Abstract
Osteolytic bone disease is the most common complication of multiple myeloma, resulting in skeletal-related events (SREs) that cause significant morbidity. Bone destruction in myeloma is due to an increased activity of osteoclasts coupled with suppressed bone formation by osteoblasts. Currently, bisphosphonates are the mainstay of the treatment of myeloma bone disease. Zoledronic acid and pamidronate have shown similar efficacy in reducing SREs in a randomized study in the conventional chemotherapy era. However, in a recent study (the Myeloma-IX trial of the UK Medical Research Council, MRC), zoledronic acid was found to be superior to clodronate in reducing SREs, but also it produced a survival advantage of approximately 10 months in patients with bone disease at baseline. During recent years, novel agents targeting bone have been used in myeloma. This review focuses on the established therapy of myeloma bone disease and also on recent advances in treatment that take advantage of the better understanding of the pathophysiology of bone disease.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Kyle RA, Gertz MA, Witzig TE, et al. Review of 1027 patients with newly diagnosed multiple myeloma. Mayo Clin Proc. 2003;78:21–33.
Christoulas D, Terpos E, Dimopoulos MA. Pathogenesis and management of myeloma bone disease. Expert Rev Hematol. 2009;2:385–98.
Terpos E, Szydlo R, Apperley JF, et al. Soluble receptor activator of nuclear factor kappaB ligand/osteoprotegerin ratio predicts survival in multiple myeloma: proposal for a novel prognostic index. Blood. 2003;102:1064–9.
Sugatani T, Alvarez UM, Hruska KA. Activin A stimulates IkappaB-alpha/NFkappaB and RANK expression for osteoclast differentiation, but not AKT survival pathway in osteoclast precursors. J Cell Biochem. 2003;90:59–67.
Gavriatopoulou M, Dimopoulos MA, Christoulas D, et al. Dickkopf-1: a suitable target for the management of myeloma bone disease. Expert Opin Ther Targets. 2009;13:839–48.
Gkotzamanidou M, Dimopoulos MA, Kastritis E, et al. Sclerostin: a possible target for the management of cancer-induced bone disease. Expert Opin Ther Targets. 2012;16:761–9.
Bruce NJ, McCloskey EV, Kanis JA, et al. Economic impact of using clodronate in the management of patients with multiple myeloma. Br J Haematol. 1999;104:358–64.
Cocks K, Cohen D, Wisløff F, et al. An international field study of the reliability and validity of a disease-specific questionnaire module (the QLQ-MY20) in assessing the quality of life of patients with multiple myeloma. Eur J Cancer. 2007;43:1670–8.
Saad F, Lipton A, Cook R, et al. Pathologic fractures correlate with reduced survival in patients with malignant bone disease. Cancer. 2007;110:1860–7.
Coleman RE. Bisphosphonates: clinical experience. Oncologist. 2004;9:14–27.
Belch AR, Bergsagel DE, Wilson K, et al. Effect of daily etidronate on the osteolysis of multiple myeloma. J Clin Oncol. 1991;9:1397–402.
Daragon A, Humez C, Michot C, et al. Treatment of multiple myeloma with etidronate: results of a multicentre double-blind study. Eur J Med. 1993;2:449–52.
Menssen HD, Sakalova A, Fontana A, et al. Effects of long-term intravenous ibandronate therapy on skeletal-related events, survival, and bone resorption markers in patients with advanced multiple myeloma. J Clin Oncol. 2002;20:2353–9.
Lahtinen R, Laakso M, Palva I, et al. Randomised, placebo-controlled multicentre trial of clodronate in multiple myeloma. Lancet. 1992;40:1049–52.
Laakso M, Lahtinen R, Virkkunen P, et al. Subgroup and cost-benefit analysis of the Finnish multicentre trial of clodronate in multiple myeloma. Br J Haematol. 1994;87:725–9.
McCloskey EV, MacLennan IC, Drayson MT, et al. A randomized trial of the effect of clodronate on skeletal morbidity in multiple myeloma. MRC Working Party on Leukaemia in Adults. Br J Haematol. 1998;100:317–25.
McCloskey EV, Dunn JA, Kanis JA, et al. Long-term follow-up of a prospective, double-blind, placebo-controlled randomized trial of clodronate in multiple myeloma. Br J Haematol. 2001;113:1035–43.
