Abstract
Background
Treatment with hematopoietic cell transplantation (HCT) has potentially severe effects on physical and psychosocial functioning. Poor social support has been linked with physical morbidity and mortality as well as psychological distress in HCT survivors. This study tested a theory-driven hypothesis that social support buffers adverse effects of health stressors of comorbidities and graft-versus-host disease (cGVHD) on distress and adherence to recommended healthcare among long-term HCT survivors.
Methods
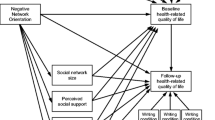
This cross-sectional study analyzed baseline data from a randomized controlled trial in adult survivors 3–18 years post-HCT. Data included medical records and patient-reported outcomes including cancer and treatment distress (CTXD), healthcare adherence (HCA), comorbidity index, cGVHD, ENRICHD Social Support Instrument (ESSI), Social Activity Log, and Health Self-Efficacy. We tested hypothesized models for HCA and CTXD using blocked hierarchical linear regressions.
Results
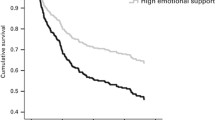
Among the 781 HCT survivors completing baseline assessment, 38% had > 3 comorbidities, 8% had moderate–severe cGVHD, 30% reported low social support, 30% reported elevated distress, and 49% reported low healthcare adherence. Social support and self-efficacy were directly related to both adherence and distress. Regression models supported the hypothesized moderated relationships for distress but not for healthcare adherence.
Conclusions
The two tested models confirm that the health stressors of comorbidities and cGVHD are moderated by better social support and self-efficacy in their associations with lower distress but without moderating effects for healthcare adherence.
Implications for Cancer Survivors
Social support and self-efficacy confer protective benefits on healthcare adherence and psychological distress. Interventions are needed that focus on maintaining social networks or finding new networks if necessary.
Clinical trial registration number
NCT00799461.

Similar content being viewed by others
Change history
07 April 2021
A Correction to this paper has been published: https://doi.org/10.1007/s11764-021-01029-3
References
Hahn T, McCarthy PL Jr, Hassebroek A, Bredeson C, Gajewski JL, Hale GA, et al. Significant improvement in survival after allogeneic hematopoietic cell transplantation during a period of significantly increased use, older recipient age, and use of unrelated donors. J Clin Oncol. 2013;31(19):2437–49. https://doi.org/10.1200/jco.2012.46.6193.
McCarthy PL Jr, Hahn T, Hassebroek A, Bredeson C, Gajewski J, Hale G, et al. Trends in use of and survival after autologous hematopoietic cell transplantation in North America, 1995-2005: significant improvement in survival for lymphoma and myeloma during a period of increasing recipient age. Biol Blood Marrow Transplant. 2013;19(7):1116–23. https://doi.org/10.1016/j.bbmt.2013.04.027.
Martin PJ, Counts GW Jr, Appelbaum FR, Lee SJ, Sanders JE, Deeg HJ, et al. Life expectancy in patients surviving more than 5 years after hematopoietic cell transplantation. J Clin Oncol. 2010;28(6):1011–6. https://doi.org/10.1200/jco.2009.25.6693.
Wingard JR, Majhail NS, Brazauskas R, Wang Z, Sobocinski KA, Jacobsohn D, et al. Long-term survival and late deaths after allogeneic hematopoietic cell transplantation. J Clin Oncol. 2011;29(16):2230–9. https://doi.org/10.1200/jco.2010.33.7212.
Bevans M, El-Jawahri A, Tierney DK, Wiener L, Wood WA, Hoodin F, et al. National Institutes of Health Hematopoietic Cell Transplantation Late Effects Initiative: the patient-centered outcomes working group report. Biol Blood Marrow Transplant. 2017;23(4):538–51. https://doi.org/10.1016/j.bbmt.2016.09.011.
Majhail NS, Rizzo JD, Lee SJ, Aljurf M, Atsuta Y, Bonfim C, et al. Recommended screening and preventive practices for long-term survivors after hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2012;18(3):348–71. https://doi.org/10.1016/j.bbmt.2011.12.519.
Yi JC, Syrjala KL. Sexuality after hematopoietic stem cell transplantation. Cancer J. 2009;15(1):57–64. https://doi.org/10.1097/PPO.0b013e318198c758.
Khera N, Chow EJ, Leisenring WM, Syrjala KL, Baker KS, Flowers ME, et al. Factors associated with adherence to preventive care practices among hematopoietic cell transplantation survivors. Biol Blood Marrow Transplant. 2011;17(7):995–1003. https://doi.org/10.1016/j.bbmt.2010.10.023.
Bishop MM, Lee SJ, Beaumont JL, Andrykowski MA, Rizzo JD, Sobocinski KA, et al. The preventive health behaviors of long-term survivors of cancer and hematopoietic stem cell transplantation compared with matched controls. Biol Blood Marrow Transplant. 2010;16(2):207–14. https://doi.org/10.1016/j.bbmt.2009.09.015.
