Abstract
Purpose of Review
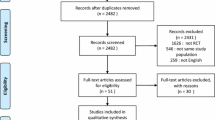
To analyze whether the use of morphine, as initial treatment in acute cardiogenic pulmonary edema (ACPE), has an impact in clinical outcomes and mortality. A systematic review of the literature was performed, including all the studies comparing clinical outcomes in patients with ACPE who were treated or not with morphine.
Recent Findings
Seven studies were selected, none of which were a randomized trial focused on answering the aim of this systematic review. The studies consisted of clinical trial secondary analysis assessing non-invasive ventilation in ACPE, one open non-randomized trial, two propensity score evaluations from large registries, and three clinical case reviews. Most of the studies showed unfavorable results with the use of morphine in terms of adverse events and mortality, and many of them were statistically significant. Finally, the ongoing MIdazolam versus MOrphine in acute cardiogenic pulmonary edema (MIMO) trial was specifically designed to compare the results of morphine use versus midazolam.
Summary
The potential hemodynamic and sedative benefit of the use of morphine for vasodilatation and dyspnea amelioration may be opposed by an increase in mortality, ICU admission, and adverse events. Until there is a randomized clinical trial, the use of morphine for ACPE should be limited.



Similar content being viewed by others
References
Gamero Donis D, Cebrián Patiño E, López C. Heart failure. Acute pulmonary oedema. In: Moya Mir MS, Piñera Salmerón P, Mariné Blanco M, editors. Tratado de Medicina de Urgencias, vol. Volumen 1. Madrid: Menarini. p. 516–31.
Cairns CB. Heart failure and pulmonary oedema. In: Tintinalli JE, Kelen GD, Stapczynski JS, editors. Medicina de urgencias. 6ª edit ed. Madrid: McGraw-Hill Interamericana de España; 2006. p. 425–9.
Hohman JS, Ingbar D. Cardiogenic shock and pulmonary oedema. In: Kasper DL, Braunwald E, Fauci AS, Hauser SL, Longo DL, Harrison LJJ, editors. Principles of internal medicine. 3ª ed. Madrid: Elsevier; 2006. p. 185–90.
Mosterd A, Hoes AW. Clinical epidemiology of heart failure. Heart. 2007;93:1137–46.
Redfield MM, Jacobsen SJ, Burnett JC, Mahoney DW, Bailey KR, Rodeheffer RJ. Burden of systolic and diastolic ventricular dysfunction in the community: appreciating the scope of the heart failure epidemic. JAMA. 2003;289:194–202.
Bleumink GS, Knetsch AM, Sturkenboom MCJM, Straus SMJM, Hofman A, Deckers JW, et al. Quantifying the heart failure epidemic: prevalence, incidence rate, lifetime risk and prognosis of heart failure: The Rotterdam Study. Eur Heart J England. 2004;25:1614–9.
Ceia F, Fonseca C, Mota T, Morais H, Matias F, De Sousa A, et al. Prevalence of chronic heart failure in Southwestern Europe: the EPICA study. Eur J Heart Fail. 2002;4:531–9.
Formiga F, Chivite D. Acute heart failure: understanding the patient is essential. Emergencias. 2018;30:145–6.
Llorens P. Risk assessment in emergency department patients with acute heart failure: we need to reach beyond our clinical judgment. Emergencias. 2018;30:75–6.
García-Gutiérrez S, Quintana López JM, Antón-Ladislao A, Gallardo Rebollal MS, Rilo Miranda I, Morillas Bueno M, et al. External validity of a prognostic score for acute heart failure based on the Epidemiology of Acute heart failure in Emergency Departments registry: the EAHFE-3D scale. Emergencias. 2018;30:84–90.
Llauger L, Jacob J, Corominas Lasalle G, Puig Martorell J, González Casquet P, Bullon Chia A. Renal insufficiency and hyperkalemia in acute heart failure. Emergencias. 2018;30:357–8.
Carratala JM, Díaz Lobato S, Brouzet B, Más-Serrano P, Espinosa B, Llorens P. Efficacy and safety of high-flow nasal cannula oxygen therapy in patients with acute heart failure. Emergencias. 2018;30:395–9.