Berenson JR, Lichtenstein A, Porter L, et al. Efficacy of pamidronate in reducing skeletal events in patients with advanced multiple myeloma. Myeloma Aredia Study Group. N Engl J Med. 1996;334:488–93.
Berenson JR, Lichtenstein A, Porter L, et al. Long-term pamidronate treatment of advanced multiple myeloma patients reduces skeletal events. Myeloma Aredia Study Group. J Clin Oncol. 1998;16:593–602.
Brincker H, Westin J, Abildgaard N, et al. Failure of oral pamidronate to reduce skeletal morbidity in multiple myeloma: a double-blind placebo-controlled trial. Danish-Swedish co-operative study group Br J Haematol. 1998;101:280–6.
• Gimsing P, Carlson K, Turesson I, et al. Effect of pamidronate 30 mg versus 90 mg on physical function in patients with newly diagnosed multiple myeloma (Nordic Myeloma Study Group): a double-blind, randomised controlled trial. Lancet Oncol. 2010;11:973–82. The only randomized study which compared two different dosages of pamidronate in myeloma patients.
Berenson JR, Rosen LS, Howell A, et al. Zoledronic acid reduces skeletal-related events in patients with osteolytic metastases. Cancer. 2001;91:1191–200.
Rosen LS, Gordon D, Kaminski M, et al. Zoledronic acid versus pamidronate in the treatment of skeletal metastases in patients with breast cancer or osteolytic lesions of multiple myeloma: a phase III, double-blind, comparative trial. Cancer J. 2001;7:377–87.
Rosen LS, Gordon D, Kaminski M, et al. Long-term efficacy and safety of zoledronic acid compared with pamidronate disodium in the treatment of skeletal complications in patients with advanced multiple myeloma or breast carcinoma: a randomized, double-blind, multicenter, comparative trial. Cancer. 2003;98:1735–44.
•• Morgan GJ, Davies FE, Gregory WM, et al. First-line treatment with zoledronic acid as compared with clodronic acid in multiple myeloma (MRC Myeloma IX): a randomised controlled trial. Lancet. 2010;376:1989–99. The biggest randomized study in the field of bisphosphonates for the treatment of myeloma-related bone disease which compared oral clodronate and zoledronic acid. The study confirmed the superiority of zoledronic acid over clodronate not only regarding skeletal-related events but also regarding survival.
Morgan GJ, Child JA, Gregory WM, et al. Effects of zoledronic acid versus clodronic acid on skeletal morbidity in patients with newly diagnosed multiple myeloma (MRC Myeloma IX): secondary outcomes from a randomised controlled trial. Lancet Oncol. 2011;12:743–52.
•• Morgan GJ, Davies FE, Gregory WM, et al. Effects of induction and maintenance plus long-term bisphosphonates on bone disease in patients with multiple myeloma: MRC Myeloma IX trial. Blood. 2012;119:5374–83. The updated analysis of the reference 25 which showed that the beneficial effect of zoledronic acid over clodronate continues even after two years following initiation of bisphosphonate therapy.
Kyle RA, Yee GC, Somerfield MR, et al. American Society of Clinical Oncology 2007 clinical practice guideline update on the role of bisphosphonates in multiple myeloma. J Clin Oncol. 2007;25:2464–72.
•• Terpos E, Sezer O, Croucher PI, et al. The use of bisphosphonates in multiple myeloma: recommendations of an expert panel on behalf of the European Myeloma Network. Ann Oncol. 2009;20:1303–17. Recommendations of the European Myeloma Network for the tretament of myeloma-related bone disease.
Bamias A, Kastritis E, Bamia C, et al. Osteonecrosis of the jaw in cancer after treatment with bisphosphonates: incidence and risk factors. J Clin Oncol. 2005;23:8580–7.
Dimopoulos MA, Kastritis E, Anagnostopoulos A, et al. Osteonecrosis of the jaw in patients with multiple myeloma treated with bisphosphonates: evidence of increased risk after treatment with zoledronic acid. Haematologica. 2006;91:968–71.
Zervas K, Verrou E, Teleioudis Z, et al. Incidence, risk factors and management of osteonecrosis of the jaw in patients with multiple myeloma: a single-centre experience in 303 patients. Br J Haematol. 2006;134:620–3.
