Abstract
Purpose of Review
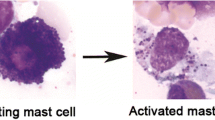
Mast cell (MC) activation can present with a wide range of symptoms. The mechanisms that cause such activation are varied. One of them is the presence of clonal MCs which is defined, within other possible changes, by the presence of a somatic, activating mutation in the KIT gene. The clinical course and prognosis of patients with this underlying disease may be different from other causes of MC activation (MCA). For this reason, it is important to early diagnose, or at least suspect, which patients with MCA are due to clonal MCs.
Recent Findings
The diagnosis of clonality must be made in a comprehensive manner. However, this paper reviews chronologically each of the stages from the patient’s first visit to the doctor’s office which can be indicative of clonality: clinical presentation of MCA, physical examination, analytical determinations of tryptase, and/or KIT mutational analysis and bone involvement, among others. The different clonality predictive scores proposed are also reviewed and compared.
Summary
Although the gold standard for the diagnosis of certainty of MC clonality is the performance of a bone marrow (BM) biopsy, there are clinical symptoms, signs, and biological parameters suggestive of clonality, as well as predictive scores, which can guide (or rule out) an early diagnosis and avoid unnecessary BM biopsies.
Similar content being viewed by others
Data Availability
The data that support the findings of this review are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Rottem M, Okada T, Goff JP, Metcalfe DD. Mast cells cultured from the peripheral blood of normal donors and patients with mastocytosis originate from a CD34+/Fc epsilon RI- cell population. Blood. 1994;84:2489–96.
Kempuraj D, Saito H, Kaneko A, Fukagawa K, Nakayama M, Toru H, et al. Characterization of mast cell-committed progenitors present in human umbilical cord blood. Blood. 1999;93:3338–46.
Gonzalez-de-Olano D, Álvarez-Twose I. Mast cells as key players in allergy and inflammation. J Investig Allergol Clin Immunol. 2018;28:365–78.
Valent P, Akin C, Arock M, Brockow K, Butterfield JH, Carter MC, et al. Definitions, criteria and global classification of mast cell disorders with special reference to mast cell activation syndromes: a consensus proposal. Int Arch Allergy Immunol. 2012;157:215–25.
Valent P. Mast cell activation syndromes: definition and classification. Allergy. 2013;68:417–24.
Akin C, Valent P, Metcalfe DD. Mast cell activation syndrome: proposed diagnostic criteria. J Allergy Clin Immunol. 2010;126:1099-104.e4.
• Valent P, Akin C, Nedoszytko B, Bonadonna P, Hartmann K, Niedoszytko M, et al. Diagnosis, classification and management of mast cell activation syndromes (MCAS) in the era of personalized medicine. Int J Mol Sci. 2020;21:1–14. Current description of MC activation symptoms and underlying mechanisms, MCAS classification, and differential diagnosis.
Akin C, Scott LM, Kocabas CN, Kushnir-Sukhov N, Brittain E, Noel P, et al. Demonstration of an aberrant mast-cell population with clonal markers in a subset of patients with “idiopathic” anaphylaxis. Blood. 2007;110:2331–3.
Sonneck K, Florian S, Mullauer L, Wimazal F, Fodinger M, Sperr WR, et al. Diagnostic and subdiagnostic accumulation of mast cells in the bone marrow of patients with anaphylaxis: Monoclonal mast cell activation syndrome. Int Arch Allergy Immunol. 2007;142:158–64.
• Arber DA, Orazi A, Hasserjian RP, Borowitz MJ, Calvo K, Kvasnicka H, et al. Arber. International consensus classification of myeloid neoplasms and acute leukemias integrating morphologic, clinical, and genomic data. Blood. 2022;140:1200–28. Updated guide to the main hematopoietic diseases, including mastocytosis and their diagnostic criteria.
Decker WW, Campbell RL, Manivannan V, Luke A, St Sauver JL, Weaver A, et al. The etiology and incidence of anaphylaxis in Rochester, Minnesota: a report from the Rochester Epidemiology Project. J Allergy Clin Immunol. 2008;122:1161–5.
