Abstract
Purpose of Review
This review aims to summarize the pathophysiology, clinical presentation, and management of acute myeloid leukemia (AML) with FMS-like tyrosine kinase-3 (FLT3) mutations.
Recent Findings
The recent European Leukemia Net (ELN2022) recommendations re-classified AML with FLT3 internal tandem duplications (FLT3-ITD) as intermediate risk regardless of Nucleophosmin 1 (NPM1) co-mutation or the FLT3 allelic ratio. Allogeneic hematopoietic cell transplantation (alloHCT) is now recommended for all eligible patients with FLT3-ITD AML. This review outlines the role of FLT3 inhibitors in induction and consolidation, as well as for post-alloHCT maintenance. It outlines the unique challenges and advantages of assessing FLT3 measurable residual disease (MRD) and discusses the pre-clinical basis for the combination of FLT3 and menin inhibitors. And, for the older or unfit patient ineligible for upfront intensive chemotherapy, it discusses the recent clinical trials incorporating FLT3 inhibitors into azacytidine- and venetoclax-based regimens. Finally, it proposes a rational sequential approach for integrating FLT3 inhibitors into less intensive regimens, with a focus on improved tolerability in the older and unfit patient population.
Summary
The management of AML with FLT3 mutation remains a challenge in clinical practice. This review provides an update on the pathophysiology and therapeutic landscape of FLT3 AML, as well as a clinical management framework for managing the older or unfit patient ineligible for intensive chemotherapy.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Levis M, Small D. FLT3: ITDoes matter in leukemia. Leukemia. 2003;17(9):1738–52. https://doi.org/10.1038/sj.leu.2403099.
Griffith J, Black J, Faerman C, et al. The structural basis for autoinhibition of FLT3 by the Juxtamembrane domain. Mol Cell. 2004;13(2):169–78. https://doi.org/10.1016/S1097-2765(03)00505-7.
Kayser S, Schlenk RF, Londono MC, et al. Insertion of FLT3 internal tandem duplication in the tyrosine kinase domain-1 is associated with resistance to chemotherapy and inferior outcome. Blood. 2009;114(12):2386–92. https://doi.org/10.1182/blood-2009-03-209999.
Yoshimoto G, Miyamoto T, Jabbarzadeh-Tabrizi S, et al. FLT3-ITD up-regulates MCL-1 to promote survival of stem cells in acute myeloid leukemia via FLT3-ITD-specific STAT5 activation. Blood. 2009;114(24):5034–43. https://doi.org/10.1182/blood-2008-12-196055.
Mead AJ, Kharazi S, Atkinson D, et al. FLT3-ITDs instruct a myeloid differentiation and transformation bias in lymphomyeloid multipotent progenitors. Cell Rep. 2013;3(6):1766–76. https://doi.org/10.1016/j.celrep.2013.04.031.
Boyer SW, Schroeder AV, Smith-Berdan S, Forsberg EC. All hematopoietic cells develop from hematopoietic stem cells through Flk2/Flt3-positive progenitor cells. Cell Stem Cell. 2011;9(1):64–73. https://doi.org/10.1016/j.stem.2011.04.021.
Lyman SD, James L, Johnson L, et al. Cloning of the human homologue of the murine flt3 ligand: a growth factor for early hematopoietic progenitor cells. Blood. 1994;83(10):2795–801.
Kikushige Y, Yoshimoto G, Miyamoto T, et al. Human Flt3 is expressed at the hematopoietic stem cell and the granulocyte/macrophage progenitor stages to maintain cell survival. J Immunol. 2008;180(11):7358–67. https://doi.org/10.4049/jimmunol.180.11.7358.
Deol A, Sengsayadeth S, Ahn KW, et al. Does FLT3 mutation impact survival after hematopoietic stem cell transplantation for acute myeloid leukemia? A Center for International Blood and Marrow Transplant Research (CIBMTR) analysis. Cancer. 2016;122(19):3005–14. https://doi.org/10.1002/cncr.30140.
