Abstract
Purpose of Review
The aim of this review is to summarize existing research investigating the use of sodium glucose cotransporter-2 (SGLT2) inhibitors in patients with type 1 diabetes mellitus (T1DM) while highlighting potential strategies to mitigate the risk of diabetic ketoacidosis (DKA).
Recent Findings
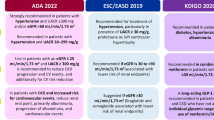
SGLT2 inhibitors have been studied in patients with T1DM in phase 3 clinical trials such as the inTandem, DEPICT, and EASE trials, which demonstrated consistent reductions in HbA1c. Secondary analyses of these trials have also reported potential kidney protective effects that are independent of improved glycemic control. However, trials in patients with type 2 diabetes mellitus (T2DM) have found an increased risk of DKA with SGLT2 inhibitors, a serious concern in patients with T1DM.
Summary
SGLT2 inhibitors provide cardiovascular benefits and kidney protection in patients with T2DM and are a promising therapeutic option for patients with T1DM due to overlapping pathophysiological mechanisms. However, SGLT2 inhibitors increase the risk of DKA, and there is currently a lack of research investigating the beneficial effects of SGLT2 inhibitors in patients with T1DM. Preventative measure for DKA would have to be implemented and the risks would need to be carefully balanced with the benefits offered by SGLT2 inhibitors. Additional research will also be required to determine the kidney protective effects of SGLT2 inhibitors in patients with T1DM and diabetic kidney disease and to quantify the risk of DKA after the implementation of preventative measures, proper patient education, and ketone monitoring.


Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Hirsch IB, Juneja R, Beals JM, Antalis CJ, Wright EE. The evolution of insulin and how it informs therapy and treatment choices. Endocr Rev. 2020;41(5):733–55.
Mobasseri M, Shirmohammadi M, Amiri T, Vahed N, Hosseini Fard H, Ghojazadeh M. Prevalence and incidence of type 1 diabetes in the world: a systematic review and meta-analysis. Health Promotion Perspectives. 2020;10(2):98–115.
Harjutsalo V, Thomas MC, Forsblom C, Groop PH. Risk of coronary artery disease and stroke according to sex and presence of diabetic nephropathy in type 1 diabetes. Diabetes Obes Metab. 2018;20(12):2759–67.
Hägg S, Thorn LM, Putaala J, Liebkind R, Harjutsalo V, Forsblom CM, et al. Incidence of stroke according to presence of diabetic nephropathy and severe diabetic retinopathy in patients with type 1 diabetes. Diabetes Care. 2013;36(12):4140–6.
Toschi E, Bailey RJ, Miller KM, Calhoun PM. Improvement in A1c levels in early adulthood in the T1D exchange: impact of racial, socioeconomic, and clinical factors. J Clin Endocrinol Metab. 2021;106(5):1294–302.
Foster NC, Beck RW, Miller KM, Clements MA, Rickels MR, DiMeglio LA, et al. State of Type 1 diabetes management and outcomes from the T1D exchange in 2016–2018. Diabetes Technol Ther. 2019;21(2):66–72.
Leoncini G, Viazzi F, De Cosmo S, Russo G, Fioretto P, Pontremoli R. Blood pressure reduction and RAAS inhibition in diabetic kidney disease: therapeutic potentials and limitations. J Nephrol. 2020;33(5):949–63.
Helve J, Sund R, Arffman M, Harjutsalo V, Groop P-H, Grönhagen-Riska C, et al. Incidence of end-stage renal disease in patients with type 1 diabetes. Diabetes Care. 2018;41(3):434–9.
Kristófi R, Bodegard J, Norhammar A, Thuresson M, Nathanson D, Nyström T, et al. Cardiovascular and renal disease burden in type 1 compared with type 2 diabetes: A Two-Country nationwide observational study. Diabetes Care. 2021;44(5):1211–8.
Costacou T, Orchard TJ. Cumulative kidney complication risk by 50 years of Type 1 diabetes: the effects of sex, age, and calendar year at onset. Diabetes Care. 2018;41(3):426–33.
Groop PH, Thomas MC, Moran JL, Wadèn J, Thorn LM, Mäkinen VP, et al. The presence and severity of chronic kidney disease predicts all-cause mortality in type 1 diabetes. Diabetes. 2009;58(7):1651–8.
Harjutsalo V, Forsblom C, Groop PH. Time trends in mortality in patients with type 1 diabetes: nationwide population based cohort study. BMJ. 2011;343:d5364.