Armenian SH, Sun CL, Francisco L, Baker KS, Weisdorf DJ, Forman SJ, et al. Health behaviors and cancer screening practices in long-term survivors of hematopoietic cell transplantation (HCT): a report from the BMT Survivor Study. Bone Marrow Transplant. 2012;47(2):283–90. https://doi.org/10.1038/bmt.2011.60.
Uchino BN, Bowen K, Carlisle M, Birmingham W. Psychological pathways linking social support to health outcomes: a visit with the “ghosts” of research past, present, and future. Soc Sci Med. 2012;74(7):949–57. https://doi.org/10.1016/j.socscimed.2011.11.023.
Barth J, Schneider S, von Kanel R. Lack of social support in the etiology and the prognosis of coronary heart disease: a systematic review and meta-analysis. Psychosom Med. 2010;72(3):229–38. https://doi.org/10.1097/PSY.0b013e3181d01611.
Pinquart M, Hoffken K, Silbereisen RK, Wedding U. Social support and survival in patients with acute myeloid leukaemia. Support Care Cancer. 2007;15(1):81–7. https://doi.org/10.1007/s00520-006-0114-x.
Holden L, Lee C, Hockey R, Ware RS, Dobson AJ. Longitudinal analysis of relationships between social support and general health in an Australian population cohort of young women. Qual Life Res. 2015;24(2):485–92. https://doi.org/10.1007/s11136-014-0774-9.
Barutcu CD, Mert H. The relationship between social support and quality of life in patients with heart failure. J Pak Med Assoc. 2013;63(4):463–7.
Applebaum AJ, Stein EM, Lord-Bessen J, Pessin H, Rosenfeld B, Breitbart W. Optimism, social support, and mental health outcomes in patients with advanced cancer. Psychooncology. 2014;23(3):299–306. https://doi.org/10.1002/pon.3418.
Kornblith AB, Herndon JE 2nd, Zuckerman E, Viscoli CM, Horwitz RI, Cooper MR, et al. Social support as a buffer to the psychological impact of stressful life events in women with breast cancer. Cancer. 2001;91(2):443–54.
Leung J, Pachana NA, McLaughlin D. Social support and health-related quality of life in women with breast cancer: a longitudinal study. Psychooncology. 2014;23(9):1014–20. https://doi.org/10.1002/pon.3523.
Haugland T, Wahl AK, Hofoss D, DeVon HA. Association between general self-efficacy, social support, cancer-related stress and physical health-related quality of life: a path model study in patients with neuroendocrine tumors. Health Qual Life Outcomes. 2016;14:11. https://doi.org/10.1186/s12955-016-0413-y.
Weber BA, Roberts BL, Yarandi H, Mills TL, Chumbler NR, Wajsman Z. The impact of dyadic social support on self-efficacy and depression after radical prostatectomy. J Aging Health. 2007;19(4):630–45. https://doi.org/10.1177/0898264307300979.
Liang Y, Wang H, Niu M, Zhu X, Cai J, Wang X. Longitudinal analysis of the relationships between social support and health-related quality of life in hematopoietic stem cell transplant recipients. Cancer Nurs. 2019;42(3):251–7. https://doi.org/10.1097/ncc.0000000000000616.
Margolis M, Austin J, Wu L, Valdimarsdottir H, Stanton AL, Rowley SD, et al. Effects of social support source and effectiveness on stress buffering after stem cell transplant. Int J Behav Med. 2019;26(4):391–400. https://doi.org/10.1007/s12529-019-09787-2.
Rini C, Redd WH, Austin J, Mosher CE, Meschian YM, Isola L, et al. Effectiveness of partner social support predicts enduring psychological distress after hematopoietic stem cell transplantation. J Consult Clin Psychol. 2011;79(1):64–74. https://doi.org/10.1037/a0022199.
Wells KJ, Booth-Jones M, Jacobsen PB. Do coping and social support predict depression and anxiety in patients undergoing hematopoietic stem cell transplantation? J Psychosoc Oncol. 2009;27(3):297–315. https://doi.org/10.1080/07347330902978947.
Hochhausen N, Altmaier EM, McQuellon R, Davies SM, Papadopolous E, Carter S, et al. Social support, optimism, and self-efficacy predict physical and emotional well-being after bone marrow transplantation. J Psychosoc Oncol. 2007;25(1):87–101. https://doi.org/10.1300/J077v25n01_05.
Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98(2):310–57.
Barata A, Gonzalez BD, Sutton SK, Small BJ, Jacobsen PB, Field T, et al. Coping strategies modify risk of depression associated with hematopoietic cell transplant symptomatology. J Health Psychol. 2018;23(8):1028–37. https://doi.org/10.1177/1359105316642004.
