, Pang L, Lou M, Rosen CJ, Qiu T, et al. Matrix IGF-1 maintains bone mass by activation of mTOR in mesenchymal stem cells. Nat Med. 2012;18(7):1095–101. doi:10.1038/nm.2793.
Crane JL, Zhao L, Frye JS, Xian L, Qiu T, Cao X. IGF-1 Signaling is Essential for Differentiation of Mesenchymal Stem Cells for Peak Bone Mass. Bone Res. 2013;1(2):186–94. doi:10.4248/BR201302007.
Bouillon R. Diabetic bone disease. Low turnover osteoporosis related to decreased IGF-I production. Verh K Acad Geneeskd Belg. 1992;54(4):365–91. discussion 91–2.
Zhang M, Xuan S, Bouxsein ML, von Stechow D, Akeno N, Faugere MC, et al. Osteoblast-specific knockout of the insulin-like growth factor (IGF) receptor gene reveals an essential role of IGF signaling in bone matrix mineralization. J Biol Chem. 2002;277(46):44005–12. doi:10.1074/jbc.M208265200.
Centrella M, McCarthy TL, Canalis E. Receptors for insulin-like growth factors-I and -II in osteoblast-enriched cultures from fetal rat bone. Endocrinology. 1990;126(1):39–44. doi:10.1210/endo-126-1-39.
Pun KK, Lau P, Ho PW. The characterization, regulation, and function of insulin receptors on osteoblast-like clonal osteosarcoma cell line. J Bone Min Res. 1989;4(6):853–62. doi:10.1002/jbmr.5650040610.
Kream BE, Smith MD, Canalis E, Raisz LG. Characterization of the effect of insulin on collagen synthesis in fetal rat bone. Endocrinology. 1985;116(1):296–302. doi:10.1210/endo-116-1-296.
Fulzele K, Riddle RC, DiGirolamo DJ, Cao X, Wan C, Chen D, et al. Insulin receptor signaling in osteoblasts regulates postnatal bone acquisition and body composition. Cell. 2010;142(2):309–19. doi:10.1016/j.cell.2010.06.002.
Thrailkill K, Bunn RC, Lumpkin C, Jr., Wahl E. Loss of insulin receptor in osteoprogenitor cells impairs structural strength of bone. 2014;2014:703589. doi:10.1155/2014/703589
Peng J, Hui K, Hao C, Peng Z, Gao QX, Jin Q et al. Low bone turnover and reduced angiogenesis in streptozotocin-induced osteoporotic mice. Connective tissue research. 2016:1–13. doi:10.3109/03008207.2016.1171858.
Hamada Y, Kitazawa S, Kitazawa R, Fujii H, Kasuga M, Fukagawa M. Histomorphometric analysis of diabetic osteopenia in streptozotocin-induced diabetic mice: a possible role of oxidative stress. Bone. 2007;40(5):1408–14. doi:10.1016/j.bone.2006.12.057.
Weinberg E, Maymon T, Moses O, Weinreb M. Streptozotocin-induced diabetes in rats diminishes the size of the osteoprogenitor pool in bone marrow. Diabetes Res Clin Pract. 2014;103(1):35–41. doi:10.1016/j.diabres.2013.11.015. This study examined the effect of oxidative stress in the function and survival of osteoprogenitor cells of an STZ-induced diabetes model.
Hamed EA, Faddan NH, Elhafeez HA, Sayed D. Parathormone--25(OH)-vitamin D axis and bone status in children and adolescents with type 1 diabetes mellitus. Pediatr Diabetes. 2011;12(6):536–46. doi:10.1111/j.1399-5448.2010.00739.x.
Motyl KJ, McCauley LK, McCabe LR. Amelioration of type I diabetes-induced osteoporosis by parathyroid hormone is associated with improved osteoblast survival. J Cell Physiol. 2012;227(4):1326–34. doi:10.1002/jcp.22844.
Verhaeghe J, Van Herck E, van Bree R, Moermans K, Bouillon R. Decreased osteoblast activity in spontaneously diabetic rats. In vivo studies on the pathogenesis. Endocrine. 1997;7(2):165–75. doi:10.1007/bf02778138.
Horcajada-Molteni MN, Chanteranne B, Lebecque P, Davicco MJ, Coxam V, Young A, et al. Amylin and bone metabolism in streptozotocin-induced diabetic rats. J Bone Min Res. 2001;16(5):958–65. doi:10.1359/jbmr.2001.16.5.958.