Groop PH, Thomas M, Feodoroff M, Forsblom C, Harjutsalo V. Excess mortality in patients with type 1 diabetes without albuminuria-separating the contribution of early and late risks. Diabetes Care. 2018;41(4):748–54.
Heerspink HJ, Perkins BA, Fitchett DH, Husain M, Cherney DZ. Sodium glucose cotransporter 2 inhibitors in the treatment of diabetes mellitus: cardiovascular and kidney effects, potential mechanisms, and clinical applications. Circulation. 2016;134(10):752–72.
McMurray JJV, Solomon SD, Inzucchi SE, Køber L, Kosiborod MN, Martinez FA, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019;381(21):1995–2008.
Packer M, Anker SD, Butler J, Filippatos G, Pocock SJ, Carson P, et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. N Engl J Med. 2020;383(15):1413–24.
Heerspink HJL, Stefánsson BV, Correa-Rotter R, Chertow GM, Greene T, Hou F-F, et al. Dapagliflozin in patients with chronic kidney disease. N Engl J Med. 2020;383(15):1436–46. https://doi.org/10.1056/NEJMoa2024816.
Rosenstock J, Ferrannini E. Euglycemic diabetic ketoacidosis: A predictable, detectable, and preventable safety concern with SGLT2 inhibitors. Diabetes Care. 2015;38(9):1638–42.
Wolfsdorf JI, Ratner RE. SGLT inhibitors for type 1 diabetes: proceed with extreme caution. Diabetes Care. 2019;42(6):991–3.
Perkins BA, Rosenstock J, Skyler JS, Laffel LM, Cherney DZ, Mathieu C, et al. Exploring patient preferences for adjunct-to-insulin therapy in type 1 diabetes. Diabetes Care. 2019;42(9):1716–23.
Verma S, McMurray JJV, Cherney DZI. The metabolodiuretic promise of sodium-dependent glucose cotransporter 2 inhibition: The search for the sweet spot in heart failure. JAMA Cardiol. 2017;2(9):939–40.
Thomas MC, Cherney DZI. The actions of SGLT2 inhibitors on metabolism, renal function and blood pressure. Diabetologia. 2018;61(10):2098–107.
Cherney DZI, Cooper ME, Tikkanen I, Pfarr E, Johansen OE, Woerle HJ, et al. Pooled analysis of Phase III trials indicate contrasting influences of renal function on blood pressure, body weight, and HbA1c reductions with empagliflozin. Kidney Int. 2018;93(1):231–44.
Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373(22):2117–28.
Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019;380(4):347–57.
Neal B, Perkovic V, Mahaffey KW, De Zeeuw D, Fulcher G, Erondu N, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377(7):644–57.
Cannon CP, Pratley R, Dagogo-Jack S, Mancuso J, Huyck S, Masiukiewicz U, et al. Cardiovascular outcomes with ertugliflozin in type 2 diabetes. N Engl J Med. 2020;383(15):1425–35.
Cherney DZI, Charbonnel B, Cosentino F, Dagogo-Jack S, McGuire DK, Pratley R, et al. Effects of ertugliflozin on kidney composite outcomes, renal function and albuminuria in patients with type 2 diabetes mellitus: an analysis from the randomised VERTIS CV trial. Diabetologia. 2021;64(6):1256–67.
Bhatt DL, Szarek M, Pitt B, Cannon CP, Leiter LA, McGuire DK, et al. Sotagliflozin in patients with diabetes and chronic kidney disease. N Engl J Med. 2021;384(2):129–39.
Perkovic V, Jardine MJ, Neal B, Bompoint S, Heerspink HJL, Charytan DM, et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med. 2019;380(24):2295–306.
Heerspink HJL, Stefansson BV, Correa-Rotter R, Chertow GM, Greene T, Hou FF, et al. Dapagliflozin in patients with chronic kidney disease. N Engl J Med. 2020;383(15):1436–46.
Goldenberg RM, Gilbert JD, Hramiak IM, Woo VC, Zinman B. Sodium-glucose co-transporter inhibitors, their role in type 1 diabetes treatment and a risk mitigation strategy for preventing diabetic ketoacidosis: The STOP DKA Protocol. Diabetes Obes Metab. 2019;21(10):2192–202.
Garg SK, Peters AL, Buse JB, Danne T. Strategy for mitigating DKA risk in patients with type 1 diabetes on adjunctive treatment with SGLT inhibitors: A STICH protocol. Diabetes Technol Ther. 2018;20(9):571–5.
