Abstract
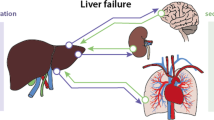
The critical care management of cirrhotic patients involves a multidisciplinary team approach, including the hepatologist and intensivist, to address life-threatening complications and to provide comprehensive care for multi-organ failure commonly seen in these patients. A systematic approach to the diagnosis and therapy of multi-organ system dysfunction is essential to optimize the intensive care management of these complex patients, with a goal to stabilize them for possible liver transplantation. This review provides a system-based approach for the intensive care management of critically ill cirrhotic patients.
Similar content being viewed by others
Abbreviations
- AMS:
-
Altered mental status
- HE:
-
Hepatic encephalopathy
- SBP:
-
Spontaneous bacterial peritonitis
- HRS:
-
Hepatorenal syndrome
- HPS:
-
Hepatopulmonary syndrome
- PPH:
-
Portopulmonary hypertension
- ACLF:
-
Acute on chronic renal failure
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Olson JC et al. Intensive care of the patient with cirrhosis. Hepatology. 2011;54(5):1864–72.
Karvellas CJ, Bagshaw SM. Advances in management and prognostication in critically ill cirrhotic patients. Curr Opin Crit Care. 2014;20(2):210–7.
Gines P et al. Management of critically-ill cirrhotic patients. J Hepatol. 2012;56 Suppl 1:S13–24.
Ford RM, Sakaria SS, Subramanian RM. Critical care management of patients before liver transplantation. Transplant Rev (Orlando). 2010;24(4):190–206.
Mullen KD et al. Rifaximin is safe and well tolerated for long-term maintenance of remission from overt hepatic encephalopathy. Clin Gastroenterol Hepatol. 2014;12(8):1390–1397 e2.
Bass NM et al. Rifaximin treatment in hepatic encephalopathy. N Engl J Med. 2010;362(12):1071–81.
Mas A et al. Comparison of rifaximin and lactitol in the treatment of acute hepatic encephalopathy: results of a randomized, double-blind, double-dummy, controlled clinical trial. J Hepatol. 2003;38(1):51–8.
Hassanein TI et al. Randomized controlled study of extracorporeal albumin dialysis for hepatic encephalopathy in advanced cirrhosis. Hepatology. 2007;46(6):1853–62.
Laleman W et al. Embolization of large spontaneous portosystemic shunts for refractory hepatic encephalopathy: a multicenter survey on safety and efficacy. Hepatology. 2013;57(6):2448–57.
Garcia-Tsao G et al. Portal pressure, presence of gastroesophageal varices and variceal bleeding. Hepatology. 1985;5(3):419–24.
Carbonell N et al. Improved survival after variceal bleeding in patients with cirrhosis over the past two decades. Hepatology. 2004;40(3):652–9.
Villanueva C et al. Transfusion strategies for acute upper gastrointestinal bleeding. N Engl J Med. 2013;368(1):11–21.
Bosch J et al. Recombinant factor VIIa for variceal bleeding in patients with advanced cirrhosis: a randomized, controlled trial. Hepatology. 2008;47(5):1604–14.
Theivanayagam S et al. Administration of erythromycin before endoscopy in upper gastrointestinal bleeding: a meta-analysis of randomized controlled trials. Saudi J Gastroenterol. 2013;19(5):205–10.
Levacher S et al. Early administration of terlipressin plus glyceryl trinitrate to control active upper gastrointestinal bleeding in cirrhotic patients. Lancet. 1995;346(8979):865–8.
Bernard B et al. Antibiotic prophylaxis for the prevention of bacterial infections in cirrhotic patients with gastrointestinal bleeding: a meta-analysis. Hepatology. 1999;29(6):1655–61.
Soares-Weiser K et al. Antibiotic prophylaxis of bacterial infections in cirrhotic inpatients: a meta-analysis of randomized controlled trials. Scand J Gastroenterol. 2003;38(2):193–200.
Garcia-Tsao G et al. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology. 2007;46(3):922–38.
Shaheen NJ et al. Pantoprazole reduces the size of postbanding ulcers after variceal band ligation: a randomized, controlled trial. Hepatology. 2005;41(3):588–94.
Boo GB et al. The effect of proton pump inhibitor on healing of post-esophageal variceal ligation ulcers. Korean J Gastroenterol. 2008;51(4):232–40.
de Franchis R. Evolving consensus in portal hypertension. Report of the Baveno IV consensus workshop on methodology of diagnosis and therapy in portal hypertension. J Hepatol. 2005;43(1):167–76.
Romero-Castro R et al. EUS-guided coil versus cyanoacrylate therapy for the treatment of gastric varices: a multicenter study (with videos). Gastrointest Endosc. 2013;78(5):711–21.