Kottaridis PD, Gale RE, Langabeer SE, Frew ME, Bowen DT, Linch DC. Studies of FLT3 mutations in paired presentation and relapse samples from patients with acute myeloid leukemia: implications for the role of FLT3 mutations in leukemogenesis, minimal residual disease detection, and possible therapy with FLT3 inhibitors. Blood. 2002;100(7):2393–8. https://doi.org/10.1182/blood-2002-02-0420.
Stone RM, Mandrekar SJ, Sanford BL, et al. Midostaurin plus chemotherapy for acute myeloid leukemia with a FLT3 mutation. N Engl J Med. 2017;377(5):454–64. https://doi.org/10.1056/NEJMoa1614359.
Papaemmanuil E, Gerstung M, Bullinger L, et al. Genomic classification and prognosis in acute myeloid leukemia. N Engl J Med. 2016;374(23):2209–21. https://doi.org/10.1056/NEJMoa1516192.
Fiedler W, Kayser S, Kebenko M, et al. A phase I/II study of sunitinib and intensive chemotherapy in patients over 60 years of age with acute myeloid leukaemia and activating FLT3 mutations. Br J Haematol. 2015;169(5):694–700. https://doi.org/10.1111/bjh.13353.
Smith BD, Levis M, Beran M, et al. Single-agent CEP-701, a novel FLT3 inhibitor, shows biologic and clinical activity in patients with relapsed or refractory acute myeloid leukemia. Blood. 2004;103(10):3669–76. https://doi.org/10.1182/blood-2003-11-3775.
Knapper S, Russell N, Gilkes A, et al. A randomized assessment of adding the kinase inhibitor lestaurtinib to first-line chemotherapy for FLT3-mutated AML. Blood. 2017;129(9):1143–54. https://doi.org/10.1182/blood-2016-07-730648.
Röllig C, Serve H, Hüttmann A, et al. Addition of sorafenib versus placebo to standard therapy in patients aged 60 years or younger with newly diagnosed acute myeloid leukaemia (SORAML): a multicentre, phase 2, randomised controlled trial. Lancet Oncol. 2015;16(16):1691–9. https://doi.org/10.1016/S1470-2045(15)00362-9.
Perl AE, Martinelli G, Cortes JE, et al. Gilteritinib or chemotherapy for relapsed or refractory FLT3-mutated AML. N Engl J Med. 2019;381(18):1728–40. https://doi.org/10.1056/NEJMoa1902688.
Wang ES, Stone RM, Tallman MS, Walter RB, Eckardt JR, Collins R. Crenolanib, a Type I FLT3 TKI, Can be safely combined with cytarabine and anthracycline induction chemotherapy and results in high response rates in patients with newly diagnosed FLT3 mutant acute myeloid leukemia (AML). Blood. 2016;128(22):1071. https://doi.org/10.1182/blood.V128.22.1071.1071.
Altman JK, Foran JM, Pratz KW, Trone D, Cortes JE, Tallman MS. Phase 1 study of quizartinib in combination with induction and consolidation chemotherapy in patients with newly diagnosed acute myeloid leukemia. Am J Hematol. 2018;93(2):213–21. https://doi.org/10.1002/ajh.24974.
Smith CC, Wang Q, Chin CS, et al. Validation of ITD mutations in FLT3 as a therapeutic target in human acute myeloid leukaemia. Nature. 2012;485(7397):260–3. https://doi.org/10.1038/nature11016.
McMahon CM, Ferng T, Canaani J, et al. Clonal selection with RAS pathway activation mediates secondary clinical resistance to selective FLT3 Inhibition in acute myeloid leukemia. Cancer Discov. 2019;9(8):1050–63. https://doi.org/10.1158/2159-8290.CD-18-1453.
Fujifilm Pharmaceuticals U.S.A., Inc. A first-in-human phase 1/2a study to assess the safety, tolerability, efficacy, and pharmacokinetics of FF-10101-01 in subjects with relapsed or refractory acute myeloid leukemia. clinicaltrials.gov; 2022. Accessed October 20, 2022. https://clinicaltrials.gov/ct2/show/NCT03194685
Levis MJ, Smith CC, Perl AE, et al. Phase 1 first-in-human study of irreversible FLT3 inhibitor FF-10101–01 in relapsed or refractory acute myeloid leukemia. J Clin Oncol. 2021;39(15_suppl):7008–7008. https://doi.org/10.1200/JCO.2021.39.15_suppl.7008.