• Danne T, Garg S, Peters AL, Buse JB, Mathieu C, Pettus JH, et al. International Consensus on Risk Management of Diabetic Ketoacidosis in Patients With Type 1 Diabetes Treated With Sodium-Glucose Cotransporter (SGLT) Inhibitors. Diabetes Care. 2019;42(6):1147–54. This Consensus Report written by an international team of physicians and researchers with expertise in using SGLT2 inhibitor therapy. The report summarizes and reviews the current research regarding SGLT2 inhibitor use in addition to providing recommendations and strategies to enhance the safety (mitigating risk of DKA in particular) of SGLT2 inhibitors in individuals with type 1 diabetes.
Lam CSP, Karasik A, Melzer-Cohen C, Cavender MA, Kohsaka S, Norhammar A, et al. Association of sodium-glucose cotransporter-2 inhibitors with outcomes in type 2 diabetes with reduced and preserved left ventricular ejection fraction: Analysis from the CVD-REAL 2 study. Diabetes Obes Metab. 2021;20(6):1431–5.
Koh ES, Han K, Nam YS, Wittbrodt ET, Fenici P, Kosiborod MN, et al. Renal outcomes and all-cause death associated with sodium-glucose co-transporter-2 inhibitors versus other glucose-lowering drugs (CVD-REAL 3 Korea). Diabetes Obes Metab. 2021;23(2):455–66.
Kohsaka S, Lam CSP, Kim DJ, Cavender MA, Norhammar A, Jorgensen ME, et al. Risk of cardiovascular events and death associated with initiation of SGLT2 inhibitors compared with DPP-4 inhibitors: an analysis from the CVD-REAL 2 multinational cohort study. Lancet Diabetes Endocrinol. 2020;8(7):606–15.
Kohsaka S, Takeda M, Bodegard J, Thuresson M, Kosiborod M, Yajima T, et al. Sodium-glucose cotransporter 2 inhibitors compared with other glucose-lowering drugs in Japan: Subanalyses of the CVD-REAL 2 Study. J Diabetes Investig. 2021;12(1):67–73.
Cavender MA, Norhammar A, Birkeland KI, Jorgensen ME, Wilding JP, Khunti K, et al. SGLT-2 inhibitors and cardiovascular risk: An analysis of CVD-REAL. J Am Coll Cardiol. 2018;71(22):2497–506.
Kidney Disease: Improving Global Outcomes Diabetes Work G. KDIGO 2020 Clinical Practice Guideline for Diabetes Management in Chronic Kidney Disease. Kidney Int. 2020;98(4S):S1–S115.
Cherney DZ, Perkins BA, Soleymanlou N, Maione M, Lai V, Lee A, et al. Renal hemodynamic effect of sodium-glucose cotransporter 2 inhibition in patients with type 1 diabetes mellitus. Circulation. 2014;129(5):587–97.
Nathan DM, Cleary PA, Backlund JY, Genuth SM, Lachin JM, Orchard TJ, et al. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med. 2005;353(25):2643–53.
Zinman B. Glucose control in type 1 diabetes: from conventional to intensive therapy. Clin Cornerstone. 1998;1(3):29–38.
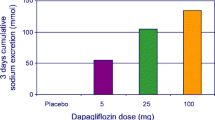
• Rosenstock J, Marquard J, Laffel LM, Neubacher D, Kaspers S, Cherney DZ, et al. Empagliflozin as adjunctive to insulin therapy in type 1 diabetes: The EASE trials. Diabetes Care. 2018;41(12):2560–9. The EASE trials were one of the three large RCTs investigating the use of SGLT2 inhibitors (empagliflozin in the EASE trials) as an adjunctive to insulin therapy in patients with type 1 diabetes. This trial found that empagliflozin improved glycemic control and weight without increasing hypoglycemia, and provides concrete evidence of the benfits SGLT2 inhibitors provide in patients with type 1 diabetes.
Buse JB, Garg SK, Rosenstock J, Bailey TS, Banks P, Bode BW, et al. Sotagliflozin in combination with optimized insulin therapy in adults with type 1 diabetes: The North American inTandem1 study. Diabetes Care. 2018;41(9):1970–80.
Garg SK, Henry RR, Banks P, Buse JB, Davies MJ, Fulcher GR, et al. Effects of sotagliflozin added to insulin in patients with type 1 diabetes. N Engl J Med. 2017;377(24):2337–48.