Badros A, Terpos E, Katodritou E, et al. Natural history of osteonecrosis of the jaw in patients with multiple myeloma. J Clin Oncol. 2008;26:5904–9.
•• Dimopoulos MA, Kastritis E, Bamia C, et al. Reduction of osteonecrosis of the jaw (ONJ) after implementation of preventive measures in patients with multiple myeloma treated with zoledronic acid. Ann Oncol. 2009;20:117–20. An important study which showed for the first time that the implementation of dental preventive measures reduces the incidence of ONJ in myeloma patients who receive bisphosphonates.
Montefusco V, Gay F, Spina F, et al. Antibiotic prophylaxis before dental procedures may reduce the incidence of osteonecrosis of the jaw in patients with multiple myeloma treated with bisphosphonates. Leuk Lymphoma. 2008;49:2156–62.
Migliorati CA, Casiglia J, Epstein J, et al. Managing the care of patients with bisphosphonate-associated osteonecrosis: an American Academy of Oral Medicine position paper. J Am Dent Assoc. 2005;136:1658–68.
Anderson KC, Alsina M, Bensinger W, et al. Multiple myeloma. Clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2007;5:118–47.
Harrouseau JL, Greil R, Kloke O. ESMO Guidelines Task Force. ESMO Minimum Clinical Recommendations for diagnosis, treatment and follow-up of multiple myeloma. Ann Oncol. 2005;16:45–7.
Lacy MQ, Dispenzieri A, Gertz MA, et al. Mayo clinic consensus statement for the use of bisphosphonates in multiple myeloma. Mayo Clin Proc. 2006;81:1047–53.
Durie BG. Use of bisphosphonates in multiple myeloma: IMWG response to Mayo Clinic consensus statement. Mayo Clin Proc. 2007;82:516–57.
Musto P, Petrucci MT, Bringhen S, et al. A multicenter, randomized clinical trial comparing zoledronic acid versus observation in patients with asymptomatic myeloma. Cancer. 2008;113:1588–95.
Corso A, Varettoni M, Zappasodi P, et al. A different schedule of zoledronic acid can reduce the risk of the osteonecrosis of the jaw in patients with multiple myeloma. Leukemia. 2007;21:1545–8.
Terpos E, Dimopoulos MA, Sezer O, et al. The use of biochemical markers of bone remodeling in multiple myeloma: a report of the International Myeloma Working Group. Leukemia. 2010;24:1700–12.
Yaccoby S, Pearse RN, Johnson CL, et al. Myeloma interacts with the bone marrow microenvironment to induce osteoclastogenesis and is dependent on osteoclast activity. Br J Haematol. 2002;116:278–90.
Vanderkerken K, De Leenheer E, Shipman C, et al. Recombinant osteoprotegerin decreases tumor burden and increases survival in a murine model of multiple myeloma. Cancer Res. 2003;63:287–9.
Kostenuik PJ, Nguyen HQ, McCabe J, et al. Denosumab, a fully human monoclonal antibody to RANKL, inhibits bone resorption and increases BMD in knock-in mice that express chimeric (murine/human) RANKL. J Bone Miner Res. 2009;24:182–95.
Henry DH, Costa L, Goldwasser F, et al. Randomized, double-blind study of denosumab versus zoledronic acid in the treatment of bone metastases in patients with advanced cancer (excluding breast and prostate cancer) or multiple myeloma. J Clin Oncol. 2011;29:1125–32.
Steinman RM, Bonifaz L, Fujii S, et al. The innate functions of dendritic cells in peripheral lymphoid tissues. Adv Exp Med Biol. 2005;560:83–97.
• Vallet S, Mukherjee S, Vaghela N, et al. Activin A promotes multiple myeloma-induced osteolysis and is a promising target for myeloma bone disease. Proc Natl Acad Sci U S A. 2010;107:5124–9. The first paper addressing the role of activin-A in myeloma-related bone disease.
Terpos E, Kastritis E, Christoulas D, et al. Circulating activin-A is elevated in patients with advanced multiple myeloma and correlates with extensive bone involvement and inferior survival; no alterations post-lenalidomide and dexamethasone therapy. Ann Oncol. Forthcoming 2012.