Procaccini NJ et al. Endoscopic cyanoacrylate versus transjugular intrahepatic portosystemic shunt for gastric variceal bleeding: a single-center U.S. analysis. Gastrointest Endosc. 2009;70(5):881–7.
Crisan D, Tantau M, Tantau A. Endoscopic management of bleeding gastric varices—an updated overview. Curr Gastroenterol Rep. 2014;16(10):413.
Garcia-Pagan JC et al. Use of early-TIPS for high-risk variceal bleeding: results of a post-RCT surveillance study. J Hepatol. 2013;58(1):45–50.
Garcia-Pagan JC et al. Early use of TIPS in patients with cirrhosis and variceal bleeding. N Engl J Med. 2010;362(25):2370–9.
Runyon BA, Committee APG. Management of adult patients with ascites due to cirrhosis: an update. Hepatology. 2009;49(6):2087–107.
Such J, Runyon BA. Spontaneous bacterial peritonitis. Clin Infect Dis. 1998;27(4):669–74. quiz 675–6.
Pleguezuelo M et al. Diagnosis and management of bacterial infections in decompensated cirrhosis. World J Hepatol. 2013;5(1):16–25.
Bellot P et al. Automated low flow pump system for the treatment of refractory ascites: a multi-center safety and efficacy study. J Hepatol. 2013;58(5):922–7.
Kwon JH et al. Mortality associated with proton pump inhibitors in cirrhotic patients with spontaneous bacterial peritonitis. J Gastroenterol Hepatol. 2014;29(4):775–81.
Serste T et al. Deleterious effects of beta-blockers on survival in patients with cirrhosis and refractory ascites. Hepatology. 2010;52(3):1017–22.
Mandorfer M et al. Nonselective beta blockers increase risk for hepatorenal syndrome and death in patients with cirrhosis and spontaneous bacterial peritonitis. Gastroenterology. 2014;146(7):1680–90 e1.
Gustot T et al. Severe sepsis in cirrhosis. Hepatology. 2009;50(6):2022–33.
Karvellas CJ et al. Bacteremia, acute physiology and chronic health evaluation II and modified end stage liver disease are independent predictors of mortality in critically ill nontransplanted patients with acute on chronic liver failure. Crit Care Med. 2010;38(1):121–6.
Bajaj JS et al. Second infections independently increase mortality in hospitalized patients with cirrhosis: the North American consortium for the study of end-stage liver disease (NACSELD) experience. Hepatology. 2012;56(6):2328–35. Prospective cohort study showed potentially preventable second infections are predictors of mortality independent of severity of cirrhosis.
Monnet X, Teboul J-L. Prediction of fluid responsiveness in patients with shock. Clin Pulm Med. 2014;21(6):282–7.
Rivers E et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345(19):1368–77.
Early Goal-Directed Therapy Collaborative Group of Zhejiang, P. The effect of early goal-directed therapy on treatment of critical patients with severe sepsis/septic shock: a multi-center, prospective, randomized, controlled study. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue 2010;22(6):331–4.
Moreau R et al. Abnormal tissue oxygenation in patients with cirrhosis and liver failure. J Hepatol. 1988;7(1):98–105.
Dellinger RP et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41(2):580–637.
Arabi YM et al. Antimicrobial therapeutic determinants of outcomes from septic shock among patients with cirrhosis. Hepatology. 2012;56(6):2305–15.
De Backer D et al. Comparison of dopamine and norepinephrine in the treatment of shock. N Engl J Med. 2010;362(9):779–89.
Acevedo J et al. Relative adrenal insufficiency in decompensated cirrhosis: relationship to short-term risk of severe sepsis, hepatorenal syndrome, and death. Hepatology. 2013;58(5):1757–65.
Moreau R et al. Septic shock in patients with cirrhosis: hemodynamic and metabolic characteristics and intensive care unit outcome. Crit Care Med. 1992;20(6):746–50.
Kor DJ, Gajic O. Blood product transfusion in the critical care setting. Curr Opin Crit Care. 2010;16(4):309–16.
Bianchini M, De Pietri L, Villa E. Coagulopathy in liver diseases: complication or therapy? Dig Dis. 2014;32(5):609–14.
Intagliata NM et al. Prophylactic anticoagulation for venous thromboembolism in hospitalized cirrhosis patients is not associated with high rates of gastrointestinal bleeding. Liver Int. 2014;34(1):26–32.
Yang ZJ et al. Venous thromboembolism in cirrhosis. Clin Appl Thromb Hemost. 2014;20(2):169–78.
