Abstract
Organ transplantation represents one of the great success stories of 20th century medicine. However, its continued success is greatly limited by the shortage of donor organs. This has led to an increased focus within the critical care community on optimal identification and management of the potential organ donor. The multi-organ donor can represent one of the most complex intensive care patients, with numerous competing physiological priorities. However, appropriate management of the donor not only increases the number of organs that can be successfully donated but has long-term implications for the outcomes of multiple recipients. This review outlines current understandings of the physiological derangements seen in the organ donor and evaluates the available evidence for management strategies designed to optimize donation potential and organ recovery. Finally, emerging management strategies for the potential donor are discussed within the current ethical and legal frameworks permitting donation after both brain and circulatory death.
Similar content being viewed by others
Introduction
Organ transplantation represents the optimal treatment for end-stage organ dysfunction. Currently the greatest limiting factor in the ongoing success of transplantation is the widening disparity between supply of adequate donor organs and demand for transplantation [1, 2]. This has led to an increased focus within the critical care and transplant community on optimizing the utilization of donor organs, through active management of the potential donor and through broadening of the donor eligibility criteria. For the intensivist, the potential multi-organ donor is a complex patient to manage. They may have profound physiological and homeostatic derangements, and there are often competing management priorities between different organs, which must be balanced to optimize overall donation potential. The growing acceptance of marginal donors, and re-emergence of donation after circulatory death (DCD), has added further complexity. Increasingly there has been a move toward protocol-based critical care management of organ donors; however, it is important to understand the available evidence on which protocols are based, and its limitations.
This review outlines current understandings of the physiological derangements seen in the organ donor and evaluates available evidence for management strategies designed to optimize donation potential and organ recovery, with reference to both donation after brain and circulatory death.
Defining the Potential Donor in 21st Century Transplantation
Prior to the acceptance of the concept of brain death, all organs were procured following cardiac arrest of the donor. The establishment of the Harvard Criteria for brain death in 1968 [3] allowed for donation after brain death (DBD), which remains the principal source of donor organs in most Western countries today. Brain death is associated with derangements in hemodynamic, endocrine, and metabolic homeostatic processes [4]. Subsequently, strategies for the management of organ donors have primarily focused on the normalization of donor physiology following brain death [5].
The persistent shortfall of organs for transplantation has resulted in the recent re-emergence of DCD as a means of expanding the donor pool, re-defining the nature of the potential donor in the 21st century. In DCD, death is declared only after the heart has stopped, and there must be proof of irreversibility, before donation procedures can be commenced. Potential DCD donors have usually sustained a catastrophic brain injury or other end-stage disease (musculoskeletal, pulmonary, severe high spinal cord injury) where there is no expectation for meaningful survival, but who do not otherwise meet brain death criteria [6–8]. The first international workshop on DCD took place in Maastricht in 1995. It defined four types of DCD and a further category was added in 2000 [9] (Table 1; [10]). Controlled DCD (Category III and IV) has since become a potential group of organ donors in many centers. Uncontrolled DCD (category I, II, and V) is rarely performed outside of Spain, and is not permitted in many countries.
DCD donation involves a significantly different set of pre-donation processes compared to DBD. As such the nature of the potential donor in the 21st century has developed to include two physiologically and legally distinct types of organ donor requiring intensive care management.
Donation After Brain Death Management
Hemodynamics
The cardiovascular system is profoundly affected by brain death [11]. Brainstem ischemia caused by rising intracranial pressure initially results in systemic hypertension, in an attempt to maintain cerebral perfusion. Ischemia progresses in a rostral-caudal direction, causing parasympathetic activation and sinus bradycardia. Unopposed sympathetic stimulation follows as ischemia reaches the medulla oblongata, resulting in an intense but transient “autonomic storm” with massive catecholamine release, which causes vasoconstriction and diminishes end-organ perfusion [4]. Finally, cerebral herniation and spinal cord ischemia lead to deactivation of the sympathetic nervous system, catecholamine insufficiency, and blunted homeostatic responses [12] causing marked vasodilation, a fall in cardiac output, and hemodynamic instability. These physiological perturbations may then result in the development of myocardial necrosis [13], predisposing to arrhythmias [14].
While systemic hypertension generally represents a transient phase in the progression to brainstem death, the hypotension that follows is profound, sustained, and threatens organ viability [15]. The etiology of hypotension in the brain-dead donor is multifactorial, and well described elsewhere [16]. In addition to neurohormonal disturbances precipitating vasodilation and capillary leakage, donors are often intravascularly deplete prior to brain death either as a result of osmotic therapy used to manage rising intracranial pressures, or blood loss. This is compounded by the development of diabetes insipidus (DI), which occurs as a result of the panhypopituitarism accompanying brain death. Failure to correct these cardiovascular disturbances will result in poor end-organ perfusion and inadequate tissue oxygenation.
Immediate hemodynamic management should focus on correction of hypovolemia and support of perfusion pressure and cardiac output. Where cardiac donation is considered, echocardiography is often helpful. Early poor echocardiography parameters (left ventricular ejection fraction <45 %) are an indication for institution of more aggressive management and monitoring strategies, rather than an absolute contraindication to cardiac donation per se, as initial myocardial dysfunction can often be successfully corrected [17].
When hemodynamic stabilization is not achieved despite adequate volume expansion, cautious use of vasoactive drugs is warranted. Dopamine has been the inotropic agent of choice [18], with addition of a second vasoactive agent in patients with dopamine requirements >10 ug/kg/min. Both dopamine and other catecholamines have been shown to have immunomodulatory effects, inhibiting upregulation of adhesion molecules [19], which may be of benefit in reducing the systemic inflammatory response (SIR) to brain death. However, dopamine has also been shown to suppress the function of anterior pituitary hormones [20].
High requirements for vasoactive support were initially considered grounds for exclusion from donation, although subsequent data in the late 1990s showed limited or no association between vasopressor requirements and outcome after transplantation [19, 21, 22].