Phillip M, Mathieu C, Lind M, Araki E, di Bartolo P, Bergenstal R, et al. Long-term efficacy and safety of dapagliflozin in patients with inadequately controlled type 1 diabetes: pooled 52-week outcomes from the DEPICT-1 and -2 studies. Diabetes Obes Metab. 2021;23(2):549–60.
Vinovskis C, Li LP, Prasad P, Tommerdahl K, Pyle L, Nelson RG, et al. Relative hypoxia and early diabetic kidney disease in type 1 diabetes. Diabetes. 2020;69(12):2700–8.
van Raalte DH, Cherney DZI. Sodium glucose cotransporter 2 inhibition and renal ischemia: implications for future clinical trials. Kidney Int. 2018;94(3):459–62.
Korner A, Eklof AC, Celsi G, Aperia A. Increased renal metabolism in diabetes. Mechanism and functional implications. Diabetes. 1994;43(5):629–33.
O’Neill J, Fasching A, Pihl L, Patinha D, Franzén S, Palm F. Acute SGLT inhibition normalizes O2 tension in the renal cortex but causes hypoxia in the renal medulla in anaesthetized control and diabetic rats. Am J Physiol Renal Physiol. 2015;309(3):F227–34.
Layton AT, Vallon V, Edwards A. Modeling oxygen consumption in the proximal tubule: effects of NHE and SGLT2 inhibition. Am J Physiol Renal Physiol. 2015;308(12):F1343–57.
Layton AT, Vallon V, Edwards A. Predicted consequences of diabetes and SGLT inhibition on transport and oxygen consumption along a rat nephron. Am J Physiol Renal Physiol. 2016;310(11):ajprenal 00543.2015.
Tahara A, Takasu T. Prevention of progression of diabetic nephropathy by the SGLT2 inhibitor ipragliflozin in uninephrectomized type 2 diabetic mice. Eur J Pharmacol. 2018;830:68–75.
Woods TC, Satou R, Miyata K, Katsurada A, Dugas CM, Klingenberg NC, et al. Canagliflozin prevents intrarenal angiotensinogen augmentation and mitigates kidney injury and hypertension in mouse model of type 2 diabetes mellitus. Am J Nephrol. 2019;49(4):331–42.
Dekkers CCJ, Petrykiv S, Laverman GD, Cherney DZ, Gansevoort RT, Heerspink HJL. Effects of the SGLT-2 inhibitor dapagliflozin on glomerular and tubular injury markers. Diabetes Obes Metab. 2018;20(8):1988–93.
Cherney DZI, Zinman B, Inzucchi SE, Koitka-Weber A, Mattheus M, von Eynatten M, et al. Effects of empagliflozin on the urinary albumin-to-creatinine ratio in patients with type 2 diabetes and established cardiovascular disease: an exploratory analysis from the EMPA-REG OUTCOME randomised, placebo-controlled trial. Lancet Diabetes Endocrinol. 2017;5(8):610–21.
Cherney D, Lund SS, Perkins BA, Groop PH, Cooper ME, Kaspers S, et al. The effect of sodium glucose cotransporter 2 inhibition with empagliflozin on microalbuminuria and macroalbuminuria in patients with type 2 diabetes. Diabetologia. 2016;59(9):1860–70.
Abdel-Wahab AF, Bamagous GA, Al-Harizy RM, ElSawy NA, Shahzad N, Ibrahim IA, et al. Renal protective effect of SGLT2 inhibitor dapagliflozin alone and in combination with irbesartan in a rat model of diabetic nephropathy. Biomed Pharmacother. 2018;103:59–66.
Kopecky C, Lytvyn Y, Domenig O, Antlanger M, Kovarik JJ, Kaltenecker CC, et al. Molecular regulation of the renin-angiotensin system by sodium-glucose cotransporter 2 inhibition in type 1 diabetes mellitus. Diabetologia. 2019;62(6):1090–3.
Kojima N, Williams JM, Takahashi T, Miyata N, Roman RJ. Effects of a new SGLT2 inhibitor, luseogliflozin, on diabetic nephropathy in T2DN rats. J Pharmacol Exp Ther. 2013;345(3):464–72.
Laursen JC, Søndergaard-Heinrich N, De Melo JML, Haddock B, Rasmussen IKB, Safavimanesh F, et al. Acute effects of dapagliflozin on renal oxygenation and perfusion in type 1 diabetes with albuminuria: A randomised, double-blind, placebo-controlled crossover trial. EClinicalMedicine. 2021;37:100895.