Bouillon R, Bex M, Van Herck E, Laureys J, Dooms L, Lesaffre E, et al. Influence of age, sex, and insulin on osteoblast function: osteoblast dysfunction in diabetes mellitus. J Clin Endocrinol Metab. 1995;80(4):1194–202. doi:10.1210/jcem.80.4.7714089.
Lumachi F, Camozzi V, Tombolan V, Luisetto G. Bone mineral density, osteocalcin, and bone-specific alkaline phosphatase in patients with insulin-dependent diabetes mellitus. Ann N Y Acad Sci. 2009;1173 Suppl 1:E64–7. doi:10.1111/j.1749-6632.2009.04955.x.
Maddaloni E, D’Onofrio L, Lauria A, et al. Osteocalcin levels are inversely associated with Hba1c and BMI in adult subjects with long-standing type 1 diabetes. J Diabetes Res. 2014;37(7):661–6. doi:10.1155/2014/703589.
Starup-Linde J. Diabetes, biochemical markers of bone turnover, diabetes control, and bone. Front Endocrinol. 2013;4:21. doi:10.3389/fendo.2013.00021.
Brenner RE, Riemenschneider B, Blum W, Morike M, Teller WM, Pirsig W, et al. Defective stimulation of proliferation and collagen biosynthesis of human bone cells by serum from diabetic patients. Acta Endocrinol. 1992;127(6):509–14.
Cunha JS, Ferreira VM, Maquigussa E, Naves MA, Boim MA. Effects of high glucose and high insulin concentrations on osteoblast function in vitro. Cell Tissue Res. 2014;358(1):249–56. doi:10.1007/s00441-014-1913-x.
Zayzafoon M, Stell C, Irwin R, McCabe LR. Extracellular glucose influences osteoblast differentiation and c-Jun expression. J Cell Biochem. 2000;79(2):301–10.
Botolin S, McCabe LR. Chronic hyperglycemia modulates osteoblast gene expression through osmotic and non-osmotic pathways. J Cell Biochem. 2006;99(2):411–24. doi:10.1002/jcb.20842.
Santana RB, Xu L, Chase HB, Amar S, Graves DT, Trackman PC. A role for advanced glycation end products in diminished bone healing in type 1 diabetes. Diabetes. 2003;52(6):1502–10.
Ogawa N, Yamaguchi T, Yano S, Yamauchi M, Yamamoto M, Sugimoto T. The combination of high glucose and advanced glycation end-products (AGEs) inhibits the mineralization of osteoblastic MC3T3-E1 cells through glucose-induced increase in the receptor for AGEs. Horm Metab Res. 2007;39(12):871–5. doi:10.1055/s-2007-991157.
Weinberg E, Maymon T, Weinreb M. AGEs induce caspase-mediated apoptosis of rat BMSCs via TNFalpha production and oxidative stress. J Mol Endocrinol. 2014;52(1):67–76. doi:10.1530/JME-13-0229.
Rachon D, Mysliwska J, Suchecka-Rachon K, Semetkowska-Jurkiewicz B, Zorena K, Lysiak-Szydlowska W. Serum interleukin-6 levels and bone mineral density at the femoral neck in post-menopausal women with Type 1 diabetes. Diabet Med. 2003;20(6):475–80.
Jin Y, Sharma A, Carey C, Hopkins D, Wang X, Robertson DG, et al. The expression of inflammatory genes is upregulated in peripheral blood of patients with type 1 diabetes. Diabetes Care. 2013;36(9):2794–802. doi:10.2337/dc12-1986.
AboElAsrar MA, Elbarbary NS, Elshennawy DE, Omar AM. Insulin-like growth factor-1 cytokines cross-talk in type 1 diabetes mellitus: relationship to microvascular complications and bone mineral density. Cytokine. 2012;59(1):86–93. doi:10.1016/j.cyto.2012.03.019.
Motyl KJ, Botolin S, Irwin R, Appledorn DM, Kadakia T, Amalfitano A, et al. Bone inflammation and altered gene expression with type I diabetes early onset. J Cell Physiol. 2009;218(3):575–83. doi:10.1002/jcp.21626.
Perrien DS, Liu Z, Wahl EC, Bunn RC, Skinner RA, Aronson J, et al. Chronic ethanol exposure is associated with a local increase in TNF-alpha and decreased proliferation in the rat distraction gap. Cytokine. 2003;23(6):179–89.