There has been a move away from high-dose vasoactive therapy toward the use of vasopressin, based on studies demonstrating successful maintenance of hemodynamic stability and a catecholamine-sparing effect in DBD without impairment of graft function [23••, 24, 25]. Vasopressin (± arginine) is currently recommended by the American College of Cardiology as the initial therapy of choice for achieving donor hemodynamic stability [26]. Vasopressin also enhances the vascular sensitivity to catecholamines, and where hemodynamic stability cannot be achieved with vasopressin alone [27], its use in conjunction with catecholamines assists in minimizing vasoactive requirements. However, high-quality clinical trials comparing the different inotropic and pressor agents in the donor population are lacking.
When hemodynamic goals are not achieved despite the use of vasopressor and inotropic agents, institution of hormonal therapy is warranted.
Pulmonary Considerations
The lungs remain one of the most difficult organs to preserve following brain death, being transplanted in only 15–25 % of donors [28, 29]. They are vulnerable to a series of injuries both prior to and after the onset of brain death. While some donor factors associated with poor outcome (eg, donor age and smoking status) are fixed, many factors (eg, prolonged mechanical ventilation, broncho-aspiration, atelectasis, barotrauma, and hemodynamic instability) are potentially modifiable through optimal donor resuscitation and management. With appropriate management strategies significant reconditioning is possible, allowing successful conversion to donation, with acceptable short- and medium-term outcomes [30, 31•].
The onset of brainstem death results in acute systemic vasoconstriction and a rise in systemic vascular resistance. Left ventricular output decreases and left atrial pressure rises, venous return increases, and blood is shifted into the more compliant pulmonary circulation, elevating hydrostatic pressures across the pulmonary capillary membrane [32] and resulting in neurogenic pulmonary edema. Uncontrolled sympathetic activity triggers an SIR, initiating infiltration of neutrophils and increasing pulmonary endothelial permeability, which further contributes to lung injury [33, 34]. The local release of proinflammatory cytokines is a prominent feature in DBD. Bronchoalveolar lavage concentrations of neutrophils and interleukin-8 have been shown to be predictive of early graft failure and mortality after lung transplantation [35, 36]. Interestingly, proinflammatory pathway activation and subsequent SIR-mediated lung injury appear to be features of DBD but not DCD lungs [37, 38], suggesting that these inflammatory changes, which may contribute to both early and late graft dysfunction, are unique to the process of brain death. Finall, hormonal instability appears to reduce alveolar fluid clearance (AFC) resulting in significant accumulation of extravascular lung water [39].
Adequate gas exchange and good oxygenation are considered to be the most important indicator for the functional quality of the lung [28]. However, even if initial Pa02/Fi02 is poor, scope exists for improving these parameters as part of an aggressive donor management strategy [40], and an isolated finding of a marginal arterial P02 should not on its own be used as grounds for exclusion. The PaO2/FiO2 ratio can be affected by reversible processes such as retained secretions, pulmonary edema, and atelectasis. Endobronchial suctioning should be performed regularly and bronchoscopy undertaken to assess the airways and remove mucous plugs.
Approaches to mechanical ventilation of the donor are highly variable [41]. Current trends favor the use of low tidal volume ventilation, based on evidence from studies of acute respiratory distress syndrome [42]; however, there are no prospective randomized trials in organ donors. Pulmonary recruitment maneuvers (involving short periods of pressure-controlled ventilation with inspiratory pressures of 25 cm H20 and a positive end-expiratory pressure [PEEP] of 15 cm H20 for 2 h before return to conventional volume-controlled ventilation with a lower PEEP of 5 cm H20) have been shown to prevent atelectasis and open alveoli, thereby improving gas exchange in potential donors [30, 43]. Administration of aerosolized terbutaline has been shown to increase AFC via β-adrenergic stimulation in an ex vivo human lung model [44] and in a porcine model [45] and is currently the subject of a randomized multicenter controlled trial (BOLD study; β-agonist for oxygenation in lung donors) [46•]. In addition, triiodothyronine (T3) and low-dose dopamine may increase AFC [44, 47].
Management strategies in the potential lung donor require careful consideration of cardiopulmonary interactions. Unlike in the abdominal organs, where aggressive fluid resuscitation is beneficial to maintain organ perfusion, excessive fluid administration can cause rapid deterioration in lung function and preclude donation. In addition, the use of catecholamines has been associated with impaired gas exchange when the lungs are subsequently used for transplantation [48].
Hormonal Therapy
Brainstem herniation and ischemia results in the sudden transient release of catecholamines from the post-ganglionic sympathetic nerve endings, the so-called “catecholamine storm” [13, 14, 49]. This catecholamine surge is followed by sustained pituitary failure, with gross disturbances in circulating levels of cortisol, thyroid hormones, anti-diuretic hormone (ADH), and insulin [14, 50]. The correction of these hormonal changes in the donor remains an area of contention due to conflicting published experimental and clinical results [13, 14, 49].
Posterior pituitary insufficiency, resulting in ADH depletion and development of central DI, is seen in up to 90 % of DBD donors [51, 52]. Exogenous replacement of ADH in DBD (with arginine vasopressin or desmopressin) has been shown to improve graft function in kidney, liver, and cardiac recipients [17, 53, 54]. Arginine vasopressin confers the added advantage of a combined vasopressor and antidiuretic effect but high doses may induce coronary, renal, and splanchnic vasoconstriction [55].
Volume replacement is essential in the management of DI. Following initial volume expansion to correct hypovolemia, the use of hypotonic volume replacement to actively correct serum hypernatremia has been advocated. Hypernatremia has been shown in several retrospective series to be associated with an increased rate of primary nonfunction (PNF) in liver transplantation [56–58]. Moreover, correction of severe hypernatremia (>155 mM) prior to procurement appeared to abrogate post-transplant liver dysfunction [59]. Recently, the importance of both peak and terminal serum hypernatremia in the donor on post-transplant liver function has been challenged. In a single-center series of 1013 DBD liver donors, neither moderate (160–169 mEq/L) nor severe (>170 m Eq/L) peak or terminal serum sodium concentrations impacted on graft survival up to 1 year post-transplant [60]. These findings have been supported by three smaller studies [61–63], suggesting that donor hypernatremia should not be a reason for exclusion of liver donation.
