Abstract
Purpose of Review
To provide a review of recent literature on the treatment of moderate-to-severe calcification in coronary and peripheral vasculature with intravascular lithotripsy (Shockwave Medical, Santa Clara, CA).
Recent Findings
Moderate-to-severe calcific plaques constitute a significant proportion of lesions treated with transcatheter interventions in the coronary and peripheral vascular beds and portend lower procedural success rates, increased periprocedural major adverse events, and unfavorable long-term clinical outcomes compared to non-calcific plaques. Intravascular lithotripsy (IVL) is a new technique that uses acoustic shock waves in a balloon-based system to induce fracture in the calcium deposits to facilitate luminal gain and stent expansion.
Summary
IVL demonstrated high procedural success and low complication rates in the management of moderate-to-severe calcification in coronary and peripheral vascular beds and led to large luminal gain by modification of calcific plaque as assessed by optical coherence tomography. Further studies will determine the role of IVL in an integrated, protocolized approach to the treatment of severely calcified plaques in the coronary and peripheral vascular beds.

Similar content being viewed by others
Abbreviations
- BTK:
-
Below-the-knee
- CAD:
-
Coronary artery disease
- DCB:
-
Drug coated balloons
- IVL:
-
Intravascular lithotripsy
- MACE:
-
Major adverse cardiovascular events
- MAE:
-
Major adverse events
- OA:
-
Orbital atherectomy
- PARC:
-
Peripheral Academic Research Consortium
- PCI:
-
Percutaneous coronary intervention
- PTA:
-
Percutaneous transluminal angioplasty
- RA:
-
Rotational atherectomy
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
• Mori H, Torii S, Kutyna M, Sakamoto A, Finn AV, Virmani R. Coronary artery calcification and its progression: what does it really mean?. JACC Cardiovasc Imaging. 2018;11:127–42. This paper reviews two types of coronary calficification with their progression and histopathological relevance to respective clinical presentation of ischemic coronary disease.
Genereux P, Madhavan MV, Mintz GS, Maehara A, Palmerini T, Lasalle L, et al. Ischemic outcomes after coronary intervention of calcified vessels in acute coronary syndromes. Pooled analysis from the HORIZONS-AMI (Harmonizing Outcomes With Revascularization and Stents in Acute Myocardial Infarction) and ACUITY (Acute Catheterization and Urgent Intervention Triage Strategy) TRIALS. J Am Coll Cardiol. 2014;63:1845–54.
Walker KL, Nolan BW, Columbo JA, Rzucidlo EM, Goodney PP, Walsh DB, et al. Lesion complexity drives the cost of superficial femoral artery endovascular interventions. J Vasc Surg. 2015;62:998–1002.
Soor GS, Vukin I, Leong SW, Oreopoulos G, Butany J. Peripheral vascular disease: who gets it and why? A histomorphological analysis of 261 arterial segments from 58 cases. Pathology. 2008;40:385–91.
Fanelli F, Cannavale A, Gazzetti M, Lucatelli P, Wlderk A, Cirelli C, et al. Calcium burden assessment and impact on drug-eluting balloons in peripheral arterial disease. Cardiovasc Intervent Radiol. 2014;37:898–907.
Babaev A, Zavlunova S, Attubato MJ, Martinsen BJ, Mintz GS, Maehara A. Orbital atherectomy plaque modification assessment of the femoropopliteal artery via intravascular ultrasound (TRUTH Study). Vasc Endovascular Surg. 2015;49:188–94.
Holmes SA, Whitfield HN. The current status of lithotripsy. Br J Urol. 1991;68:337–44.
Cleveland RO, McAteer JA. The physics of shock wave lithotripsy. Smith’s textbook of endourology: 3rd Edition 1: Wiley-Blackwell. 2012:527–58.
Dini CS, Tomberli B, Mattesini A, Ristalli F, Valente S, Stolcova M, et al. Intravascular lithotripsy for calcific coronary and peripheral stenoses. EuroIntervention. 2019.
Brodmann M, Werner M, Brinton TJ, Illindala U, Lansky A, Jaff MR, et al. Safety and performance of lithoplasty for treatment of calcified peripheral artery lesions. J Am Coll Cardiol. 2017;70:908–10.
•• Brodmann M, Werner M, Holden A, Tepe G, Scheinert D, Schwindt A, et al. Primary outcomes and mechanism of action of intravascular lithotripsy in calcified, femoropopliteal lesions: results of Disrupt PAD II. Catheter Cardiovasc Interv. 2019;93:335–42. A non-randomized, multicenter study established the safety of IVL in complex calcified PAD lesions with minimal vessel injury and need for adjunctive therapy.
Tepe G, Brodmann M, Werner M, Bachinsky W, Holden A, Zeller T, et al. Intravascular lithotripsy for peripheral artery calcification: 30-day outcomes from the randomized disrupt PAD III trial. JACC Cardiovasc Interv. 2021;14:1352–61.