Perrien DS, Brown EC, Fletcher TW, Irby DJ, Aronson J, Gao GG, et al. Interleukin-1 and tumor necrosis factor antagonists attenuate ethanol-induced inhibition of bone formation in a rat model of distraction osteogenesis. J Pharmacol Exp Ther. 2002;303(3):904–8. doi:10.1124/jpet.102.039636.
Gilbert LC, Chen H, Lu X, Nanes MS. Chronic low dose tumor necrosis factor-alpha (TNF) suppresses early bone accrual in young mice by inhibiting osteoblasts without affecting osteoclasts. Bone. 2013;56(1):174–83. doi:10.1016/j.bone.2013.06.002.
Gilbert L, He X, Farmer P, Boden S, Kozlowski M, Rubin J, et al. Inhibition of osteoblast differentiation by tumor necrosis factor-alpha. Endocrinology. 2000;141(11):3956–64. doi:10.1210/endo.141.11.7739.
Kayal RA, Siqueira M, Alblowi J, McLean J, Krothapalli N, Faibish D, et al. TNF-alpha mediates diabetes-enhanced chondrocyte apoptosis during fracture healing and stimulates chondrocyte apoptosis through FOXO1. J Bone Min Res. 2010;25(7):1604–15. doi:10.1002/jbmr.59.
Coe LM, Irwin R, Lippner D, McCabe LR. The bone marrow microenvironment contributes to type I diabetes induced osteoblast death. J Cell Physiol. 2011;226(2):477–83. doi:10.1002/jcp.22357.
Scheller EL, Cawthorn WP, Burr AA, Horowitz MC, MacDougald OA. Marrow adipose tissue: trimming the fat. Trends Endocrinol Metab TEM. 2016;27(6):392–403. doi:10.1016/j.tem.2016.03.016.
Liu LF, Shen WJ, Ueno M, Patel S, Kraemer FB. Characterization of age-related gene expression profiling in bone marrow and epididymal adipocytes. BMC Genomics. 2011;12:212. doi:10.1186/1471-2164-12-212.
Slade JM, Coe LM, Meyer RA, McCabe LR. Human bone marrow adiposity is linked with serum lipid levels not T1-diabetes. J Diabetes Complicat. 2012;26(1):1–9. doi:10.1016/j.jdiacomp.2011.11.001.
Clarke B. Normal bone anatomy and physiology. Clin J Am Soc Nephrol CJASN. 2008;3 Suppl 3:S131–9. doi:10.2215/cjn.04151206.
Robling AG, Bellido T, Turner CH. Mechanical stimulation in vivo reduces osteocyte expression of sclerostin. J Musculoskelet Neuronal Interac. 2006;6(4):354.
Bellido T, Ali AA, Gubrij I, Plotkin LI, Fu Q, O’Brien CA, et al. Chronic elevation of parathyroid hormone in mice reduces expression of sclerostin by osteocytes: a novel mechanism for hormonal control of osteoblastogenesis. Endocrinology. 2005;146(11):4577–83. doi:10.1210/en.2005-0239.
Ardawi MS, Al-Sibiany AM, Bakhsh TM, Rouzi AA, Qari MH. Decreased serum sclerostin levels in patients with primary hyperparathyroidism: a cross-sectional and a longitudinal study. Osteoporos Int. 2012;23(6):1789–97. doi:10.1007/s00198-011-1806-8.
Amrein K, Amrein S, Drexler C, Dimai HP, Dobnig H, Pfeifer K, et al. Sclerostin and its association with physical activity, age, gender, body composition, and bone mineral content in healthy adults. J Clin Endocrinol Metab. 2012;97(1):148–54. doi:10.1210/jc.2011-2152.
Honasoge M, Rao AD, Rao SD. Sclerostin: recent advances and clinical implications. Curr Opin Endocrinol Diabetes Obes. 2014;21(6):437–46. doi:10.1097/med.0000000000000114.
Spatz JM, Fields EE, Yu EW, Divieti Pajevic P, Bouxsein ML, Sibonga JD, et al. Serum sclerostin increases in healthy adult men during bed rest. J Clin Endocrinol Metab. 2012;97(9):E1736–40. doi:10.1210/jc.2012-1579.
Clarke BL, Drake MT. Clinical utility of serum sclerostin measurements. BoneKE y reports. 2013;2:361. doi:10.1038/bonekey.2013.95.