Dekkers CCJ, Petrykiv S, Laverman GD, Cherney DZ, Gansevoort RT, Heerspink HJL. Effects of the SGLT-2 inhibitor dapagliflozin on glomerular and tubular injury markers. Diabetes Obes Metab. 2018;20(8):1988–93. https://doi.org/10.1111/dom.13301.
Heerspink HJL, Perco P, Mulder S, et al. Canagliflozin reduces inflammation and fibrosis biomarkers: a potential mechanism of action for beneficial effects of SGLT2 inhibitors in diabetic kidney disease. Diabetologia. 2019;62:1154–66. https://doi.org/10.1007/s00125-019-4859-4.
Opingari E, Verma S, Connelly KA, Mazer CD, Teoh H, Quan A, et al. The impact of empagliflozin on kidney injury molecule-1: a subanalysis of the effects of empagliflozin on cardiac structure, function, and circulating biomarkers in patients with type 2 diabetes CardioLink-6 trial. Nephrol Dial Transplant. 2020;35(5):895–7.
Lawler PR, Liu H, Frankfurter C, Lovblom LE, Lytvyn Y, Burger D, et al. Changes in cardiovascular biomarkers associated with the sodium-glucose cotransporter 2 (SGLT2) inhibitor ertugliflozin in patients with chronic kidney disease and type 2 diabetes. Diabetes Care. 2021;44(3):e45–7.
Kraus BJ, Weir MR, Bakris GL, Mattheus M, Cherney DZI, Sattar N, et al. Characterization and implications of the initial estimated glomerular filtration rate “dip” upon sodium-glucose co-transporter-2 inhibition with empagliflozin in the EMPA-REG OUTCOME trial. Kidney Int. 2021;99:750–62.
Iskander C, Cherney DZ, Clemens KK, Dixon SN, Harel Z, Jeyakumar N, et al. Use of sodium-glucose cotransporter-2 inhibitors and risk of acute kidney injury in older adults with diabetes: a population-based cohort study. CMAJ. 2020;192(14):E351–60.
Neuen BL, Young T, Heerspink HJL, Neal B, Perkovic V, Billot L, et al. SGLT2 inhibitors for the prevention of kidney failure in patients with type 2 diabetes: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2019;7(11):845–54.
Sridhar VS, Tuttle KR, Cherney DZI. We can finally stop worrying about SGLT2 inhibitors and acute kidney injury. Am J Kidney Dis. 2020;76(4):454–6.
Skrtic M, Cherney DZ. Sodium-glucose cotransporter-2 inhibition and the potential for renal protection in diabetic nephropathy. Curr Opin Nephrol Hypertens. 2015;24(1):96–103.
Scholtes RA, van Baar MJB, Lytvyn Y, Bjornstad P, Nieuwdorp M, Cherney DZI, et al. Sodium glucose cotransporter (SGLT)-2 inhibitors: do we need them for glucose-lowering, for cardiorenal protection or both? Diabetes Obes Metab. 2019;21:24–33.
Lytvyn Y, Bjornstad P, Katz A, Singh SK, Godoy LC, Chung LT, et al. SGLT2 inhibition increases serum copeptin in young adults with type 1 diabetes. Diabetes Metab. 2020;46(3):203–9.
Leon Jimenez D, Cherney DZI, Bjornstad P, Guerra LC, Miramontes Gonzalez JP. Antihyperglycemic agents as novel natriuretic therapies in diabetic kidney disease. Am J Physiol Renal Physiol. 2018;315(5):F1406–15.
Bjornstad P, Laffel L, Tamborlane WV, Simons G, Hantel S, von Eynatten M, et al. Acute effect of empagliflozin on fractional excretion of sodium and eGFR in youth with type 2 diabetes. Diabetes Care. 2018;41(8):e129–30.
Kidokoro K, Cherney DZI, Bozovic A, Nagasu H, Satoh M, Kanda E, et al. Evaluation of glomerular hemodynamic function by empagliflozin in diabetic mice using in vivo imaging. Circulation. 2019;23(140):303–15.
Vestri S, Okamoto MM, de Freitas HS, Aparecida Dos Santos R, Nunes MT, Morimatsu M, et al. Changes in sodium or glucose filtration rate modulate expression of glucose transporters in renal proximal tubular cells of rat. J Membr Biol. 2001;182(2):105–12.
Vallon V, Richter K, Blantz RC, Thomson S, Osswald H. Glomerular hyperfiltration in experimental diabetes mellitus: potential role of tubular reabsorption. J Am Soc Nephrol. 1999;10(12):2569–76.