Harjola P, Harjola VP. Can we do more for patients with acute heart failure before arrival at the hospital? Emergencias. 2017;29:221–2.
Miró O, Llorens P, Escalada X, Herrero P, Jacob J, Gil V, et al. Prehospital emergency care of patients with acute heart failure in Spain: the SEMICA study (emergency medical response systems for patients with acute heart failure). Emergencias. 2017;29:223–30.
Viejo-Moreno R, Hernández-Corral J, Campos-Espolio MC. Comments on the SEMICA study (emergency medical response systems for patients with acute heart failure). Emergencias. 2017;29:429–30.
Gerber Y, Weston SA, Redfield MM, Chamberlain AM, Manemann SM, Jiang R, et al. A contemporary appraisal of the heart failure epidemic in Olmsted County, Minnesota, 2000 to 2010. JAMA Intern Med. 2015;175:996–1004.
Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006;355:251–9.
Martín-Sánchez FJ, Rodríguez-Adrada E, Vidan MT, Díez Villanueva P, Llopis García G, González Del Castillo J, et al. Impact of geriatric assessment variables on 30-day mortality among older patients with acute heart failure. Emergencias. 2018;30:149–55.
González-Colaço Harmand M, Prada Arrondo PC, Domínguez Rodríguez A. Quality of life for elderly patients with acute heart failure: is it time to talk? Emergencias. 2018;30:363.
Aguirre Tejedo A, Miró O. Precipitating factors in acute heart failure: a review. Emergencias. 2017;29:185–93.
Llorens P, Escoda R, Miró O, et al. Characteristics and clinical course of patients with acute heart failure and the therapeutic measures applied in Spanish emergency departments: based on the EAHFE registry (epidemiology of acute heart failure in emergency departments). Emergencias. 2015;27:11–22.
Llorens P, Miró O, Martín-Sánchez FJ, Herrero-Puente P, Jacob-Rodríguez J, Gil V, et al. Guidelines for emergency management of acute heart failure: consensus of the Acute Heart Failure Working group of the Spanish Society of Emergency Medicine (AHF-SEMES) in 2011. Emergencias. 2011;23:119–39.
Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;18(8):891–975.
Spinar J, Parenica J, Vitovec J, Widimsky P, Linhart A, Fedorco M, et al. Baseline characteristics and hospital mortality in the Acute Heart Failure Database (AHEAD) main registry. Crit Care. 2011;15:R291.
Chioncel O, Vinereanu D, Datcu M, Ionescu DD, Capalneanu R, Brukner I, et al. The Romanian Acute Heart Failure Syndromes (ROAHFS) registry. Am Heart J. 2011;162:142–53.
Follath F, Yilmaz MB, Delgado JF, Parissis JT, Porcher R, Gayat E, et al. Clinical presentation, management and outcomes in the Acute Heart Failure Global Survey of Standard Treatment (ALARM-HF). Intensive Care Med. 2011;37:619–26.
Oliva F, Mortara A, Cacciatore G, Chinaglia A, Di Lenarda A, Gorini M, et al. IN-HF outcome investigators. Acute heart failure patient profiles, management and in-hospital outcome: results of the Italian registry on heart failure outcome. Eur J Heart Fail. 2012;14:1208–17.
Tavazzi L, Maggioni A, Lucci J, Cacciatore G, Ansalone G, Oliva F, et al. Nationwide survey on acute heart failure in cardiology ward services in Italy. Eur Heart J. 2006;27:1207–15.
Logeart D, Isnard R, Resche-Rigon M, Seronde MF, de Groote P, Jondeau G, et al. Current aspects of the spectrum of acute heart failure syndromes in a real-life setting: the OFICA study. Eur J Heart Fail. 2013;15:465–76.
Sosnowski MA. Review article: lack of effect of opiates in the treatment of acute cardiogenic pulmonary oedema. Emerg Med Australas. 2008;20(5):384–90.
Alison RC. Initial treatment of pulmonary edema: a physiological approach. Am J Med Sci. 1991;302(6):385–91.
Johnson MJ, McDonagh TA, Harkness A, McKay SE, Dargie HJ. Morphine for the relief of breathlessness in patients with chronic heart failure—a pilot study. Eur J Heart Fail. 2002;4(6):753–6.