Simons FER, Peterson S, Black CD. Epinephrine dispensing patterns for an out-of-hospital population: a novel approach to studying the epidemiology of anaphylaxis. J Allergy Clin Immunol. 2002;110:647–51.
González-Pérez A, Aponte Z, Vidaurre CF, Rodríguez LAG. Anaphylaxis epidemiology in patients with and patients without asthma: a United Kingdom database review. J Allergy Clin Immunol. 2010;125:1098–105.
Sheikh A, Hippisley-Cox J, Newton J, Fenty J. Trends in national incidence, lifetime prevalence and adrenaline prescribing for anaphylaxis in England. J R Soc Med. 2008;101:139–43.
Bohlke K, Davis RL, DeStefano F, Marcy SM, Braun MM, Thompson RS. Epidemiology of anaphylaxis among children and adolescents enrolled in a health maintenance organization. J Allergy Clin Immunol. 2004;113:536–42.
Boros CA, Kay D, Gold MS. Parent reported allergy and anaphylaxis in 4173 South Australian children. J Paediatr Child Health. 2000;36:36–40.
Tejedor Alonso MA, Moro Moro M, Múgica García MV, Esteban Hernández J, Rosado Ingelmo A, Vila Albelda C, et al. Incidence of anaphylaxis in the city of Alcorcon (Spain): a population-based study. Clin Exp Allergy. 2012;42:578–89.
González-de-Olano D, de-la-Hoz-Caballer B, Núñez-López R, Sánchez-Muñoz L, Cuevas-Agustín M, Diéguez MC, et al. Prevalence of allergy and anaphylactic symptoms in 210 adult and pediatric patients with mastocytosis in Spain: a study of the Spanish Network on Mastocytosis (REMA). Clin Exp Allergy. 2007;37:1547–55.
Brockow K, Jofer C, Behrendt H, Ring J. Anaphylaxis in patients with mastocytosis: a study on history, clinical features and risk factors in 120 patients. Allergy. 2008;63:226–32.
Gulen T, Hagglund H, Dahlen B, Nilsson G. High prevalence of anaphylaxis in patients with systemic mastocytosis - a single-centre experience. Clin Exp Allergy. 2014;44:121–9.
González-de-Olano D, Esteban-López MI, Alonso-Díaz-de-Durana MD, González-Mancebo E, Prieto-García A, Gandolfo-Cano M, et al. Frequency of clonal mast cell diseases among patients presenting with anaphylaxis: a prospective study in 178 patients from 5 tertiary centers in Spain. J Allergy Clin Immunol Pract. 2019;7:2924-2926.e1.
Álvarez-Twose I, González-de-Olano D, Sánchez-Muñoz L, Matito A, Esteban-López MI, Vega A, et al. Clinical, biological, and molecular characteristics of clonal mast cell disorders presenting with systemic mast cell activation symptoms. J Allergy Clin Immunol. 2010;125:1269-1278.e2.
González-de-Olano D, Álvarez-Twose I. Insights in anaphylaxis and clonal mast cell disorders. Front Immunol. 2017;8:792.
Bonadonna P, Lombardo C, Zanotti R. Mastocytosis and allergic diseases. J Investig Allergol Clin Immunol. 2014;24:288–97; quiz 3 p preceding 297.
Bonadonna P, Zanotti R, Muller U. Mastocytosis and insect venom allergy. Curr Opin Allergy Clin Immunol. 2010;10:347–53.
Gulen T, Hagglund H, Sander B, Dahlen B, Nilsson G. The presence of mast cell clonality in patients with unexplained anaphylaxis. Clin Exp Allergy. 2014;44:1179–87.
Carter MC, Desai A, Komarow HD, Bai Y, Clayton ST, Clark AS, et al. A distinct biomolecular profile identifies monoclonal mast cell disorders in patients with idiopathic anaphylaxis. J Allergy Clin Immunol. 2018;141:180-188.e3.