Pearsall SR, Canalis E, Cornwall-Brady M, et al. A soluble activin type IIA receptor induces bone formation and improves skeletal integrity. Proc Natl Acad Sci U S A. 2008;105:7082–7.
Tian E, Zhan F, Walker R, et al. The role of the Wnt-signaling antagonist DKK1 in the development of osteolytic lesions in multiple myeloma. N Engl J Med. 2003;349:2483–94.
Politou MC, Heath DJ, Rahemtulla A, et al. Serum concentrations of Dickkopf-1 protein are increased in patients with multiple myeloma and reduced after autologous stem cell transplantation. Int J Cancer. 2006;119:1728–31.
Terpos E, Christoulas D, Papatheodorou A, et al. Dickkopf-1 is elevated in newly-diagnosed, symptomatic patients and in relapsed patients with multiple myeloma. correlations with advanced disease features: a single-center experience in 284 patients [abstract]. Haematologica. 2010;95 Suppl 2:384.
Fulciniti M, Tassone P, Hideshima T, et al. Anti-DKK1 mAb (BHQ880) as a potential therapeutic agent for multiple myeloma. Blood. 2009;114:371–9.
Heath DJ, Chantry AD, Buckle CH, et al. Inhibiting dickkopf-1 (Dkk1) removes suppression of bone formation and prevents the development of osteolytic bone disease in multiple myeloma. J Bone Miner Res. 2009;24:425–36.
Loots GG, Kneissel M, Keller H, et al. Genomic deletion of a long-range bone enhancer misregulates sclerostin in Van Buchem disease. Genome Res. 2005;15:928–35.
Polyzos SA, Anastasilakis AD, Bratengeier C, et al. Serum sclerostin levels positively correlate with lumbar spinal bone mineral density in postmenopausal women – the six-month effect of risedronate and teriparatide. Osteoporos Int. 2012;23:1171–6.
Voskaridou E, Christoulas D, Plata E, et al. High circulating sclerostin is present in patients with thalassemia-associated osteoporosis and correlates with bone mineral density. Horm Metab Res. Forthcoming 2012.
• Terpos E, Christoulas D, Katodritou E, et al. Elevated circulating sclerostin correlates with advanced disease features and abnormal bone remodeling in symptomatic myeloma; reduction post-bortezomib monotherapy. Int J Cancer. 2012;131:1466–71. The first paper addressing the role of sclerostin in myeloma-related bone disease.
Lewiecki EM. Sclerostin: a novel target for intervention in the treatment of osteoporosis. Discov Med. 2011;12:263–73.
Terpos E, Heath DJ, Rahemtulla A, et al. Bortezomib reduces serum dickkopf-1 and receptor activator of nuclear factor-kappaB ligand concentrations and normalises indices of bone remodelling in patients with relapsed multiple myeloma. Br J Haematol. 2006;135:688–92.
Giuliani N, Morandi F, Tagliaferri S, et al. The proteasome inhibitor bortezomib affects osteoblast differentiation in vitro and in vivo in multiple myeloma patients. Blood. 2007;110:334–8.
Terpos E, Christoulas D, Kokkoris P, et al. Increased bone mineral density in a subset of patients with relapsed multiple myeloma who received the combination of bortezomib, dexamethasone and zoledronic acid. Ann Oncol. 2010;21:1561–2.
Terpos E, Kastritis E, Roussou M, et al. The combination of bortezomib, melphalan, dexamethasone and intermittent thalidomide is an effective regimen for relapsed/refractory myeloma and is associated with improvement of abnormal bone metabolism and angiogenesis. Leukemia. 2008;22:2247–56.
• Delforge M, Terpos E, Richardson PG, et al. Fewer bone disease events, improvement in bone remodeling, and evidence of bone healing with bortezomib plus melphalan-prednisone vs. melphalan-prednisone in the phase III VISTA trial in multiple myeloma. Eur J Haematol. 2011;86:372–84. The first randomized study confirming the beneficial effect of bortezomib on bone metabolism of myeloma patients who receive front-line therapy.
Zangari M, Aujay M, Zhan F, et al. Alkaline phosphatase variation during carfilzomib treatment is associated with best response in multiple myeloma patients. Eur J Haematol. 2011;86:484–7.