Deficiencies of the anterior pituitary hormones have been reported in organ donors—specifically T3, thyroxine (T4), adrenocorticotropic hormone, thyroid-stimulating hormone, and human growth hormone. However, early results investigating the role of thyroid hormone replacement in DBD were conflicting. To address this, a multicenter retrospective analysis evaluating hormonal resuscitation (HR) was undertaken by the United Network of Organ Sharing (UNOS), involving 10,292 donors. Donors that were treated with three-drug (methylprednisone, T3/T4, and arginine vasopressin) HR protocols had a mean number of organs transplanted per donor (OTPD) 22.5 % higher than those managed with no HR (P < 0.001) [64]. Three-drug HR was associated with a statistically significant increased probability of successful kidney (7.3 %), heart (4.7 %), liver (4.9 %), lung (2.8 %), and pancreas (6 %) donation and improved recipient survival at 1 year.
Hyperglycemia is often encountered in the DBD donor, in part due to the development of insulin resistance [65]. There is minimal data to support or refute the use of tight glycemic control in the potential donor. Significant hyperglycemia (glucose > 200 mg/dL) is known to damage the pancreatic β cells and has been reported as a risk factor for PNF in pancreas recipients [66]. Given the conflicting results reported with tight glycemic control in the general intensive care population, management strategies directed at maintenance of normoglycemia using short-acting insulin infusions seem reasonable.
Monitoring and Goals of Management
Successful donation and acceptable graft outcomes are dependent on the maintenance of hemodynamic stability in the potential donor. Management goals are based on achieving normovolemia to achieve optimal tissue perfusion, while minimizing vasoactive drug therapy [16]. Simultaneous assessment and management of the potential donor is required, which may require specialized monitoring to achieve specific goals, particularly in the hemodynamically unstable donor.
Almost all potential DBD donors will have invasive monitoring prior to declaration of brain death and these should remain in place. Serial echocardiography yields substantial information, particularly in the potential cardiac donor. Ejection fraction is frequently poor, particularly immediately post-catecholamine storm, but this does not preclude eventual heart donation, as the use of hormonal therapy may “salvage” donation potential [17]. Most centers with published protocols aim for a minimum mean airway pressure (MAP) of between 60 and 65 mm Hg, heart rate of 60–100 bpm, and urine output of 0.5–3 mL/kg/hr, although the evidence to support the use of these as end goals is not well established [23••].
Failure to meet hemodynamic goals despite adequate volume replacement is considered indication for institution of invasive hemodynamic monitoring [67]. This may include use of a pulmonary artery catheter, serial echocardiography (transesophageal provides the most reliable images [68]), and/or the use of newer devices that employ transpulmonary thermodilution and pulse contour analysis to calculate cardiac output, stroke volume variation, intrathoracic blood volume, and extravascular lung water (pulse contour continuous cardiac output [PiCCO], or USCOM™) [69]. While a number of different devices exist, based on currently available evidence, the protocol followed for achieving end goals appears more important than the type of monitoring [17, 69, 70].
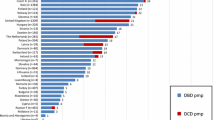
Standardization of donor management through the use of specific clinical parameters as end points of resuscitation—so-called donor management goals (DMGs)—has improved the outcome of potential donors [70–72]. Currently no national or international guidelines for best practice exist, in part because evidence to support the use of specific DMGs has only recently started to emerge [23••, 73]. DMGs vary between centers, but those reported in the literature have included MAP, average central venous pressure, pH, terminal PaO2, terminal sodium, terminal glucose, vasopressor use (number and dose), and urine output as resuscitation end points. Achievement of DMGs is associated with a significant overall increase in the number of OTPD in standard criteria donor, with less benefit seen in extended criteria and DCD donors [73]. UNOS recently reported on their early experiences using eight common DMGs. Achievement of DMGs increased the number of OTPD; however, on multivariate analysis the only significant independent variables were terminal PaO2 > 100 mm Hg, low vasopressor use (≤1 vasopressor used at low dose; dopamine <10 ug/kg/min, phenylephrine <60 ug/min, norepinephrine <10 ug/min), and glucose control (<200 mg/dL). Successful transplantation of thoracic organs was more dependent on the attainment of DMGs than that of abdominal organs. In keeping with international difficulties in successfully procuring lungs, lungs were found to be the least resilient organ in the presence of suboptimal donor parameters, particularly PaO2, where a 10- to 15-fold increase in successful lung transplantation was seen when this parameter was met [23••].
The Multi-Organ Donor
The US Health Resources and Human Services Administration stipulates among its national goals for organ donation an achievement of 3.75 OTPD [23••]. In the face of worsening donor shortages, maximizing OTPD provides a means of expanding the donor pool. Management of the multi-organ donor represents a unique challenge for the intensivist, as different organs have competing requirements. Notably, organ perfusion requirements, as well as the choice of fluid therapy and end management goals used to address and monitor these, differ markedly. Liberal volume replacement is important for maintaining optimal organ function in the kidney, but may be detrimental to the lungs. Therefore, early identification of individuals in whom the lungs are potentially suitable for donation allows for implementation of a more focussed management strategy. While inotropic support may improve renal perfusion, it is associated with cardiac graft dysfunction [74], so it needs to be titrated cautiously. HR has been shown to rescue potential donors; however, prolonged periods of HR post declaration of brain death are associated with poorer outcomes for cardiac [75] and renal [76] recipients and increase the likelihood of progression to somatic death [77••], thereby risking the viability of all organs.
Donation After Circulatory Death Management
Legal, Moral, and Ethical Issues for the Intensivist
A resurgence of interest in DCD has occurred as a result of international recognition of the need to increase the organ donation rate [78]. The role of DCD in transplantation has dominated both the donor and recipient literature in recent years. The relative risks and benefits of DCD, as well as the ethical and legal considerations when managing the potential DCD donor, remain controversial [8]. In most countries, DCD has not been directly addressed by existing law, resulting in varied interpretation of organ and transplant legislation designed for the DBD donor; these complex issues are well covered in the first book on the subject [79].