Yancy CW, Jessup M, Bozkurt B, et al. 2016 ACC/AHA/HFSA focused update on new pharmacological therapy for heart failure: an update of the 2013ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J Am Coll Cardiol. 2016;22(9):659–69.
Hoffman JR, Reynolds S. Comparison of nitroglycerin, morphine and furosemide in treatment of presumed pre-hospital pulmonary edema. Chest. 1987;92(4):586–93.
Sacchetti A, Ramoska E, Moakes ME, McDermott P, Moyer V. Effect of ED management on ICU use in acute pulmonary edema. Am J Emerg Med. 1999;17(6):571–4.
Gray A, Goodacre S, Seah M, Tilley S. Diuretic, opiate and nitrate use in severe acidotic acute cardiogenic pulmonary oedema: analysis from the 3CPO trial. QJM. 2010;103(8):573–81.
Peacock WF, Hollander JE, Diercks DB, Lopatin M, Fonarow G, Emerman CL. Morphine and outcomes in acute decompensated heart failure: an ADHERE analysis. Emerg Med J. 2008;25(4):205–9.
Iakobishvili Z, Cohen E, Garty M, Behar S, Shotan A, Sandach A, et al. Use of intravenous morphine for acute decompensated heart failure in patients with and without acute coronary syndromes. Acute Card Care. 2011;13(2):76–80.
Dominguez-Rodriguez A, Avanzas P, Burillo-Putze G, Abreu-Gonzalez P. Influence of morphine treatment on in-hospital mortality amog patients with acute heart failure. Med Intensiva. 2017;41(6):382–4.
Miró Ò, Gil V, Martín-Sánchez FJ, Herrero-Puente P, Jacob J, Mebazaa A, et al. Morphine use in the ED and outcomes of patients with acute heart failure: a propensity score-matching analysis based on the EAHFE registry. Chest. 2017;152(4):821–32.
Dominguez-Rodriguez A, Burillo-Putze G, Garcia-Saiz MDM, Aldea-Perona A, Harmand MG, Mirò O, et al. Study design and rationale of “a multicenter, open-labeled, randomized controlled trial comparing MIdazolam versus MOrphine in acute pulmonary edema”: MIMO trial. Cardiovasc Drugs Ther. 2017;31(2):209–13.
Domínguez-Rodríguez A, Abreu-González P. Morphine for acute pulmonary edema? Emergencias. 2016;28:418–20.
Acknowledgments
This study was partially supported by grants from the Instituto de Salud Carlos III supported with funds from the Spanish Ministry of Health and FEDER (PI15/01019, PI15/00773, PI18/00393, PI19/00456) and Fundació La Marató de TV3 (2015/2510). The “Emergencies: Processes and Pathologies” research group of the IDIBAPS receives financial support from the Catalonian Government for Consolidated Groups of Investigation (GRC 2009/1385 and 2014/0313).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interests
VG, ADR, JM, and OM have no conflicts of interest to declare.
WFP declares receiving support from the following research grants: Abbott, Boehringer Ingelheim, Braincheck, CSL Behring, Daiichi-Sankyo, Immunarray, Janssen, Ortho Clinical Diagnostics, Portola, Relypsa, and Roche. He has served as a consultant in the following: Abbott, Astra-Zeneca, Bayer, Beckman, Boehringer-Ingelheim, Ischemia Care, Dx, Immunarray, Instrument Labs, Janssen, Nabriva, Ortho Clinical Diagnostics, Relypsa, Roche, Quidel, and Siemens. He provided expert testimony to Johnson and Johnson. He also has stock/ownership interests in the following: AseptiScope Inc., Brainbox Inc., Comprehensive Research Associates LLC, Emergencies in Medicine LLC, and Ischemia DX LLC.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Emergency Medicine
Rights and permissions
About this article
Cite this article
Gil, V., Domínguez-Rodríguez, A., Masip, J. et al. Morphine Use in the Treatment of Acute Cardiogenic Pulmonary Edema and Its Effects on Patient Outcome: A Systematic Review. Curr Heart Fail Rep 16, 81–88 (2019). https://doi.org/10.1007/s11897-019-00427-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11897-019-00427-0