Hurchla MA, Garcia-Gomez A, Hornick MC, et al. The epoxyketone-based proteasome inhibitors carfilzomib and orally bioavailable oprozomib have anti-resorptive and bone-anabolic activity in addition to anti-myeloma effects. Leukemia. 2012. doi:10.1038/leu.2012.183.
Terpos E, Mihou D, Szydlo R, et al. The combination of intermediate doses of thalidomide with dexamethasone is an effective treatment for patients with refractory/relapsed multiple myeloma and normalizes abnormal bone remodeling, through the reduction of sRANKL/osteoprotegerin ratio. Leukemia. 2005;19:1969–76.
Tosi P, Zamagni E, Cellini C, et al. First-line therapy with thalidomide, dexamethasone and zoledronic acid decreases bone resorption markers in patients with multiple myeloma. Eur J Haematol. 2006;76:399–404.
Breitkreutz I, Raab MS, Vallet S, et al. Lenalidomide inhibits osteoclastogenesis, survival factors and bone-remodeling markers in multiple myeloma. Leukemia. 2008;22:1925–32.
Terpos E, Christoulas D, Katodritou E, et al. The combination of lenalidomide and dexamethasone (RD) reduces bone resorption in responding patients with relapsed/refractory multiple myeloma (MM) but has no effect on bone formation: results of a retrospective analysis and a prospective study on 205 patients, on behalf of the Greek myeloma study group [abstract]. Haematologica. 2011;96 Suppl 1:65.
Anderson G, Gries M, Kurihara N, et al. Thalidomide derivative CC-4047 inhibits osteoclast formation by down-regulation of PU.1. Blood. 2006;107:3098–105.
Balducci M, Chiesa S, Manfrida S, et al. Impact of radiotherapy on pain relief and recalcification in plasma cell neoplasms: long-term experience. Strahlenther Onkol. 2011;187:114–9.
Rades D, Veninga T, Stalpers LJ, et al. Outcome after radiotherapy alone for metastatic spinal cord compression in patients with oligometastases. J Clin Oncol. 2007;25:50–6.
Price P, Hoskin PJ, Easton D, et al. Prospective randomised trial of single and multifraction radiotherapy schedules in the treatment of painful bony metastases. Radiother Oncol. 1986;6:247–55.
•• Berenson J, Pflugmacher R, Jarzem P, et al. Balloon kyphoplasty versus non-surgical fracture management for treatment of painful vertebral body compression fractures in patients with cancer: a multicentre, randomised controlled trial. Lancet Oncol. 2011;12:225–35. The first randomized study revealing the value of balloon kyphoplasty for the treatment of painful vertebral fractures.
Bouza C, Lopez-Cuadrado T, Cediel P, et al. Balloon kyphoplasty in malignant spinal fractures: a systematic review and meta-analysis. BMC Palliat Care. 2009;8:12.
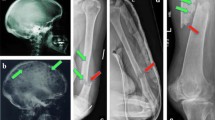
McDonald RJ, Trout AT, Gray LA, et al. Vertebroplasty in multiple myeloma: outcomes in a large patient series. AJNR Am J Neuroradiol. 2008;29:642–8.
Bhargava A, Trivedi D, Kalva L, et al. Management of cancer-related vertebral compression fracture: comparison of treatment options; a literature meta-analysis [abstract]. J Clin Oncol. 2009;27(Suppl:abstract):e20529.
Wedin R. Surgical treatment for pathologic fracture. Acta Orthop Scand Suupl. 2001;72(2p):1–29.
Utzschneider S, Schmidt H, Weber P, et al. Surgical therapy of skeletal complications in multiple myeloma. Int Orthop. 2011;35:1209–13.
Disclosure
E. Terpos: institutional grant from Janssen-Cilag, honoraria from Amgen, Novartis, Janssen-Cilag, and Onyx. E. Kastritis: none. M. Dimopoulos: honoraria from Novartis and Janssen-Cilag.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Terpos, E., Kastritis, E. & Dimopoulos, M.A. Prevention and Treatment of Myeloma Bone Disease. Curr Hematol Malig Rep 7, 249–257 (2012). https://doi.org/10.1007/s11899-012-0135-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11899-012-0135-0