Mabilleau G, Chappard D, Basle MF. Cellular and molecular effects of thiazolidinediones on bone cells: a review. Int J Biochem Mol Biol. 2011;2(3):240–6.
Kim JH, Lee DE, Woo GH, Cha JH, Bak EJ, Yoo YJ. Osteocytic Sclerostin Expression in Alveolar Bone in Rats With Diabetes Mellitus and Ligature-Induced Periodontitis. J Periodontol. 2015;86(8):1005–11. doi:10.1902/jop.2015.150083.
Tanaka K, Yamaguchi T, Kanazawa I, Sugimoto T. Effects of high glucose and advanced glycation end products on the expressions of sclerostin and RANKL as well as apoptosis in osteocyte-like MLO-Y4-A2 cells. Biochem Biophys Res Commun. 2015;461(2):193–9. doi:10.1016/j.bbrc.2015.02.091.
Kim JY, Lee SK, Jo KJ, Song DY, Lim DM, Park KY, et al. Exendin-4 increases bone mineral density in type 2 diabetic OLETF rats potentially through the down-regulation of SOST/sclerostin in osteocytes. Life Sci. 2013;92(10):533–40. doi:10.1016/j.lfs.2013.01.001.
Yee CS, Xie L, Hatsell S, Hum N, Murugesh D, Economides AN, et al. Sclerostin antibody treatment improves fracture outcomes in a Type I diabetic mouse model. Bone. 2016;82:122–34. doi:10.1016/j.bone.2015.04.048. This study demonstrated that treatment of diabetic mice with anabolic doses of sclerostin antibody improves fracture healing, enhances bone mineral content of the fracture callus and alleviates the impaired osteoblastogenesis characteristic of diabetic bone.
Clarke BL. Anti-sclerostin antibodies: utility in treatment of osteoporosis. Maturitas. 2014;78(3):199–204. doi:10.1016/j.maturitas.2014.04.016.
Neumann T, Hofbauer LC, Rauner M, Lodes S, Kastner B, Franke S, et al. Clinical and endocrine correlates of circulating sclerostin levels in patients with type 1 diabetes mellitus. Clin Endocrinol. 2014;80(5):649–55. doi:10.1111/cen.12364. This study demonstrates the age-related increase in serum sclerostin levels in adults with long-standing T1D, relative to healthy non-diabetic subjects.
Catalano A, Pintaudi B, Morabito N, Di Vieste G, Giunta L, Bruno ML, et al. Gender differences in sclerostin and clinical characteristics in type 1 diabetes mellitus. Euro J Endocrinol Eur Fed Endocrine Soc. 2014;171(3):293–300. doi:10.1530/eje-14-0106.
Gennari L, Merlotti D, Valenti R, Ceccarelli E, Ruvio M, Pietrini MG, et al. Circulating sclerostin levels and bone turnover in type 1 and type 2 diabetes. J Clin Endocrinol Metab. 2012;97(5):1737–44. doi:10.1210/jc.2011-2958.
Tsentidis C, Gourgiotis D, Kossiva L, Marmarinos A, Doulgeraki A, Karavanaki K. Sclerostin distribution in children and adolescents with type 1 diabetes mellitus and correlation with bone metabolism and bone mineral density. Pediatr Diabetes. 2016;17(4):289–99. doi:10.1111/pedi.12288.
Zhou YJ, Li A, Song YL, Zhou H, Li Y, Tang YS. Role of sclerostin in the bone loss of postmenopausal chinese women with type 2 diabetes. Chin Med Sci J. 2013;28(3):135–9.
Gaudio A, Privitera F, Battaglia K, Torrisi V, Sidoti MH, Pulvirenti I, et al. Sclerostin levels associated with inhibition of the Wnt/beta-catenin signaling and reduced bone turnover in type 2 diabetes mellitus. J Clin Endocrinol Metab. 2012;97(10):3744–50. doi:10.1210/jc.2012-1901.
Garcia-Martin A, Rozas-Moreno P, Reyes-Garcia R, Morales-Santana S, Garcia-Fontana B, Garcia-Salcedo JA, et al. Circulating levels of sclerostin are increased in patients with type 2 diabetes mellitus. J Clin Endocrinol Metab. 2012;97(1):234–41. doi:10.1210/jc.2011-2186.