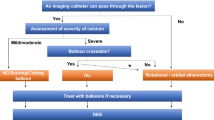
Karimi Galougahi K, Shlofmitz E, Jeremias A, Gogia S, Kirtane AJ, Hill JM, et al. Therapeutic approach to calcified coronary lesions: disruptive technologies. Curr Cardiol Rep. 2021;23:33.
• Brodmann M, Holden A, Zeller T. Safety and feasibility of intravascular lithotripsy for treatment of below-the-knee arterial stenoses. J Endovasc Ther. 2018;25:499–503. This non-randomized, multicenter prospective study established the safety of IVL in the treatment of moderate-to-severe calcification in infrapopliteal arteries with no MAE events at 30 days in 20 patients.
Karimi Galougahi K, Soukas PA, Kolski B, Tayal R, Parikh SA, Armstrong EJ, et al. Acoustic shock waves to modify calcific plaques - intravascular lithotripsy in the peripheral circulation. Cardiovasc Revasc Med. 2021.
•• Brodmann M, Schwindt A, Argyriou A, Gammon R. Safety and feasibility of intravascular lithotripsy for treatment of common femoral artery stenoses. J Endovasc Ther. 2019;26:283–7. This non-randomized, multicenter study demonstrated the safety and effectiveness of IVL in the treatment of calficified femoral artery lesions.
•• Di Mario C, Goodwin M, Ristalli F, Ravani M, Meucci F, Stolcova M, et al. A prospective registry of intravascular lithotripsy-enabled vascular access for transfemoral transcatheter aortic valve replacement. JACC Cardiovasc Interv. 2019;12:502–4. Four centers in Italy and 4 centers in USA established a prospective registry for use of IVL in transfemoral TAVR access in patients with otherwise ineligible femoral arterial access due to severely calcific femoral artery disease. Greater than 90% of patients successfully underwent transfemoral TAVR after use of IVL with low complication rates.
• Gorla R, Cannone GS, Bedogni F, De Marco F. Transfemoral aortic valve implantation following lithoplasty of iliac artery in a patient with poor vascular access. Catheter Cardiovasc Interv. 2019;93:E140–E2. A successful use of IVL in a 87-year-old patient with severely calficic femoral artery disease in preparation for transfemoral TAVR.
• Cruz-Gonzalez I, Gonzalez Ferreiro R, Martin Moreiras J, Trejo Velasco B, Barreiro Perez M, Diego Nieto A, et al. Facilitated transfemoral access by shockwave lithoplasty for transcatheter aortic valve replacement. JACC Cardiovasc Interv. 2019;12:e35–e8. A case demonstrating successful use of IVL in a 80-year-old patient with severely calcific femoral artery disease in preparation for transfemoral TAVR.
• Rosseel L, De Backer O, Sondergaard L, Bieliauskas G. Intravascular iliac artery lithotripsy to enable transfemoral thoracic endovascular aortic repair. Catheter Cardiovasc Interv. 2019. A case demonstrating first-in-man use of IVL in a 69-year-old patient with severely calcified iliac arteries enabling use of thoracic endovascular aortic repair for thoracic aortic aneurysm.
• Khalid N, Iantorno M, Shlofmitz E, Hashim H, Waksman R, Bernardo N. Kissing intravascular lithotripsy facilitated endovascular repair of a complex saccular abdominal aortic aneurysm with narrowed distal aorta: a first-in-human report. JACC Cardiovasc Interv. 2019;12:e97–e9. A first-in-man case report of use of IVL in a 84-year-old patient with narrowed distal aorta and complex saccular abdominal aortic aneurysm facilitating delivery of endovascular stent graft.
• Riley RF, Corl JD, Kereiakes DJ. Intravascular lithotripsy-assisted Impella insertion: a case report. Catheter Cardiovasc Interv. 2019;93:1317–9. A case illustrating use of IVL to facilitate 14 French sheath for use of Impella mechanical circulatory device.
Brinton TJ, Ali ZA, Hill JM, Meredith IT, Maehara A, Illindala U, et al. Feasibility of Shockwave coronary intravascular lithotripsy for the treatment of calcified coronary stenoses. Circulation. 2019;139:834–6.
•• Ali ZA, Brinton TJ, Hill JM, Maehara A, Matsumura M, Karimi Galougahi K, et al. Optical coherence tomography characterization of coronary lithoplasty for treatment of calcified lesions: first description. JACC Cardiovasc Imaging. 2017;10:897–906. A prospective, multicenter, single arm study to assess feasibility of IVL in calcific coronary lesions which met primary endpoint with no MACE in 60 patients enrolled.
Attizzani GF, Patricio L, Bezerra HG. Optical coherence tomography assessment of calcified plaque modification after rotational atherectomy. Catheter Cardiovasc Interv. 2013;81:558–61.
Mestre RT, Alegria-Barrero E, Di Mario C. A coronary “tunnel”: optical coherence tomography assessment after rotational atherectomy. Catheter Cardiovasc Interv. 2014;83:E171-3.