Döhner K, Thiede C, Jahn N, et al. Impact of NPM1/FLT3-ITD genotypes defined by the 2017 European LeukemiaNet in patients with acute myeloid leukemia. Blood. 2020;135(5):371–80. https://doi.org/10.1182/blood.2019002697.
Voso MT, Larson RA, Jones D, et al. Midostaurin in patients with acute myeloid leukemia and FLT3-TKD mutations: a subanalysis from the RATIFY trial. Blood Adv. 2020;4(19):4945–54. https://doi.org/10.1182/bloodadvances.2020002904.
Erba H. Quizartinib prolonged survival vs placebo plus intensive induction and consolidation therapy followed by single-agent continuation in patients 18–75 years with newly-diagnosed FLT3-ITD+ AML. Presented at: 11 2022; Vienna, Austria. https://library.ehaweb.org/eha/2022/eha2022-congress/356965/harry.erba.quizartinib.prolonged.survival.vs.placebo.plus.intensive.induction.html?f=menu%3D6%2Abrowseby%3D8%2Asortby%3D2%2Amedia%3D3%2Ace_id%3D2233%2Amarker%3D1749%2Afeatured%3D17676
Perl AE, Pratz KW. Incorporation of FLT3 inhibitors into the treatment regimens for FLT3 mutated acute myeloid leukemia. Cancer J. 2022;28(1):7.
Levis M, Perl AE. Gilteritinib: potent targeting of FLT3 mutations in AML. Blood Adv. 2020;4(6):1178–91. https://doi.org/10.1182/bloodadvances.2019000174.
Liu SB, Dong HJ, Bao XB, et al. Impact of FLT3-ITD length on prognosis of acute myeloid leukemia. Haematologica. 2019;104(1):e9–12. https://doi.org/10.3324/haematol.2018.191809.
Stichting Hemato-Oncologie voor Volwassenen Nederland. A phase 3, multicenter, open-label, randomized, study of gilteritinib versus midostaurin in combination with induction and consolidation therapy followed by one-year maintenance in patients with newly diagnosed acute myeloid leukemia (AML) or myelodysplastic syndromes with excess blasts-2 (MDS-EB2) with FLT3 mutations eligible for intensive chemotherapy (HOVON 156 AML / AMLSG 28-18). clinicaltrials.gov; 2022. Accessed August 15, 2022. https://clinicaltrials.gov/ct2/show/NCT04027309
Arog Pharmaceuticals, Inc. Phase III randomized study of crenolanib versus midostaurin administered following induction chemotherapy and consolidation therapy in newly diagnosed subjects with FLT3 mutated acute myeloid leukemia. clinicaltrials.gov; 2020. Accessed August 15, 2022. https://clinicaltrials.gov/ct2/show/NCT03258931
Pratz KW, Sato T, Murphy KM, Stine A, Rajkhowa T, Levis M. FLT3-mutant allelic burden and clinical status are predictive of response to FLT3 inhibitors in AML. Blood. 2010;115(7):1425–32. https://doi.org/10.1182/blood-2009-09-242859.
Ding L, Ley TJ, Larson DE, et al. Clonal evolution in relapsed acute myeloid leukaemia revealed by whole-genome sequencing. Nature. 2012;481(7382):506–10. https://doi.org/10.1038/nature10738.
Levis M. FLT3/ITD AML and the law of unintended consequences. Blood. 2011;117(26):6987–90. https://doi.org/10.1182/blood-2011-03-340273.
• National Comprehensive Cancer Network. Guidelines Detail.Acute myeloid leukemia version 2.2022. Published June 14, 2022. Accessed August 21, 2022. https://www.nccn.org/guidelines/guidelines-detail. (The NCCN Guidelines on AML are evidenced-based recommendations from an expert panel which are frequently updated.)