Daniele G, Winnier D, Mari A, Bruder J, Fourcaudot M, Pengou Z, et al. Sclerostin and insulin resistance in prediabetes: evidence of a cross talk between bone and glucose metabolism. Diabetes Care. 2015;38(8):1509–17. doi:10.2337/dc14-2989.
Arasu A, Cawthon PM, Lui LY, Do TP, Arora PS, Cauley JA, et al. Serum sclerostin and risk of hip fracture in older Caucasian women. J Clin Endocrinol Metab. 2012;97(6):2027–32. doi:10.1210/jc.2011-3419.
Ardawi MS, Rouzi AA, Al-Sibiani SA, Al-Senani NS, Qari MH, Mousa SA. High serum sclerostin predicts the occurrence of osteoporotic fractures in postmenopausal women: the Center of Excellence for Osteoporosis Research Study. J Bone Min Res. 2012;27(12):2592–602. doi:10.1002/jbmr.1718.
Starup-Linde J, Lykkeboe S, Gregersen S, Hauge EM, Langdahl BL, Handberg A, et al. Bone Structure and Predictors of Fracture in Type 1 and Type 2 Diabetes. J Clin Endocrinol Metab. 2016;101(3):928–36. doi:10.1210/jc.2015-3882.
Llaurado G, Megia A, Cano A, Gimenez-Palop O, Simon I, Gonzalez-Sastre M, et al. FGF-23/Vitamin D axis in type 1 diabetes: the potential role of mineral metabolism in arterial stiffness. PLoS One. 2015;10(10):e0140222. doi:10.1371/journal.pone.0140222.
Ito N, Wijenayaka AR, Prideaux M, Kogawa M, Ormsby RT, Evdokiou A, et al. Regulation of FGF23 expression in IDG-SW3 osteocytes and human bone by pro-inflammatory stimuli. Mol Cell Endocrinol. 2015;399:208–18. doi:10.1016/j.mce.2014.10.007.
Lai X, Price C, Modla S, Thompson WR, Caplan J, Kirn-Safran CB et al. The dependences of osteocyte network on bone compartment, age, and disease. Bone research. 2015;3.
Villarino ME, Sanchez LM, Bozal CB, Ubios AM. Influence of short-term diabetes on osteocytic lacunae of alveolar bone. A histomorphometric study. Acta Odontol Latinoam. 2006;19(1):23–8.
Portal-Nunez S, Lozano D, de Castro LF, de Gortazar AR, Nogues X, Esbrit P. Alterations of the Wnt/beta-catenin pathway and its target genes for the N- and C-terminal domains of parathyroid hormone-related protein in bone from diabetic mice. FEBS Lett. 2010;584(14):3095–100. doi:10.1016/j.febslet.2010.05.047.
Fu YW, He HB. Apoptosis of periodontium cells in streptozototocin- and ligature-induced experimental diabetic periodontitis in rats. Acta Odontol Scand. 2013;71(5):1206–15. doi:10.3109/00016357.2012.757638.
Tolosa MJ, Chuguransky SR, Sedlinsky C, Schurman L, McCarthy AD, Molinuevo MS, et al. Insulin-deficient diabetes-induced bone microarchitecture alterations are associated with a decrease in the osteogenic potential of bone marrow progenitor cells: preventive effects of metformin. Diabetes Res Clin Pract. 2013;101(2):177–86. doi:10.1016/j.diabres.2013.05.016.
Parajuli A, Liu C, Li W, Gu X, Lai X, Pei S, et al. Bone’s responses to mechanical loading are impaired in type 1 diabetes. Bone. 2015;81:152–60. doi:10.1016/j.bone.2015.07.012. Utilizing both in vitro and in vivo investigation, these researchers demonstrate that conditions of hyperglycemia impair the mechanosensing capabilities of osteocytes and diminished the anabolic response of bone to mechanical loading.
Seref-Ferlengez Z, Maung S, Schaffler MB, Spray DC, Suadicani SO, Thi MM. P2X7R-Panx1 Complex Impairs Bone Mechanosignaling under High Glucose Levels Associated with Type-1 Diabetes. PLoS One. 2016;11(5):e0155107. doi:10.1371/journal.pone.0155107.
Guanabens N, Gifre L, Peris P. The role of Wnt signaling and sclerostin in the pathogenesis of glucocorticoid-induced osteoporosis. Curr osteoporos Rep. 2014;12(1):90–7. doi:10.1007/s11914-014-0197-0.