Given the moral, ethical, legal, and practical complexities of DCD, strong and explicit coordination of care of potential donors is essential between emergency physicians, intensivists, organ procurement organizations, and transplant surgeons.
Controlled DCD are predominantly intensive care unit patients, and represent the vast majority of DCD donors worldwide. Controlled DCD involves planned withdrawal of treatment in the face of catastrophic illness, where a competent patient or next of kin has consented. The decision to withdraw treatment must be made entirely independently and prior to any discussion about donation. DCD should only be considered when DBD is not possible [8], when the organ procurement team and transplant surgeons have experience in the management of the DCD donor, and where a hospital DCD protocol is in place [6–8, 80, 81]. As with DBD, identification of potential DCD donors and notification of the organ procurement team is the responsibility of the ICU.
Withdrawal of Ventilator and Organ Perfusion Support and Declaration of Death
To minimize warm ischemic time (WIT), withdrawal of life-supporting treatment should take place in the operating room [8]. Withdrawal of support, administration of medications such as morphine to minimize distress, monitoring of vital signs, clinical documentation, and the certification of death must be done by the patients’ physician, independent of the transplant team. It is imperative that this division between treating team and procurement team is maintained, and failure to maintain boundaries has been the cause of a highly publicized lawsuit [82].
Organ donation can only commence following certification of death. If the time between withdrawal of treatment and certification of death is prolonged or characterized by hemodynamic instability, hypoxic organ damage is likely. Different organs have differing tolerance to this period of warm ischemia. In liver transplantation a WIT—defined as the time that systolic blood pressure is less than 50 mm Hg to commencement of aortic perfusion—of more than 30 min is considered grounds for failure to donate [7, 83–85]. Kidneys are more resistant to the effects of warm ischemia, and many centers would still transplant grafts with a WIT of up to 60–120 min.
Reliably predicting which patients are likely to die within a timeframe that permits donation following withdrawal of life-supporting treatment is difficult as it depends on multiple factors including the patients’ hemodynamic, respiratory, and neurological status as well as the impact of treatment withdrawal. Two numerical tools have been created, the University of Wisconsin DCD and the UNOS tools, to identify potential DCD donors who are likely to die within 60 min of withdrawal of life-sustaining treatment [86, 87]. The utility of these scoring systems in the setting of transplantation is limited due to derivation bias, lack of validation, and limited generalizability. Families need to be made aware that not all potential DCD will proceed to donation. In patients who are not certified dead, end-of-life care is continued in the ICU or ward environment as it would be for patients who were not potential donors.
Following certification of death, a waiting period must be observed prior to commencement of donation to exclude the possibility of “auto-resuscitation.” This so-called “no-touch” period remains under debate and a range of waiting period durations have been endorsed [6, 8, 80, 88]. Currently the no-touch period appears to be arbitrarily set between 2 and 5 min at most centers [7, 8]. The chance of auto-resuscitation needs to be balanced against the knowledge that WIT has a detrimental effect on recipient outcome [89]. Until such time as further evidence becomes available, a minimum period of 2 min and a maximum period of 5 min waiting time seem appropriate.
Premortem Intensive Care Management in DCD
The use of pharmacological therapies aimed at stabilizing the donor to facilitate successful procurement of organs has become standard practice in the setting of DBD. These management strategies are implemented after the declaration of brain death and prior to donation over a period of several hours to days. The use of both pharmacological and invasive strategies in the DCD donor to maximize donation potential prior to certification of death is controversial. Ethical questions have been raised over the use of therapies aimed at maintaining or improving donor potential that have no direct benefit to the donor, but carry a theoretical risk of hastening death [90]. In some centers, premortem administration of heparin by the donor’s treating team close to but prior to the time of withdrawal of support is routine, on the basis that heparin is unlikely to hasten the death of the donor but facilitates organ perfusion and therefore graft function. In much of Europe, the Maastricht policy is followed, which precludes the use of medication that is not beneficial to the patient until after death [91]. Where premortem donor therapies are administered, most hospital protocols and practice guidelines recommend that specific informed consent for each agent is obtained from the patient’s next of kin prior to withdrawal of support [7, 92, 93].
More invasive premortem strategies for improving organ recovery in DCD have been proposed. As prolonged warm ischemia is associated with high rates of delayed graft function and PNF, minimizing WIT through rapid recovery techniques and prompt cooling to slow metabolic demand in the tissues is critically important. Premortem cannulation—in which the femoral artery and vein are cannulated prior to withdrawal of organ support to allow rapid infusion of cold preservation solution after declaration of death—is practiced by some centers. Femoral arterial and venous catheters (± aortic occlusion balloons) have also been placed during the premortem period for use with extracorporeal membrane oxygenation (ECMO) after certification of death [94]. However, the use of ECMO in the setting of DCD remains one of the most controversial areas in transplantation currently. Early single-center experiences with ECMO have shown improved outcomes in kidney, livers, and pancreas recipients [92–96], expanding the potential organ donor pool by 33 % in one series [95]. However, concerns have been raised that ECMO-assisted DCD without the use of a thoracic aortic occlusion balloon prevents brainstem death and allows for cerebral reanimation, retroactively interfering with the determination of death. Even when used with an occlusion balloon the technique is highly invasive and while within legal frameworks for donation, some have contended it violates the spirit on which legislation to protect the donor was formed [97•].
The ECMO-assist debate highlights one of the ongoing key ethical questions for all premortem donor management—the need to protect the best interests of their dying patient, while simultaneously facilitating their wish to donate. In the face of considerable scarcity of donor organs, it is imperative that end-of-life care for the dying patient is not compromised by the desire to protect and preserve organ function for future recipients. Furthermore, it is the responsibility of the intensive care community to uphold standards of care and ensure safe practice in this area. Failure to do so risks jeopardizing the public, professional, and legal support that is fundamental to the development and success of DCD programs.