Cherney DZI, Perkins BA, Soleymanlou N, Maione M, Lai V, Lee A, et al. Renal hemodynamic effect of sodium-glucose cotransporter 2 inhibition in patients with type 1 diabetes mellitus. Circulation. 2014;129(5):587–97.
van Bommel EJM, Muskiet MHA, van Baar MJB, Tonneijck L, Smits MM, Emanuel AL, et al. The renal hemodynamic effects of the SGLT2 inhibitor dapagliflozin are caused by post-glomerular vasodilatation rather than pre-glomerular vasoconstriction in metformin-treated patients with type 2 diabetes in the randomized, double-blind RED trial. Kidney Int. 2020;97(1):202–12.
Rajasekeran H, Lytvyn Y, Hladunewich M, Cattran D, Bozovic A, Perkins B, et al. The Effect of SGLT2 inhibition on urinary adenosine excretion in patients with type 1 diabetes. Can J Diabetes. 2016;40(5):S64.
Kidokoro K, Cherney DZI, Bozovic A, Nagasu H, Satoh M, Kanda E, et al. Evaluation of glomerular hemodynamic function by empagliflozin in diabetic mice using in vivo imaging. Circulation. 2019;140(4):303–15.
Cherney DZI, Dekkers CCJ, Barbour SJ, Cattran D, Abdul Gafor AH, Greasley PJ, et al. Effects of the SGLT2 inhibitor dapagliflozin on proteinuria in non-diabetic patients with chronic kidney disease (DIAMOND): a randomised, double-blind, crossover trial. Lancet Diabetes Endocrinol. 2020;8(7):582–93.
Rajasekeran H, Reich HN, Hladunewich MA, Cattran D, Lovshin JA, Lytvyn Y, et al. Dapagliflozin in focal segmental glomerulosclerosis: a combined human-rodent pilot study. Am J Physiol Renal Physiol. 2018;314(3):F412–22.
Cherney DZI, Charbonnel B, Cosentino F, Dagogo-Jack S, McGuire DK, Pratley R, et al. Effects of ertugliflozin on kidney composite outcomes, renal function and albuminuria in patients with type 2 diabetes mellitus: an analysis from the randomised VERTIS CV trial. Diabetologia. 2021;64(6):1256–67. https://doi.org/10.1007/s00125-021-05407-5.
Cherney DZI, Heerspink HJL, Frederich R, Maldonado M, Liu J, Pong A, et al. Effects of ertugliflozin on renal function over 104 weeks of treatment: a post hoc analysis of two randomised controlled trials. Diabetologia. 2020;63(6):1128–40.
Van Raalte DH, Bjornstad P, Persson F, Powell DR, De Cassia CR, Wang PS, et al. The impact of sotagliflozin on renal function, albuminuria, blood pressure, and hematocrit in adults with type 1 diabetes. Diabetes Care. 2019;42(10):1921–9.
Tuttle KR, Brosius FC, Cavender MA, Fioretto P, Fowler KJ, Heerspink HJL, et al. SGLT2 inhibition for CKD and cardiovascular disease in type 2 diabetes: report of a scientific workshop sponsored by the national kidney foundation. Diabetes. 2021;70(1):1–16.
Lawler PR, Liu H, Frankfurter C, Lovblom LE, Lytvyn Y, Burger D, et al. Changes in cardiovascular biomarkers associated with the sodium–glucose cotransporter 2 (SGLT2) inhibitor ertugliflozin in patients with chronic kidney disease and type 2 diabetes. Diabetes Care. 2021;44(3):e45–7. https://doi.org/10.2337/dc20-2265.
Inzucchi SE, Zinman B, Fitchett D, Wanner C, Ferrannini E, Schumacher M, et al. How does empagliflozin reduce cardiovascular mortality? Insights from a mediation analysis of the EMPA-REG OUTCOME trial. Diabetes Care. 2018;41(2):356–63.
Cherney DZ, Perkins BA, Soleymanlou N, Har R, Fagan N, Johansen OE, et al. The effect of empagliflozin on arterial stiffness and heart rate variability in subjects with uncomplicated type 1 diabetes mellitus. Cardiovasc Diabetol. 2014;13:28.
van Raalte DH, Bjornstad P, Persson F, Powell DR, de Cassia CR, Wang PS, et al. The impact of sotagliflozin on renal function, albuminuria, blood pressure, and hematocrit in adults with type 1 diabetes. Diabetes Care. 2019;44(6):1–9.