Kini AS, Vengrenyuk Y, Pena J, Motoyama S, Feig JE, Meelu OA, et al. Optical coherence tomography assessment of the mechanistic effects of rotational and orbital atherectomy in severely calcified coronary lesions. Catheter Cardiovasc Interv. 2015;86:1024–32.
Karimi Galougahi K, Shlofmitz RA, Ben-Yehuda O, Genereux P, Maehara A, Mintz GS, et al. Guiding light: insights into atherectomy by optical coherence tomography. JACC Cardiovasc Interv. 2016;9:2362–3.
Tomey MI, Sharma SK. Interventional options for coronary artery calcification. Curr Cardiol Rep. 2016;18:12.
Abdel-Wahab M, Richardt G, Joachim Buttner H, Toelg R, Geist V, Meinertz T, et al. High-speed rotational atherectomy before paclitaxel-eluting stent implantation in complex calcified coronary lesions: the randomized ROTAXUS (Rotational Atherectomy Prior to Taxus Stent Treatment for Complex Native Coronary Artery Disease) trial. JACC Cardiovasc Interv. 2013;6:10–9.
Chambers JW, Feldman RL, Himmelstein SI, Bhatheja R, Villa AE, Strickman NE, et al. Pivotal trial to evaluate the safety and efficacy of the orbital atherectomy system in treating de novo, severely calcified coronary lesions (ORBIT II). JACC Cardiovasc Interv. 2014;7:510–8.
Maejima N, Hibi K, Saka K, Akiyama E, Konishi M, Endo M, et al. Relationship between thickness of calcium on optical coherence tomography and crack formation after balloon dilatation in calcified plaque requiring rotational atherectomy. Circ J. 2016;80:1413–9.
•• Saito S, Yamazaki S, Takahashi A, Namiki A, Kawasaki T, Otsuji S, et al. Intravascular lithotripsy for vessel preparation in severely calcified coronary arteries prior to stent placement- primary outcomes from the Japanese disrupt CAD IV Study. Circ J. 2021;85:826–33. A prospective, multicenter study to assess safety and feasibility of IVL in Japanese population. Similar to the Disrupt CAD III, it demonstrated high procedural success with low MACE rates in Japanese population.
•• Hill JM, Kereiakes DJ, Shlofmitz RA, Klein AJ, Riley RF, Price MJ, et al. Intravascular lithotripsy for treatment of severely calcified coronary artery disease. J Am Coll Cardiol. 2020;76:2635–46. A prospective, single-arm multicenter study showing safety and feasibility of IVL in severe coronary calcification to optimize stent deployment. Of note, an OCT sub-study demonstrated that multiplane and longitudinal calcium fractures were present 67.4% of lesions after IVL.
•• Ali ZA, Nef H, Escaned J, Werner N, Banning AP, Hill JM, et al. Safety and effectiveness of coronary intravascular lithotripsy for treatment of severely calcified coronary stenoses: the disrupt CAD II study. Circ Cardiovasc Interv. 2019;12:e008434. A prospective, single-arm, multicenter study that demonstrated the feasibility of IVL for modification of severe coronary artery calcification. Of note, an OCT sub-study provided insights into mechanism of action of IVL in coronary vascular bed that identified calcium fracture.
• Ali ZA, McEntegart M, Hill JM, Spratt JC. Intravascular lithotripsy for treatment of stent underexpansion secondary to severe coronary calcification. Eur Heart J. 2018. Novel use of IVL in a 73-year-old patient with limiting angina and in-stent stenosis refractory to high-pressure noncompliant balloon dilation. OCT confirmed severe in-stent stenosis and stent underexpansion. IVL facilitated resolution of in-stent stenosis and stent expansion.
Tovar Forero MN, Wilschut J, Van Mieghem NM, Daemen J. Coronary lithoplasty: a novel treatment for stent underexpansion. Eur Heart J. 2019;40:221.
Salazar C, Escaned J, Tirado G, Gonzalo N. Recurrent restenosis caused by severe calcific neoatherosclerosis treated with intravascular lithotripsy. EuroIntervention. 2019.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
Ziad A. Ali: grants from NIH/NHLBI (coinvestigator), Institutional research grants from Abbott, Philips, Boston Scientific, Acist Medical, Abiomed, Opsens, Medtronic, Cardiovascular Systems Inc.; consultant—Amgen, AstraZeneca, Boston Scientific; equity—Shockwave Medical. Dr. Shlofmitz reports personal fees from ShockWave Medical outside the submitted work. Other authors: none.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on New Therapies for Cardiovascular Disease
Rights and permissions
About this article
Cite this article
Ozdemir, D., Karimi Galougahi, K., Petrossian, G. et al. Calcific Plaque Modification by Acoustic Shockwaves: Intravascular Lithotripsy in Cardiovascular Interventions. Curr Cardiol Rep 24, 519–528 (2022). https://doi.org/10.1007/s11886-022-01674-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11886-022-01674-9