Conclusions
Optimal care of the potential organ donor is one of the most important and often overlooked aspects of transplantation. Despite recent advances in our understanding of the processes of death in the context of donation, the area remains medically challenging and ethically complex.
Management strategies for the DBD donor have begun to shift from those aimed primarily at correcting pathophysiological disturbances associated with brain death, to an algorithmic management approach based on achieving clinically relevant end goals to increase the number and quality of transplantable organs from each donor. Given the success of early goal directed management protocols in other areas of intensive care medicine, this approach seems warranted. Our understanding of optimal management of the DCD donor remains in its infancy and the focus to date has been on defining the moral and ethical boundaries from which donor management strategies can be developed. Concerns have been raised that DCD has occurred at the expense of DBD donation, rather than as a new source of donors. As the clinical and legal framework for identifying and managing potential DCD donors is established, more research into the relative benefits of different management strategies will be required.
The recent intense interest in DCD appears to have diverted focus away from optimizing management of the DBD donor. However, many questions pertaining to the DBD donor remain incompletely answered. While the authors recognize the challenges in conducting sound clinical research in this field, commitment to undertaking high-quality prospective research—ideally randomized controlled trials (RCTs)— to inform best practice remains paramount to optimize donation practice, and in turn recipient outcomes. In both the DBD and DCD literature there continues to be a heavy reliance on evidence from retrospective analysis of databases to inform decision making and guide protocol development. Several pressing clinical questions for DBD organ donor management—namely the role of vasopressor versus inotropic agents, the importance of hormonal therapy in the stable donor, the significance of maintaining tight glycemic control in the donor, and the role of invasive cardiac monitoring—are only likely to be definitively answered by well-designed, multicenter clinical trials. Until such time as this occurs, developing standardized evidence-based recommendations as to optimal management strategies for the potential organ donor remains difficult.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Langone A, Helderman J. Disparity between solid-organ supply and demand. NEJM. 2003;349:704–7.
The Organ Procurement and Transplantation Network; Data. In: Editor (ed)^(eds) Book The Organ Procurement and Transplantation Network; Data. OPTN, City, pp.
Beecher H. A definition of irreversible coma. Report of the Ad Hoc Committee of the Harvard Medical School to examine the definition of brain death. JAMA. 1968;205:337–40.
Novitzsky D. Detrimental effects of brain death on the potential organ donor. Transplant Proc. 1997;29:3770–2.
Vienenkoetter D, Esmaeilzadeh M, Unterberg A, Ahmadi R. Critical care management of potential organ donors: our current standard. Clin Transplant. 2009;23:2–9.
Non heart-beating organ transplantation: Practice and Protocols. In: Editor (ed)^(eds) Book Non heart-beating organ transplantation: Practice and Protocols. Institute of Medicine, City, pp. 174
Bernat J, D’Alessandro A, Port F, Bleck T, Heard S, Medina J, et al. Report of a national conference on donation after cardiac death. Am J Transplant. 2006;6:281–91.
Reich D, Mulligan P, Pruett T, Abecassis M, D’Alessandro A, Pomfret E, et al. ASTS recommended practice guidelines for controlled donation after cardiac death organ procurement and transplantation. Am J Transplant. 2009;9:2004–11.
Sanchez-Fructosis A, Prats D, Torrente J, Perez-Contin M, Fernandez C, Alvarez J, et al. Renal transplantation from non-heart beating donors: a promising alternative to enlarge the donor pool. J Am Soc Nephrol. 2000;11:350–8.
Kootstra G, Daemen J, Oomen A. Categories of non-heart-beating donors. Transplant Proc. 1995;27:2893–4.
Wilhelm M, Pratschke J, Laskowski I, Paz D, Tilney N. Brain death and its impact on the donor heart - lessons from animal models. J Heart Lung Transplant. 2000;19:414–8.
Shivalker B, van Loon J, Wieland W, Tjandra-Maga T, Borgers M, Plets C, et al. Variable effects of explosive or gradual increase of intracranial pressure on myocardial structure and function. Circulation. 1993;87:230–9.
Novitzsky D, Horak A, Cooper D, Rose A. Electrocardiographic and histopathologic changes developing during experimental brain death in the baboon. Transplant Proc. 1989;21:2567–9.
Novitzsky D, Wicomb W, Cooper D. Electrocardiographic, haemodynamic and endocrine changes occurring during experimental brain death in the Chacma baboon. J Heart Transplant. 1984;4:63.
Power B, van Heerden P. The physiological changes associated with brain death - current concepts and implications for treatment of the brain dead donor. Anaesth Intensive Care. 1995;23:26–36.
Wood K, Becker B, McCartney J, D’Alessandro A, Coursin D. Care of the potential organ donor. NEJM. 2004;351:2730–9.
Wheeldon D, Potter C, Oduro A, Wallwork J, Large S. Transforming the “unacceptable” donor: outcomes from adoption of a standardized donor management technique. J Heart Lung Transplant. 1995;14:734–42.
Kutsogiannis D, Pagliarello G, Doig C, Ross H, Shemie S. Medical management to optimize donor organ potential: review of the literature. Can J Anesth. 2006;53:820–30.
Schnuelle P, Berger S, de Boer J, Persijn G, van der Woude F. Effects of catelcholamine application to brain-dead donors on graft survival in solid organ transplantation. Transplantation. 2001;72:455–63.
Debaveye Y, van de Berghe G. Is there still a place for dopamine in the modern intensive care unit? Anaesth Analg. 2004;98:461–8.
Finfer S, Bohn D, Colpitts D, Cox P, Fleming F, Barker G. Intensive care management of paediatric donor organs and its effect on post-transplant organ function. Intensive Care Med. 1996;22:1424–32.
Koning O, Ploeg R, van Bockel J, Groenewegen M, van der Woude F, Persijn G, et al. Risk factors for delayed graft function in cadaveric kidney transplantation: a prospective study of renal function and graft survival after preservation with University of Wisconsin solution in multi-organ donors. Transplantation. 1997;63:1620–8.