Levesque E et al. Outcome of patients with cirrhosis requiring mechanical ventilation in ICU. J Hepatol. 2014;60(3):570–8.
Machicao VI, Balakrishnan M, Fallon MB. Pulmonary complications in chronic liver disease. Hepatology. 2014;59(4):1627–37.
Sharma P, Rakela J. Management of pre-liver transplantation patient—part 2. Liver Transpl. 2005;11(3):249–60.
Ramsay MA. Portopulmonary hypertension and hepatopulmonary syndrome, and liver transplantation. Int Anesthesiol Clin. 2006;44(3):69–82.
Talwalkar JA et al. Prevalence of spontaneous portosystemic shunts in patients with portopulmonary hypertension and effect on treatment. Gastroenterology. 2011;141(5):1673–9.
Colle IO et al. Diagnosis of portopulmonary hypertension in candidates for liver transplantation: a prospective study. Hepatology. 2003;37(2):401–9.
Wong F et al. New consensus definition of acute kidney injury accurately predicts 30-day mortality in patients with cirrhosis and infection. Gastroenterology. 2013;145(6):1280–8 e1. Consensus conference proposed definition for cirrhosis-associated acute kidney injury (AKI).
Barreto R et al. Type-1 hepatorenal syndrome associated with infections in cirrhosis: natural history, outcome of kidney function, and survival. Hepatology. 2014;59(4):1505–13. This prospective study shows two thirds of patients with HRS-1 associated with infections is irreversible.
European Association for the Study of the, L, European Association for the Study of the, L. EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. J Hepatol. 2010;53(3):397–417.
Banares R et al. Extracorporeal albumin dialysis with the molecular adsorbent recirculating system in acute-on-chronic liver failure: the RELIEF trial. Hepatology. 2013;57(3):1153–62.
Kwo PY. Management of hyponatremia in clinical hepatology practice. Curr Gastroenterol Rep. 2014;16(5):382.
Solà E, Graupera I, Ginès P. From refractory ascites to dilutional hyponatremia and hepatorenal syndrome: current options for treatment. Curr Hepatol Rep. 2014;1–9.
Ahluwalia V et al. Differential impact of hyponatremia and hepatic encephalopathy on health-related quality of life and brain metabolite abnormalities in cirrhosis. J Hepatol. 2013;59(3):467–73.
Gines P, Guevara M. Hyponatremia in cirrhosis: pathogenesis, clinical significance, and management. Hepatology. 2008;48(3):1002–10.
Jalan R et al. Albumin infusion for severe hyponatremia in patients with refractory ascites: a randomized clinical trial. J Hepatol. 2007;46:S95.
Davenport A. Acute renal replacement therapy. In: Harber M, editor. Practical nephrology. London: Springer; 2014. p. 75–90.
Asrani SK, O'Leary JG. Acute-on-chronic liver failure. Clin Liver Dis. 2014;18(3):561–74.
Jalan R et al. Bacterial infections in cirrhosis: a position statement based on the EASL Special Conference 2013. J Hepatol. 2014;60(6):1310–24.
Fernandez J et al. Prevalence and risk factors of infections by multiresistant bacteria in cirrhosis: a prospective study. Hepatology. 2012;55(5):1551–61.
Montano-Loza AJ. Clinical relevance of sarcopenia in patients with cirrhosis. World J Gastroenterol. 2014;20(25):8061–71.
Butterworth RF. Thiamine deficiency-related brain dysfunction in chronic liver failure. Metab Brain Dis. 2009;24(1):189–96.
Kribben A et al. Effects of fractionated plasma separation and adsorption on survival in patients with acute-on-chronic liver failure. Gastroenterology. 2012;142(4):782–789 e3.
Saliba F et al. Cirrhotic patients in the ICU: prognostic markers and outcome. Curr Opin Crit Care. 2013;19(2):154–60.
Cholongitas E et al. Prognostic models in cirrhotics admitted to intensive care units better predict outcome when assessed at 48 h after admission. J Gastroenterol Hepatol. 2008;23(8pt1):1223–7.
Moreau R., et al. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology. 2013;144(7):1426–37. 1437 e1-9. Data from cirrhotics with acute decompensation was utilized to define Acute on chronic liver failure as a distinct entity.
Compliance with Ethics Guidelines
Conflict of Interest
Sunil Dacha declares no conflict of interest.
Ram M. Subramanian is a consultant for Gambro-Baxter, Inc.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Management of the Cirrhotic Patient
Rights and permissions
About this article
Cite this article
Dacha, S., Subramanian, R.M. Critical Care Management in Cirrhosis. Curr Hepatology Rep 14, 60–68 (2015). https://doi.org/10.1007/s11901-015-0255-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11901-015-0255-9