Döhner H, Weber D, Krzykalla J, et al. Midostaurin plus intensive chemotherapy for younger and older patients with AML and FLT3 internal tandem duplications. Blood Adv. 2022;6(18):5345–55. https://doi.org/10.1182/bloodadvances.2022007223.
Döhner H, Estey E, Grimwade D, et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood. 2017;129(4):424–47. https://doi.org/10.1182/blood-2016-08-733196.
•• Döhner H, Wei AH, Appelbaum FR, et al. Diagnosis and management of AML in adults: 2022 ELN recommendations from an international expert panel. Blood. 2022:blood.2022016867.https://doi.org/10.1182/blood.2022016867. (The ELN2022 recommendations are integral to clinical practice. This recent update from an expert panel describes the most recent classification, risk stratification, and management of AML.)
Polz MF, Cavanaugh CM. Bias in template-to-product ratios in multitemplate PCR. Appl Environ Microbiol. 1998;64(10):3724–30.
Zhou Y, Othus M, Araki D, et al. Pre- and post-transplant quantification of measurable ('minimal’) residual disease via multiparameter flow cytometry in adult acute myeloid leukemia. Leukemia. 2016;30(7):1456–64. https://doi.org/10.1038/leu.2016.46.
Thiede C, Steudel C, Mohr B, et al. Analysis of FLT3-activating mutations in 979 patients with acute myelogenous leukemia: association with FAB subtypes and identification of subgroups with poor prognosis: presented in part at the 42nd Annual Meeting of the American Society of Hematology, December 1–5, 2000, San Francisco, CA (abstract 2334). Blood. 2002;99(12):4326–35. https://doi.org/10.1182/blood.V99.12.4326.
Levis MJ, Perl AE, Altman JK, et al. A next-generation sequencing–based assay for minimal residual disease assessment in AML patients with FLT3-ITD mutations. Blood Adv. 2018;2(8):825–31. https://doi.org/10.1182/bloodadvances.2018015925.
Blätte TJ, Schmalbrock LK, Skambraks S, et al. getITD for FLT3-ITD-based MRD monitoring in AML. Leukemia. 2019;33(10):2535–9. https://doi.org/10.1038/s41375-019-0483-z.
Levis M, Shi W, Chang K, et al. FLT3 inhibitors added to induction therapy induce deeper remissions. Blood. 2020;135(1):75–8. https://doi.org/10.1182/blood.2019002180.
Thol F, Kölking B, Damm F, et al. Next-generation sequencing for minimal residual disease monitoring in acute myeloid leukemia patients with FLT3-ITD or NPM1 mutations. Genes Chromosom Cancer. 2012;51(7):689–95. https://doi.org/10.1002/gcc.21955.
Ambinder AJ, Levis M. Potential targeting of FLT3 acute myeloid leukemia. Haematologica. 2020;106(3):671–81. https://doi.org/10.3324/haematol.2019.240754.
• Burchert A, Bug G, Fritz LV, et al. Sorafenib maintenance after allogeneic hematopoietic stem cell transplantation for acute myeloid leukemia with FLT3 –internal tandem duplication mutation (SORMAIN). J Clin Oncol. 2020;38(26):2993–3002. https://doi.org/10.1200/JCO.19.03345. (Together with reference (50) this Phase II clinical trial supports the use of sorafenib for post-alloHCT maintenance in FLT3-ITD AML.)
Maziarz RT, Levis M, Patnaik MM, et al. Midostaurin after allogeneic stem cell transplant in patients with FLT3-internal tandem duplication-positive acute myeloid leukemia. Bone Marrow Transplant. 2021;56(5):1180–9. https://doi.org/10.1038/s41409-020-01153-1.
Schlenk RF, Weber D, Fiedler W, et al. Midostaurin added to chemotherapy and continued single-agent maintenance therapy in acute myeloid leukemia with FLT3-ITD. Blood. 2019;133(8):840–51. https://doi.org/10.1182/blood-2018-08-869453.