•• Franklin G, Santos A, Smith J, Galbraith S, Harbrecht B, Garrison R, (2010) Optimization of Donor Management Goals yields increased organ use. The American Surgeon 76. The first data from a UNOS series prospectively evaluating the use of DMGs as end points for resuscitation in the organ donor. Provides interesting insight into which standard goals may be necessary for optimal organ use, namely PaO 2 , inotrope use, and glucose control, and which appear to have no effect. The full multiregional results evaluating the development and use of DMGs are awaited.
Katz K, Lawler J, Wax J, O’Connor R, Nadkarni V. Vasopressin pressor effects in critically ill children during evaluation for brain death and organ recovery. Resuscitation. 2000;47:33–40.
Pennefether S, Bullock R, Mantle D, Dark J. Use of low dose arginine vasopressin to support brain-dead organ donors. Transplantation. 1995;59:58–62.
Hunt S, Baldwin J, Baumgartner W, Bricker J, Costanzo M, Miller L, et al. Cardiovascular management of a potential heart donor: a statement from the Transplantation Committee of the American College of Cardiology. Crit Care Med. 1996;24:1599–601.
Iwai A, Sakano T, Uenishi M, Sugimoto H, Yoshioko T, Sugimoto T. Effect of vasopressin and catecholamines on the maintenance of stability in brain dead patients. Transplantation. 1989;48:613–7.
Van Raemdonck D, Neyrinck A, Verleden G, Dupont L, Coosemans W, Decauwe H. Lung donor selection and management. Proc Am Thorac Soc. 2009;6:28–38.
Hornby K, Ross H, Keshavjee S, Rao V, Shemie S. Non-utilisation of hearts and lungs after consent for donation: a Canadian multi-centre study. Can J Anaesth. 2006;53:831–7.
Angel L, Levine D, Restrepo M, Johnson S, Sako E, Carpenter A, et al. Impact of a lung transplantation donor-management protocol on lung donation and recipient outcomes. Am J Respir Crit Care Med. 2006;174:710–6.
• Mascia L, Pasero D, Slutsky A, Arguis M, Grasso S, Munari M, Boifava S, Cornara G, Della Corte F, Vivaldi N, Malacarne P, Del Gaudio P, Livigni S, Zavala E, Filippini C, Martin E, Donadio P, Mastromauro I, Ranieri V, (2010) Effect of a lung protective strategy for organ donors on eligibility and availability of lungs for transplantation. JAMA 304: 2620–2627. Lungs remain one of the most difficult organs to maintain donation potential in after brainstem death. This multicenter RCT demonstrates that institution of a lung-protective ventilatory strategy in potential organ donors significantly increased the number of eligible and transplanted lungs compared to conventional ventilatory strategies.
Bittner H, Kendall S, Chen E, Craig D, Van Trigt P. The effects of brain death on cardiopulmonary hemodynamics and pulmonary bloodflow characteristics. Chest. 1995;108:1358–63.
Novitzsky D, Wicomb W, Rose A, Cooper D, Reichart B. Pathophysiology of pulmonary oedema following experimental brain death in the Chacma baboon. Ann Thorac Surg. 1987;43:288–94.
van der Zee H, Malik A, Lee B, Hakim T. Lung fluid and protein exchange during intracranial hypertension and role of sympathetic mechanisms. Ann Thorac Surg. 1987;48:273–80.
Fisher A, Donnelly S, Hirani N, Burdick M, Strieter R, Dark J, et al. Enhanced pulmonary inflammation in organ donors following fatal non-traumatic brain injury. Lancet. 1999;353:1412–3.
Fisher A, Donelly S, Hirani N, Haslett C, Strieter R, Dark J, et al. Elevated levels of interleukin-8 in donor lungs is associated with early graft failure after lung transplantation. Am J Respir Crit Care Med. 2001;163:259–65.
Neyrinck A, Van de Wauwer C, Geudens N, Rega F, Verleden G, Wouters P, et al. Comparative study of donor lung injury in heart-beating versus non-heart beating donors. Eur J Cardiothorac Surg. 2006;30:628–36.
Kang C, Anraku M, Cypel M, Sato M, Yeung J, Gharib S, et al. Transcriptional signatures in donor lungs from donation after cardiac death vs after brain death: a functional pathway analysis. J Heart Lung Transplant. 2011;30:289–98.
Avlonitis V, Fisher A, Kirby J, Dark J. Pulmonary transplantation: the role of brain death in donor lung injury. Transplantation. 2003;75:1928–33.
Gabbay E, Williams T, Griffiths A, Macfarlane L, Kotsimbos T, Esmore D, et al. Maximising the utilization of donor organs offered for lung transplantation. Am J Resp Crit Care Med. 1999;160:265–71.
Mascia L, Bosma K, Pasero D, Galli T, Cortese G, Donadio P, et al. Ventilatory and hemodynamic management of potential organ donors: an observational study. Crit Care Med. 2006;34:321–7.
Botha P, Rostron A, Fisher A, Dark J. Current strategies in donor selection and management. Semin Thorac Cardiovasc Surg. 2008;20:143–51.
Noiseux N, Nguyen B, Marsolais P, Dupont J, Simard L, Houde I, et al. Pulmonary recruitment protocol for organ donors: a new strategy to improve rate of lung utilisation. Transplant Proc. 2009;41:3284–9.
Ware L, Fang X, Wang Y, Sakuma T, Hall T, Matthay M. Selected contribution: mechanisms that may stimulate the resolution of alveolar edema in the transplanted human lung. J Appl Physiol. 2002;93:1869–74.
Neyrinck A, Rega F, Fransen L, De Winter H, Jannis N, Wouters P, et al. b-adrenergic stimulation of alveolar liquid clearance: a novel strategy to resolve pulmonary edema after lung transplantation? (Abstract). Eur J Anaesthesiol. 2004;21:A664.