Syrjala KL, Yi JC, Artherholt SB, Romano JM, Crouch ML, Fiscalini AS, et al. An online randomized controlled trial, with or without problem-solving treatment, for long-term cancer survivors after hematopoietic cell transplantation. J Cancer Surviv. 2018;12(4):560–70. https://doi.org/10.1007/s11764-018-0693-9.
Syrjala KL, Yi JC, Langer SL. Psychometric properties of the Cancer and Treatment Distress (CTXD) measure in hematopoietic cell transplantation patients. Psychooncology. 2016;25(5):529–35. https://doi.org/10.1002/pon.3861.
Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW. Can comorbidity be measured by questionnaire rather than medical record review? Med Care. 1996;34(1):73–84.
Syrjala KL, Stover AC, Yi JC, Artherholt SB, Abrams JR. Measuring social activities and social function in long-term cancer survivors who received hematopoietic stem cell transplantation. Psychooncology. 2010;19(5):462–71. https://doi.org/10.1002/pon.1572.
Mitchell PH, Powell L, Blumenthal J, Norten J, Ironson G, Pitula CR, et al. A short social support measure for patients recovering from myocardial infarction: the ENRICHD Social Support Inventory. J Cardpulm Rehabil. 2003;23(6):398–403.
Lotfi-Jam K, Gough K, Schofield P, Aranda S, Jefford M. A longitudinal study of four unique trajectories of psychological distress in cancer survivors after completing potentially curative treatment. Acta Oncol. 2019;58(5):782–9. https://doi.org/10.1080/0284186x.2018.1562209.
Penedo FJ, Traeger L, Benedict C, Thomas G, Dahn JR, Krause MH, et al. Perceived social support as a predictor of disease-specific quality of life in head-and-neck cancer patients. J Support Oncol. 2012;10(3):119–23. https://doi.org/10.1016/j.suponc.2011.09.002.
Johnston MWS, Weinman J. Measures in health psychology: a user’s portfolio. UK: Windsor: NFER-NELSON; 1995.
Syrjala KL, Crouch ML, Leisenring WM, Flowers MED, Artherholt SB, Fiscalini AS, et al. Engagement with INSPIRE, an online program for hematopoietic cell transplantation survivors. Biol Blood Marrow Transplant. 2018;24(8):1692–8. https://doi.org/10.1016/j.bbmt.2018.05.004.
Battiwalla M, Hashmi S, Majhail N, Pavletic S, Savani BN, Shelburne N. National Institutes of Health Hematopoietic Cell Transplantation Late Effects Initiative: developing recommendations to improve survivorship and long-term outcomes. Biol Blood Marrow Transplant. 2017;23(1):6–9. https://doi.org/10.1016/j.bbmt.2016.10.020.
Battiwalla M, Tichelli A, Majhail NS. Reprint of: Long-term survivorship after hematopoietic cell transplantation: roadmap for research and care. Biol Blood Marrow Transplant. 2017;23(3s):S1–s9. https://doi.org/10.1016/j.bbmt.2017.01.001.
Sun CL, Kersey JH, Francisco L, Armenian SH, Baker KS, Weisdorf DJ, et al. Burden of morbidity in 10+ year survivors of hematopoietic cell transplantation: report from the bone marrow transplantation survivor study. Biol Blood Marrow Transplant. 2013;19(7):1073–80. https://doi.org/10.1016/j.bbmt.2013.04.002.
Cohen S, Herbert TB. Health psychology: psychological factors and physical disease from the perspective of human psychoneuroimmunology. Annu Rev Psychol. 1996;47:113–42. https://doi.org/10.1146/annurev.psych.47.1.113.
Acknowledgments
The authors thank all of the HCT survivors who participated in this study.
Author contributions—CRediT taxonomy
Kristina Holmegaard Nørskov: Visualization, methodology, formal analysis, writing original draft, and review and editing.
Jean Yi: Project administration, software, data curation, visualization, formal analysis, validation, writing—review and editing.
Marie-Laure Crouch: Data curation, visualization, writing—review and editing.
Allison Stover Fiscalini: Investigation, data curation, writing—review and editing.
Mary E.D. Flowers: Investigation, writing—review and editing.
Karen Syrjala: Funding acquisition, conceptualization, methodology, investigation, data curation, formal analysis, resources, software, supervision, validation, visualization, conceptualization, methodology, formal analysis, writing—original draft and review and editing.
Funding
Supported by grants from the National Cancer Institute/National Institutes of Health R01 CA112631 and R01 CA215134 to Dr. Syrjala.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
All procedures were approved by the Institutional Review Board of the Fred Hutchinson Cancer Research Center (Fred Hutch).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
The participants provided informed consent regarding publishing their data in this article.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nørskov, K.H., Yi, J.C., Crouch, ML. et al. Social support as a moderator of healthcare adherence and distress in long-term hematopoietic cell transplantation survivors. J Cancer Surviv 15, 866–875 (2021). https://doi.org/10.1007/s11764-020-00979-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-020-00979-4