• Xuan L, Wang Y, Huang F, et al. Sorafenib maintenance in patients with FLT3-ITD acute myeloid leukaemia undergoing allogeneic haematopoietic stem-cell transplantation: an open-label, multicentre, randomised phase 3 trial. Lancet Oncol. 2020;21(9):1201–12. https://doi.org/10.1016/S1470-2045(20)30455-1. (Together with reference (47) this Phase III randomized clinical trial supports the use of sorafenib for post-alloHCT maintenance in FLT3-ITD AML.)
Burchert A. Maintenance therapy for FLT3-ITD-mutated acute myeloid leukemia. Haematologica. 2021;106(3):664–70. https://doi.org/10.3324/haematol.2019.240747.
Arai Y, Chi S, Minami Y, Yanada M. FLT3-targeted treatment for acute myeloid leukemia. Int J Hematol. 2022. https://doi.org/10.1007/s12185-022-03374-0
•• DiNardo CD, Jonas BA, Pullarkat V, et al. Azacitidine and venetoclax in previously untreated acute myeloid leukemia. N Engl J Med. 2020;383(7):617–29. https://doi.org/10.1056/NEJMoa2012971. (This recent Phase III randomized clinical trial has changed the standard of care for the management of newly-diagnosed AML in patients unfit for intensive chemotherapy.)
Ohanian M, Garcia-Manero G, Levis M, et al. Sorafenib combined with 5-azacytidine in older patients with untreated FLT3-ITD mutated acute myeloid leukemia. Am J Hematol. 2018;93(9):1136–41. https://doi.org/10.1002/ajh.25198.
Swaminathan M, Kantarjian HM, Levis M, et al. A phase I/II study of the combination of quizartinib with azacitidine or low-dose cytarabine for the treatment of patients with acute myeloid leukemia and myelodysplastic syndrome. Haematologica. 2021;106(8):2121–30. https://doi.org/10.3324/haematol.2020.263392.
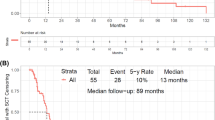
Wang ES, Montesinos P, Minden MD, et al. Phase 3 trial of gilteritinib plus azacitidine vs azacitidine for newly diagnosed FLT3mut+ AML ineligible for intensive chemotherapy. Blood. 2022;140(17):1845–57. https://doi.org/10.1182/blood.2021014586.
Mali RS, Zhang Q, DeFilippis R, et al. Venetoclax combines synergistically with FLT3 inhibition to effectively target leukemic cells in FLT3-ITD+ acute myeloid leukemia models. Haematologica. 2021;106(4):1034–46. https://doi.org/10.3324/haematol.2019.244020.
Ma J, Zhao S, Qiao X, et al. Inhibition of Bcl-2 synergistically enhances the antileukemic activity of midostaurin and gilteritinib in preclinical models of FLT3-mutated acute myeloid leukemia. Clin Cancer Res Off J Am Assoc Cancer Res. 2019;25(22):6815–26. https://doi.org/10.1158/1078-0432.CCR-19-0832.
Maiti A, DiNardo CD, Daver NG, et al. Triplet therapy with venetoclax, FLT3 inhibitor and decitabine for FLT3-mutated acute myeloid leukemia. Blood Cancer J. 2021;11(2):25. https://doi.org/10.1038/s41408-021-00410-w.
Perl AE, Daver NG, Pratz KW, et al. Venetoclax in combination with gilteritinib in patients with relapsed/refractory acute myeloid leukemia: a phase 1b study. Blood. 2019;134(Supplement_1):3910. https://doi.org/10.1182/blood-2019-127416.