• Ware L, Koyama T, Billheimer D, Landeck M, Johnson E, Brady S, Bernard G, Matthay M, (2011) Advancing donor management research: design and implentation of a large, randomized, placebo-controlled trial. Annals of Intensive Care 1. Evaluates the logistical challenges of conducting RCTs in the setting of organ donor management, based on the group’s personal experiences with instigating one of the few placebo-controlled RCTs in this field. Given the need to improve the quality of evidence pertaining to the management of the potential organ donor this is an important paper both for investigators planning future clinical trials in the brain-dead donor population and for intensivists who are involved in the care of the brain-dead organ donors and in the design and conduct of research in this field.
Folkesson H, Norlin A, Wang Y, Abedinpour P, Matthay M. Dexamethasone and thyroid hormone pre-treatment upregulate alveloar epithelial fluid clearance in adult rats. J Appl Physiol. 2000;88:416–24.
Mukadam M, Harrington D, Wilson I, Mascaro J, Rooney S, Thompson R, et al. Does donor catelcholamine administration effect early lung function after transplantation? J Thorac Cardiovasc Surg. 2005;130:926–7.
Cooper D, Novitzsky D, Wicomb W. The pathophysiological effects of brain death on potential donor organs, with particular reference to the heart. Ann R Coll Surg Engl. 1989;71:261–6.
Wicomb W, Cooper D, Lanza R, Novitzsky D, Isaacs S. Storage by hypothermic perfusion on donor heart function in the pig. J Thorac Cardiovasc Surg. 1986;91:896–909.
Dictus C, Vienenkoetter B, Esmaeilzadeh M, Unterberg A, Ahmadi R. Critical care management of potential organ donors: our current standard. Clin Transplant. 2009;23:2–9.
Novitzsky D, Cooper D, Rosendale J, Kauffman H. Hormonal therapy of the brain-dead organ donor: experimental and clinical studies. Transplantation. 2006;82:1396–401.
Rosendale J, Kauffman H, McBride M, Chabalewski F, Zaroff J, Garrity E, et al. Hormonal resuscitation yields more transplanted hearts with improved early function. Transplantation. 2003;75:1336–8.
Holmes C, Patel B, Russell J, Walley K. Physiology of vasopressin relevant to management of septic shock. Chest. 2001;120:989–1002.
Figueras J, Busquets J, Grande L, Jaurrieta E, Perez-Ferreiroa J, Mir J, et al. The deleterious effect of donor high plasma sodium and extended preservation in liver transplantation. A multivariate analysis. Transplantation. 1996;61:410–3.
Avolio A, Agnes S, Magalini S, Foco M, Castagneto M. Importance of donor blood chemistry data (AST, serum sodium) in predicting liver transplant outcome. Transplant Proc. 1991;23:2451–2.
Gonzalez F, Rimmola A, Grande L, Antolin M, Garcia-Valdecasas J, Fuster J, et al. Predictive factors of early postoperative graft function in human liver transplantation. Hepatology. 1994;20:565–73.
Totsuka E, Dodson F, Urakami A, Moras N, Ishii T, Lee M, et al. Influence of high donor serum sodium levels on early postoperative graft function in human liver transplantation: effect of correction of donor hypernatremia. Liver Transpl Surg. 1999;5:421–8.
Mangus R, Fridell J, Vianna R, Milgrom M, Chestovich P, Vandenboom C, et al. Severe hypernatremia in deceased liver donors does not impact early transplant outcome. Transplantation. 2010;90:438–43.
Tector A, Mangus R, Chestovich P, Vianna R, Fridell J, Milgrom M, et al. Use of extended criteria livers decrease wait time for liver transplantation without adversely impacting posttransplant survival. Ann Surg. 2006;244:439–50.
Tekin K, Imber C, Atli M, Gunson B, Bramhall S, Mayer D, et al. A simple scoring system to evaluate the effects of cold ischemia on marginal liver donors. Transplantation. 2004;77:411–6.
Renz J, Kin C, Kinkhabwala M, Jan D, Varadarajan R, Goldstein M, et al. Utilization of extended donor criteria liver allografts maximises donor use and patient access to liver transplantation. Ann Surg. 2005;242:556–63.
Rosendale J, Kauffman H, McBride M, Chabalewski F, Zaroff J, Garrity E, et al. Aggressive pharmacological donor management results in more transplanted organs. Transplantation. 2003;75:482–7.
Masson F, Thicoipe M, Gin H, De Mascarela A, Angibeau R, Favarel-Garrigues J, et al. The endocrine pancreas in brain-dead donors. Transplantation. 1993;56:363–7.
Gores P, Gillingham K, Dunn D, Moudry-Munns K, Najarian J, Sutherland D. Donor hyperglycaemia as a minor risk factor and immunologic variables as major risk factors for pancreas allograft loss in a multivariate analysis of a single institution’s experience. Ann Surg. 1992;215:217–30.
Smith M. Physiologic changes during brainstem death: lessons for management of the organ donor. J Heart Lung Transplant. 2004;23:S217–22.
Cipolla J, Stawicki S, Spatz D. Haemodynamic monitoring of organ donors: a novel use of the oesophageal echo-Doppler probe. Am Surg. 2006;72:500–4.
Uchino S, Bellomo R, Morimatsu H, Sugihara M, French C, Stephens D, et al. Pulmonary artery catheter versus pulse contour analysis: a prospective epidemiological study. Crit Care. 2006;10:R174.
Jenkins D, Reilly P, Schwab C. Improving the approach to organ donation: a review. World J Surg. 1999;23:644–9.
Lopez-Navidad A, Caballero F. For a rational approach to the critical points of the cadaveric donation process. Transplant Proc. 2001;33:795–805.
Grossman M, Reilly P, McMahon D, (1996) Loss of potential organ donors due to medical failure. Crit Care Med 24
Hagan M, McClean D, Falcone C, Arrington J, Matthews D, Summe C. Attaining specific donor management goals increases number of organs transplanted per donor: a quality improvement project. Prog Transplant. 2009;19:227–31.
Santisea G, D’Anconaa G, Fallettab C, Pironea F, Sciaccaa S, Turrisia M, et al. Donor pharmacological hemodynamic support is associated with primary graft failure in human heart transplantation. Interact Cardiovasc Thorac Surg. 2009;9:476–9.