Hartmann K, Escribano L, Grattan C, Brockow K, Carter MC, Álvarez-Twose I, et al. Cutaneous manifestations in patients with mastocytosis: consensus report of the European Competence Network on Mastocytosis; the American Academy of Allergy, Asthma & Immunology; and the European Academy of Allergology and Clinical Immunology. J Allergy Clin Immunol. 2016;137:35–45.
Matito A, Azaña JM, Torrelo A, Álvarez-Twose I. Cutaneous mastocytosis in adults and children: new classification and prognostic factors. Immunol Allergy Clin North. 2018;38:351–63.
Álvarez-Twose I, Vañó-Galván S, Sánchez-Muñoz L, Morgado JM, Matito A, Torrelo A, et al. Increased serum baseline tryptase levels and extensive skin involvement are predictors for the severity of mast cell activation episodes in children with mastocytosis. Allergy. 2012;67:813–21.
Schwartz LB, Lewis RA, Austen KF. Tryptase from human pulmonary mast cells. Purification and characterization. J Biol Chem. 1981;256:11939–43.
Schwartz LB, Metcalfe DD, Miller JS, Earl H, Sullivan T. Tryptase levels as an indicator of mast-cell activation in systemic anaphylaxis and mastocytosis. N Engl J Med. 1987;316:1622–6.
Lee AYS. Elevated serum tryptase in non-anaphylaxis cases: a concise review. Int Arch Allergy Immunol. 2020;181:357–64.
Lyons JJ, Yu X, Hughes JD, Le QT, Jamil A, Bai Y, et al. Elevated basal serum tryptase identifies a multisystem disorder associated with increased TPSAB1 copy number. Nat Genet. 2016;48:1564–9.
Wu R, Lyons JJ. Hereditary alpha-tryptasemia: a commonly inherited modifier of anaphylaxis. Curr Allergy Asthma Rep. 2021;21:1–9.
Greiner G, Sprinzl B, Górska A, Ratzinger F, Gurbisz M, Witzeneder N, et al. Hereditary α tryptasemia is a valid genetic biomarker for severe mediator-related symptoms in mastocytosis. Blood. 2021;137:238–47.
O’Connell MP, Lyons JJ. Hymenoptera venom-induced anaphylaxis and hereditary alpha-tryptasemia. Curr Opin Allergy Clin Immunol. 2020;20:431–7.
Robey RC, Wilcock A, Bonin H, Beaman G, Myers B, Grattan C, et al. Hereditary alpha-tryptasemia: UK prevalence and variability in disease expression. J Allergy Clin Immunol Pract. 2020;8:3549–56.
Chollet MB, Akin C. Hereditary alpha tryptasemia is not associated with specific clinical phenotypes. J Allergy Clin Immunol. 2022;149:728-735.e2.
•• González‐de‐Olano D, Navarro‐Navarro P, Muñoz‐González JI, Sánchez‐Muñoz L, Henriques A, de‐Andrés‐Martín A, et al. Clinical impact of the TPSAB1 genotype in mast cell diseases: a REMA study in a cohort of 959 individuals. Allergy [Internet]. 2023; Available from: https://onlinelibrary.wiley.com/doi/10.1111/all.15911. Longer series in which the clinical impact of mastocytosis and HAT is studied separately.
• Sordi B, Vanderwert F, Crupi F, Gesullo F, Zanotti R, Bonadonna P, et al. Disease correlates and clinical relevance of hereditary alpha-tryptasemia in patients with systemic mastocytosis. J Allergy Clin Immunol. 2023;151:485–93.e11. Multicenter study studying the clinical correlation of germline TPSAB1 copy number gains.
García-Montero AC, Jara-Acevedo M, Teodosio C, Sánchez ML, Núñez R, Prados A, et al. KIT mutation in mast cells and other bone marrow hematopoietic cell lineages in systemic mast cell disorders: a prospective study of the Spanish Network on Mastocytosis (REMA) in a series of 113 patients. Blood. 2006;108:2366–72.