Krakauer JC, McKenna MJ, Buderer NF, Rao DS, Whitehouse FW, Parfitt AM. Bone loss and bone turnover in diabetes. Diabetes. 1995;44(7):775–82.
Horowitz MC, Xi Y, Wilson K, Kacena MA. Control of osteoclastogenesis and bone resorption by members of the TNF family of receptors and ligands. Cytokine Growth Factor Rev. 2001;12(1):9–18.
Tsentidis C, Gourgiotis D, Kossiva L, Doulgeraki A, Marmarinos A, Galli-Tsinopoulou A, et al. Higher levels of s-RANKL and osteoprotegerin in children and adolescents with type 1 diabetes mellitus may indicate increased osteoclast signaling and predisposition to lower bone mass: a multivariate cross-sectional analysis. Osteoporos Int. 2016;27(4):1631–43. doi:10.1007/s00198-015-3422-5.
Mabilleau G, Petrova NL, Edmonds ME, Sabokbar A. Increased osteoclastic activity in acute Charcot’s osteoarthropathy: the role of receptor activator of nuclear factor-kappaB ligand. Diabetologia. 2008;51(6):1035–40. doi:10.1007/s00125-008-0992-1.
Wittrant Y, Gorin Y, Woodruff K, Horn D, Abboud HE, Mohan S, et al. High d(+)glucose concentration inhibits RANKL-induced osteoclastogenesis. Bone. 2008;42(6):1122–30. doi:10.1016/j.bone.2008.02.006.
Valcourt U, Merle B, Gineyts E, Viguet-Carrin S, Delmas PD, Garnero P. Non-enzymatic glycation of bone collagen modifies osteoclastic activity and differentiation. J Biol Chem. 2007;282(8):5691–703. doi:10.1074/jbc.M610536200.
Hie M, Shimono M, Fujii K, Tsukamoto I. Increased cathepsin K and tartrate-resistant acid phosphatase expression in bone of streptozotocin-induced diabetic rats. Bone. 2007;41(6):1045–50. doi:10.1016/j.bone.2007.08.030.
Thrailkill KM, Clay Bunn R, Nyman JS, Rettiganti MR, Cockrell GE, Wahl EC, et al. SGLT2 inhibitor therapy improves blood glucose but does not prevent diabetic bone disease in diabetic DBA/2J male mice. Bone. 2016;82:101–7. doi:10.1016/j.bone.2015.07.025.
Catalfamo DL, Calderon NL, Harden SW, Sorenson HL, Neiva KG, Wallet SM. Augmented LPS responsiveness in type 1 diabetes-derived osteoclasts. J Cell Physiol. 2013;228(2):349–61. doi:10.1002/jcp.24138. This study demonstrated that osteoclasts from NOD mice are hyperresponsive to RANKL stimulation resulting in increased cathepsin K and MMP9 and increased bone degradation and, at the same time, they are unresponsive to bone resorption inhibition by LPS.
Motyl K, McCabe LR. Streptozotocin, type I diabetes severity and bone. Biol Proc Online. 2009;11:296–315. doi:10.1007/s12575-009-9000-5.
Roszer T. Inflammation as death or life signal in diabetic fracture healing. Inflamm Res. 2011;60(1):3–10. doi:10.1007/s00011-010-0246-9.
Coe LM, Tekalur SA, Shu Y, Baumann MJ, McCabe LR. Bisphosphonate treatment of type I diabetic mice prevents early bone loss but accentuates suppression of bone formation. J Cell Physiol. 2015;230(8):1944–53. doi:10.1002/jcp.24929.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Iuliana Popescu, Kathryn Thrailkill, Robert Bunn, John Fowlkes, and Evangelia Kalaitzoglou declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Funding
This work was supported in part by National Institutes of Health Grants R01DK055653 (to J.L.F.) and R21AR070620 (to K.M.T). Additional funding was provided by the University of Kentucky Barnstable Brown Diabetes Center Endowment.
Additional information
This article is part of the Topical Collection on Bone and Diabetes
Rights and permissions
About this article
Cite this article
Kalaitzoglou, E., Popescu, I., Bunn, R.C. et al. Effects of Type 1 Diabetes on Osteoblasts, Osteocytes, and Osteoclasts. Curr Osteoporos Rep 14, 310–319 (2016). https://doi.org/10.1007/s11914-016-0329-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-016-0329-9