Daver N. Efficacy and safety of venetoclax in combination with gilteritinib for relapsed/refractory FLT3 mutated acute myeloid leukemia in the expansion cohort of a phase 1b study. In: ASH; 2020. Accessed July 18, 2022. https://ash.confex.com/ash/2020/webprogram/Paper139705.html
Daver N. Venetoclax in combination with gilteritinib demonstrates molecular clearance of FLT3 mutation in relapsed/refractory FLT3 mutated acute myeloid leukemia. In: ASH; 2021. Accessed July 18, 2022. https://ash.confex.com/ash/2021/webprogram/Paper150743.html
M.D. Anderson Cancer Center. A phase I/II study of ASTX727, Venetoclax, and gilteritinib for patients with acute myeloid leukemia or high-risk myelodysplastic syndrome with an activating FLT3 mutation. clinicaltrials.gov; 2022. Accessed October 20, 2022. https://clinicaltrials.gov/ct2/show/NCT05010122
PETHEMA Foundation. A Phase I-II, Multicentre, open label clinical trial to assess the safety and tolerability of the combination of low-dose cytarabine or azacitidine, plus venetoclax and quizartinib in newly diagnosed acute myeloid leukemia patients aged equal or more than 60 years old ineligible for standard induction chemotherapy. clinicaltrials.gov; 2022. Accessed October 20, 2022. https://clinicaltrials.gov/ct2/show/NCT04687761
Cortes JE, Khaled S, Martinelli G, et al. Quizartinib versus salvage chemotherapy in relapsed or refractory FLT3-ITD acute myeloid leukaemia (QuANTUM-R): a multicentre, randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2019;20(7):984–97. https://doi.org/10.1016/S1470-2045(19)30150-0.
FDA declines to approve quizartinib for FLT3-mutated acute myeloid leukemia. Published online December 30, 2021.Accessed August 31, 2022. https://ashpublications.org/ashclinicalnews/news/4584/FDA-Declines-to-Approve-Quizartinib-for-FLT3
Dzama MM, Steiner M, Rausch J, et al. Synergistic targeting of FLT3 mutations in AML via combined menin-MLL and FLT3 inhibition. Blood. 2020;136(21):2442–56. https://doi.org/10.1182/blood.2020005037.
Syndax Pharmaceuticals. A phase 1/2, open-label, dose-escalation and dose-expansion cohort study of SNDX-5613 in patients with relapsed/refractory leukemias, including those harboring an MLL/KMT2A gene rearrangement or nucleophosmin 1 (NPM1) mutation. clinicaltrials.gov; 2022. Accessed September 22, 2022. https://clinicaltrials.gov/ct2/show/NCT04065399
Kura Oncology, Inc. A phase 1/2a first in human study of the menin-MLL(KMT2A) inhibitor KO-539 in patients with relapsed or refractory acute myeloid leukemia. clinicaltrials.gov; 2022. Accessed September 22, 2022. https://clinicaltrials.gov/ct2/show/NCT04067336
Bullinger L, Döhner K, Döhner H. Genomics of acute myeloid leukemia diagnosis and pathways. J Clin Oncol. 2017. https://doi.org/10.1200/JCO.2016.71.2208
Miao H, Kim E, Chen D, et al. Combinatorial treatment with menin and FLT3 inhibitors induces complete remission in AML models with activating FLT3 mutations. Blood. 2020;136(25):2958–63. https://doi.org/10.1182/blood.2020006575.
Stein EM. Safety and efficacy of menin inhibition in patients with MLL-rearranged and NPM1 mutant acute leukemia: a phase 1, first-in-human study of SNDX-5613 (AUGMENT 101). Presented at: December 13, 2021; American Society of Hematology Annual Meeting & Exposition 2021.
Wang ES. Preliminary data on a phase 1/2A first in human study of the menin-KMT2A (MLL) inhibitor KO-539 in Patients with Relapsed or refractory acute myeloid leukemia. Presented at: December 5, 2020.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
Rebecca Bystrom does not have any conflict of interest. Mark Levis is a consultant for Abbvie, Amgen, Astellas, Bristol Myers Squibb, Daiichi Sankyo, and Jazz and receives research funding from Astellas and FujiFilm.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bystrom, R., Levis, M.J. An Update on FLT3 in Acute Myeloid Leukemia: Pathophysiology and Therapeutic Landscape. Curr Oncol Rep 25, 369–378 (2023). https://doi.org/10.1007/s11912-023-01389-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11912-023-01389-2