Longley BJ, Tyrrell L, Lu SZ, Ma YS, Langley K, Ding TG, et al. Somatic c-KIT activating mutation in urticaria pigmentosa and aggressive mastocytosis: establishment of clonality in a human mast cell neoplasm. Nat Genet. 1996;12:312–4.
Piao X, Bernstein A. A point mutation in the catalytic domain of c-kit induces growth factor independence, tumorigenicity, and differentiation of mast cells. Blood. 1996;87:3117–23.
Akin C, Kirshenbaum AS, Semere T, Worobec AS, Scott LM, Metcalfe DD. Analysis of the surface expression of c-kit and occurrence of the c-kit Asp816Val activating mutation in T cells, B cells, and myelomonocytic cells in patients with mastocytosis. Exp Hematol. 2000;28:140–7.
Kristensen T, Vestergaard H, Moller MB. Improved detection of the KIT D816V mutation in patients with systemic mastocytosis using a quantitative and highly sensitive real-time qPCR assay. J Mol Diagn. 2011;13:180–8.
Kristensen T, Vestergaard H, Bindslev-Jensen C, Moller MB, Broesby-Olsen S, Mastocytosis Centre OUH. Sensitive KIT D816V mutation analysis of blood as a diagnostic test in mastocytosis. Am J Hematol. 2014;89:493–8.
Jara-Acevedo M, Teodosio C, Sánchez-Muñoz L, Álvarez-Twose I, Mayado A, Caldas C, et al. Detection of the KIT D816V mutation in peripheral blood of systemic mastocytosis: diagnostic implications. Mod Pathol. 2015;28:1138–49.
Muñoz-González JI, Álvarez-Twose I, Jara-Acevedo M, Henriques A, Viñas E, Prieto C, et al. Frequency and prognostic impact of KIT and other genetic variants in indolent systemic mastocytosis. Blood. 2019;134:456–68.
Kristensen T, Broesby-Olsen S, Vestergaard H, Bindslev-Jensen C, Møller MB. Circulating KIT D816V mutation-positive non-mast cells in peripheral blood are characteristic of indolent systemic mastocytosis. Eur J Haematol. 2012;89:42–6.
Broesby-Olsen S, Oropeza AR, Bindslev-Jensen C, Vestergaard H, Moller MB, Siebenhaar F, et al. Recognizing mastocytosis in patients with anaphylaxis: value of KIT D816V mutation analysis of peripheral blood. J Allergy Clin Immunol. 2015;135:262–4.
Greiner G, Gurbisz M, Ratzinger F, Witzeneder N, Simonitsch-Klupp I, Mitterbauer-Hohendanner G, et al. Digital PCR: a sensitive and precise method for KIT D816V quantification in mastocytosis. Clin Chem. 2018;64:547–55.
Kristensen T, Vestergaard H, Bindslev-Jensen C, Mortz CG, Kjaer HF, Ollert M, et al. Prospective evaluation of the diagnostic value of sensitive KIT D816V mutation analysis of blood in adults with suspected systemic mastocytosis. Allergy. 2017;72:1737–43.
Czarny J, Żuk M, Żawrocki A, Plata-Nazar K, Biernat W, Niedoszytko M, et al. New approach to paediatric mastocytosis: implications of kit d816v mutation detection in peripheral blood. Acta Derm Venereol. 2020;100:1–2.
Carter MC, Bai Y, Ruiz-Esteves KN, Scott LM, Cantave D, Bolan H, et al. Detection of KIT D816V in peripheral blood of children with manifestations of cutaneous mastocytosis suggests systemic disease. Br J Haematol. 2018;183:775–82.
• Navarro-Navarro P, Álvarez-Twose I, Pérez-Pons A, Henriques A, Mayado A, García-Montero AC, et al. KITD816V mutation in blood for the diagnostic screening of systemic mastocytosis and mast cell activation syndromes. Allergy. 2022;1446:1–13. Cell enrichment approaches show to significantly improve the sensitivity of the molecular assays which allows detecting the KIT mutation.