Mathieu C, Dandona P, Birkenfeld AL, Hansen TK, Iqbal N, Xu J, et al. Benefit/risk profile of dapagliflozin 5 mg in the DEPICT-1 and -2 trials in individuals with type 1 diabetes and body mass index >/=27 kg/m(2). Diabetes Obes Metab. 2020;22(11):2151–60.
Li J, Neal B, Perkovic V, de Zeeuw D, Neuen BL, Arnott C, et al. Mediators of the effects of canagliflozin on kidney protection in patients with type 2 diabetes. Kidney Int. 2020;98(3):769–77.
Li J, Woodward M, Perkovic V, Figtree GA, Heerspink HJL, Mahaffey KW, et al. Mediators of the effects of canagliflozin on heart failure in patients with type 2 diabetes. JACC Heart Fail. 2020;8(1):57–66.
Mathieu C, Dandona P, Gillard P, Senior P, Hasslacher C, Araki E, et al. Efficacy and safety of dapagliflozin in patients with inadequately controlled type 1 diabetes (the DEPICT-2 Study): 24-Week results from a randomized controlled trial. Diabetes Care. 2018;41(9):1938–46.
Dandona P, Mathieu C, Phillip M, Hansen L, Griffen SC, Tschöpe D, et al. Efficacy and safety of dapagliflozin in patients with inadequately controlled type 1 diabetes (DEPICT-1): 24 week results from a multicentre, double-blind, phase 3, randomised controlled trial. Lancet Diabetes Endocrinol. 2017;5(11):864–76.
Scheen AJ. An update on the safety of SGLT2 inhibitors. Expert Opin Drug Saf. 2019;18(4):295–311.
Cahn A, Melzer-Cohen C, Pollack R, Chodick G, Shalev V. Acute renal outcomes with sodium-glucose co-transporter-2 inhibitors: Real-world data analysis. Diabetes Obes Metab. 2019;21(2):340–8.
Menne J, Dumann E, Haller H, Schmidt BMW. Acute kidney injury and adverse renal events in patients receiving SGLT2-inhibitors: A systematic review and meta-analysis. PLoS Med. 2019;16(12):e1002983.
Heerspink HJL, Cherney D, Postmus D, Stefánsson BV, Chertow GM, Dwyer JP, et al. A pre-specified analysis of the Dapagliflozin and Prevention of Adverse Outcomes in Chronic Kidney Disease (DAPA-CKD) randomized controlled trial on the incidence of abrupt declines in kidney function. Kidney Int. 2022;101(1):174–84. https://doi.org/10.1016/j.kint.2021.09.005.
Oshima M, Jardine MJ, Agarwal R, Bakris G, Cannon CP, Charytan DM, et al. Insights from CREDENCE trial indicate an acute drop in estimated glomerular filtration rate during treatment with canagliflozin with implications for clinical practice. Kidney Int. 2021;99(4):999–1009. https://doi.org/10.1016/j.kint.2020.10.042.
Oshima M, Neal B, Toyama T, Ohkuma T, Li Q, de Zeeuw D, et al. Different eGFR decline thresholds and renal effects of canagliflozin: Data from the CANVAS program. J Am Soc Nephrol. 2020;31(10):2446–56.
Kraus BJ, Weir MR, Bakris GL, Mattheus M, Cherney DZI, Sattar N, et al. Characterization and implications of the initial estimated glomerular filtration rate 'dip' upon sodium-glucose co-transporter-2 inhibition with empagliflozin in the EMPA-REG OUTCOME trial. Kidney Int. 2021;99(3):750–62. https://doi.org/10.1016/j.kint.2020.10.031.
Holtkamp FA, de Zeeuw D, Thomas MC, Cooper ME, de Graeff PA, Hillege HJ, et al. An acute fall in estimated glomerular filtration rate during treatment with losartan predicts a slower decrease in long-term renal function. Kidney Int. 2011;80(3):282–7.
Cryer PE. The barrier of hypoglycemia in diabetes. Diabetes. 2008;57(12):3169–76.
Kelly MS, Lewis J, Huntsberry AM, Dea L, Portillo I. Efficacy and renal outcomes of SGLT2 inhibitors in patients with type 2 diabetes and chronic kidney disease. Postgrad Med. 2019;131(1):31–42.
Hodson DJ, Rorsman P. A variation on the theme: SGLT2 inhibition and glucagon secretion in human islets. Diabetes. 2020;69(5):864–6.
Ferrannini E, Mark M, Mayoux E. CV protection in the EMPA-REG OUTCOME trial: A “Thrifty Substrate” hypothesis. Diabetes Care. 2016;39(7):1108–14.