Reilly P, Morgan L, Grossman M, Shapiro M, Anderson H, Hawthorne R, Schwab C, Lung procurement from solid organ donors: role of fluid resuscitation in procurement failures. The Internet Journal of Emergency and Intensive Care Medicine. 1999;3
Kunzendorf U, Hohenstein B, Oberbarnscheid M, Muller E, Renders L, Schott G, et al. Duration of donor brain death and its influence on kidney graft function. Am J Transplant. 2002;2:292–4.
Lopez-Navidad A, Domingo P, Caballero F. Organ shortage: viability of potential organ donors and possible loss depend on health care workers who are responsible for the organ procurement program. Transplant Proc. 1997;29:3614–6.
•• Kootstra G (2009) History of non-heart beating donation. In: Talbot D, D’Alessandro A (eds) Organ donation and transplantation after cardiac death. Oxford University Press, Oxford. Written by a team of international experts, this book provides a detailed and comprehensive overview of both the basic science and the clinical evidence currently available that has underpinned the development of DCD protocols in the UK and Europe. It also provides an outline of the moral, legal, and ethical considerations in the development of DCD programs. It is probably the most considered and authorative overview of DCD to date.
Shemie S, De Vita M. Legal, moral and ethical issues. In: Talbot D, D’Alessandro A, editors. Organ donation and transplantation after cardiac death. Oxford: Oxford University Press; 2009.
Ethics Committee, American College of Critical Care Medicine; Society of Critical Care Medicine. Recommendations for nonheart-beating organ donation. A position paper by the Ethics Committee, American College of Critical Care Medicine, Society of Critical Care Medicine. Crit Care Med. 2001;29:1826–31.
United Network of Organ Sharing. Donation after cardiac death; A reference guide. UNOS, Richmond, VA
Rubenstein S, (2008) Caifornia surgeon cleared of hastening organ donor’s death. The Wall Street J
Lewis J, Peltier J, Nelson H, Snyder W, Schneider K, Steinberger D, et al. Development of th University of Wisconsin donation after cardiac death evaluation tool. Prog Transplant. 2003;13:265–73.
Lee K, Simpkins C, Montgomery R, Locke J, Segev D, Maley W. Factors affecting graft survival after liver transplantation from donation after cardiac death donors. Transplantation. 2006;82:1683–8.
Fernandez L, Di Carlo A, Odorico J, Leverson G, Shames B, Becker Y, et al. Simultaneous pancreas-kidney transplantation from donation after cardiac death: successful long term outcomes. Ann Surg. 2005;242:732–8.
DeVita M, Brooks M, Zawistowski C, Rudich S, Daly B, Chaitin E. Donors after Cardiac Death: Validation of identification Criteria (DVIC) study for predictors of rapid death. Am J Transp. 2008;8:432–41.
Herdman R, Beauchamp T, Potts J. The Institute of Medicine’s report on non-heart beating organ transplantation. Kennedy Inst Ethics. 1998;8:83–90.
Casavilla A, Ramirez CS R, Nghiem D, Miracle J, Fung J, Starzl T. Experience with liver and kidney allografts from non heart beating donors. Transplant Proc. 1995;27:2898.
Veatch R. Transplantation Ethics. Washington: Georgetown University Press; 2000.
Koffman G, Gambaro G. Renal transplantation from non-heart beating donors: a review of the European experience. J Nephrol. 2003;16:334–41.
Shemie S, Baker A, Knoll G, Wall W, Rocker G, Howes D. Donation after cardiocirculatory death in Canada. CMAJ. 2006;175:S1–S24.
Organ donation: opportunities for action. In: Editor (ed)^(eds) Book Organ donation: opportunities for action. Institution of Medicine, City, pp. 358
Punch J (2009) Extracorporeal circulatory-assisted non heart beating organ donation. In: Talbot D, D'Alessandro A (eds) Organ donation and transplantation after cardiac death. Oxford University Press
Magliocca J, Magee J, Rowe S, Gravel M, Chenault R, Merion R, et al. Extracorporeal support for organ donation after cardiac death effectively expands the donor pool. J Trauma. 2005;58:1095–102.
Ko W, Chen Y, Tsai P, Lee P. Extracorporeal membrane oxygenation support of donor abdominal organs in non-heart beating donors. Clin Transplant. 2000;14:152–6.
Gravel M, Arenas J, Chenault R, Magee J, Rudich S, Maraschio M, et al. Kidney transplantation from organ donors following cardiopulmonary death using extracorporeal membrane oxygenation support. Am J Transplant. 2004;9:57–8.
Fondevila C, Hessheimer A, Ruiz A, Calatayud D, Ferrer J, Charco R, et al. Liver transplant using donors after unexpected cardiac death: Novel preservation protocol and acceptance criteria. Am J Transplant. 2007;7:1849–55.
• Bernat J, Capron A, Bleck T, Blosser S, Bratton S, Childress J, DeVita M, Fulda G, Gries C, Mathur M, Nakagawa T, Rushton C, Shemie S, White D, (2010) The circulatory-respiratory determination of death in organ donation. Crit Care Med 38: 963–970. This paper represents the report of an interdisciplinary panel convened by the Health Resources and Services Administration, Division of Transplantation in the US, on the role and means of death determination using circulatory-repsiratory tests, with particular reference to the use of postmortem ECMO to support donor organs and the transplantation of hearts. This report outlines many of the key ethical and technical issues and controversies associated with advancing management of the DCD donor.
Disclosure
Conflicts of interest: A.J. Dare; none; A. Bartlett: none; J. Fraser: has received a competitive grant from Cellsept (to study the effect of endothelin antagonist); and he is the medical director of BiVACOR, a totally artificial heart (this is still in the animal stages).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dare, A.J., Bartlett, A.S. & Fraser, J.F. Critical Care of the Potential Organ Donor. Curr Neurol Neurosci Rep 12, 456–465 (2012). https://doi.org/10.1007/s11910-012-0272-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11910-012-0272-9