•• Henriques A, Muñoz-González JI, Sánchez-Muñoz L, Matito A, Torres-Rivera L, et al. Frequency and prognostic impact of blood-circulating tumor mast cells in mastocytosis. Blood. 2022 Jan 27;139(4):572–583. Circulating mast cells are detected in peripheral blood which provides promising results for future lines of research.
Sturm GJ, Varga EM, Roberts G, Mosbech H, Bilo MB, Akdis CA, et al. EAACI guidelines on allergen immunotherapy: hymenoptera venom allergy. Allergy. 2018;73(4):744–64.
González-de-Olano D, Álvarez-Twose I, Morgado JM, López MI, Castro AV, Diaz de Durana MD, et al. Evaluation of basophil activation in mastocytosis with hymenoptera venom anaphylaxis. Cytometry B Clin Cytom. 2011;80:167–75.
Álvarez-Twose I, Zanotti R, González-de-Olano D, Bonadonna P, Vega A, Matito A, et al. Nonaggressive systemic mastocytosis (SM) without skin lesions associated with insect-induced anaphylaxis shows unique features versus other indolent SM. J Allergy Clin Immunol. 2014;133:520–8.
Zanotti R, Bonifacio M, Isolan C, Tanasi I, Crosera L, Olivieri F, et al. A multidisciplinary diagnostic approach reveals a higher prevalence of indolent systemic mastocytosis: 15-years’ experience of the GISM network. Cancers (Basel). 2021;20(13):6380.
Fuchs D, Kilbertus A, Kofler K, von Bubnoff N, Shoumariyeh K, Zanotti R, et al. Scoring the risk of having systemic mastocytosis in adult patients with mastocytosis in the skin. J Allergy Clin Immunol Pract. 2021;9:1705-1712.e4.
van Doormaal JJ, van der Veer E, van Voorst Vader PC, Kluin PM, Mulder AB, van der Heide S, et al. Tryptase and histamine metabolites as diagnostic indicators of indolent systemic mastocytosis without skin lesions. Allergy. 2012;67:683–90.
Álvarez-Twose I, González-de-Olano D, Sánchez-Muñoz L, Matito A, Jara-Acevedo M, Teodosio C, et al. Validation of the REMA score for predicting mast cell clonality and systemic mastocytosis in patients with systemic mast cell activation symptoms. Int Arch Allergy Immunol. 2011;157:275–80.
Gulen T, Akin C. Idiopathic anaphylaxis: a perplexing diagnostic challenge for allergists. Curr Allergy Asthma Rep. 2021;21:11.
González de Olano D, Cain WV, Bernstein JA, Akin C. Disease spectrum of anaphylaxis disorders. J Allergy Clin Immunol Pract. 2023;11:1989–96.
• Rama TA, Torrado I, Henrinques AF, Sánchez-Muñoz L, Jara-Acevedo M, Navarro-Navarro P, et al. Mast cell activation syndromes: comparison between two scoring models to predict for mast cell clonality. J Allergy Clin Immunol Pract. 2023;11:908–19.e4. Comparison between different predictive scores that help to find the best combination to reach a clonality diagnosis.
• Valent P, Hartmann K, Schwaab J, Álvarez-Twose I, Brockow K, Bonadonna P, et al. Personalized management strategies in mast cell disorders: ECNM-AIM user’s guide for daily clinical practice. J Allergy Clin Immunol Pract. 2022;10:1999–2012.e6. The work provides a guide for application of markers in MCAS, algorithms, prognostic scores, and treatments for use in daily practice.
Pyatilova P, Siebenhaar F. Measuring symptom severity and quality of life in mastocytosis. Immunol Allergy Clin North Am. 2023;43:751–62.
Author information
Authors and Affiliations
Contributions
Both DGO and IAT equally contributed to the conception, data generation, revision, and approval of the manuscript.
Corresponding authors
Ethics declarations
Conflict of Interest
The authors have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gonzalez-de-Olano, D., Álvarez-Twose, I. Predictors of Clonality and Underlying Mastocytosis in Mast Cell Activation Syndromes. Curr Allergy Asthma Rep 24, 25–32 (2024). https://doi.org/10.1007/s11882-023-01122-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11882-023-01122-w