Lopaschuk GD, Verma S. Empagliflozin’s fuel hypothesis: not so soon. Cell Metab. 2016;24(2):200–2.
Monami M, Nreu B, Zannoni S, Lualdi C, Mannucci E. Effects of SGLT-2 inhibitors on diabetic ketoacidosis: A meta-analysis of randomised controlled trials. Diabetes Res Clin Pract. 2017;130:53–60.
Fralick M, Schneeweiss S, Patorno E. Risk of Diabetic Ketoacidosis after Initiation of an SGLT2 Inhibitor. N Engl J Med. 2017;376(23):2300–2.
Yamada T, Shojima N, Noma H, Yamauchi T, Kadowaki T. Sodium-glucose co-transporter-2 inhibitors as add-on therapy to insulin for type 1 diabetes mellitus: Systematic review and meta-analysis of randomized controlled trials. Diabetes Obes Metab. 2018;20(7):1755–61.
Miller KM, Foster NC, Beck RW, Bergenstal RM, DuBose SN, DiMeglio LA, et al. Current state of type 1 diabetes treatment in the U.S.: updated data from the T1D Exchange clinic registry. Diabetes Care. 2015;38(6):971–8.
Fioretto P, Zambon A, Rossato M, Busetto L, Vettor R. SGLT2 inhibitors and the diabetic kidney. Diabetes Care. 2016;39(Supplement 2):S165–71.
Nguyen KT, Xu NY, Zhang JY, Shang T, Basu A, Bergenstal RM, et al. Continuous Ketone Monitoring Consensus Report 2021. J Diabetes Sci Technol. 2021;19322968211042656. https://doi.org/10.1177/19322968211042656.
Zhang JY, Shang T, Koliwad SK, Klonoff DC. Continuous ketone monitoring: A new paradigm for physiologic monitoring. J Diabetes Sci Technol. 2021;15(4):775–80.
Acknowledgements
D.Z.I.C. is supported by a Department of Medicine, University of Toronto Merit Award and receives support from the CIHR, the Heart and Stroke Richard Lewar Centre of Excellence, the Heart and Stroke Foundation and the Kidney Foundation of Canada. V.S.S. is supported by the Department of Medicine Eliot Phillipson Clinician Scientist Training Program, a Banting and Best Diabetes Centre Postdoctoral fellowship at the University of Toronto, and a CIHR Frederick Banting and Charles Best Canada Graduate Scholarships Doctoral Research Award. B.A.P. acknowledges support as the Sam and Judy Pencer Family Chair in Diabetes Clinical Research at the University of Toronto, from Diabetes Action Canada and its Innovations in Type 1 Diabetes Goal Group, Boehringer Ingelheim’s Beta Cell Preservation program, the Menkes Foundation, and contributions from David Wright.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
D.Z.I.C. has received consulting fees or speaking honorarium or both from Janssen, Bayer, Boehringer Ingelheim-Eli, Lilly, AstraZeneca, Merck & Co Inc, Prometic and Sanofi, and has received operating funds from Janssen, Boehringer Ingelheim-Eli, Lilly, Sanofi, AstraZeneca and Merck & Co Inc. B.A.P. has received speaker honoraria from Abbott, Medtronic, Insulet, and Novo-Nordisk; research support to his research institute from Boehringer Ingelheim, Novo Nordisk, and the Bank of Montreal (BMO), and has served as a consultant to Boehringer Ingelheim, Abbott, Insulet, and Novo-Nordisk. J.R. has served on advisory boards for Applied Therapeutics, Boehringer Ingelheim, Eli Lilly, Intarcia, Janssen, Novo Nordisk, Oramed, Sanofi, and Zealand; and has received research support from Applied Therapeutics, AstraZeneca, Boehringer Ingelheim, Eli Lilly, Genentech, GlaxoSmithKline, Intarcia, Janssen, Lexicon, Merck, Novo Nordisk, Oramed, Pfizer and Sanofi. No potential conflicts of interest relevant to this article were reported for H.L. and V.S.S.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Microvascular Complications—Nephropathy
Hongyan Liu and Vikas S. Sridhar are Co-primary authors
Rights and permissions
About this article
Cite this article
Liu, H., Sridhar, V.S., Perkins, B.A. et al. SGLT2 Inhibition in Type 1 Diabetes with Diabetic Kidney Disease: Potential Cardiorenal Benefits Can Outweigh Preventable Risk of Diabetic Ketoacidosis. Curr Diab Rep 22, 317–332 (2022). https://doi.org/10.1007/s11892-022-01471-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11892-022-01471-2