Abstract
Objectives
This study aimed to reveal the differences in intermediate outcomes between TAR and d-TEVAR in octogenarians and to identify risk factors for adverse events after aortic arch repair in octogenarians.
Methods
We reviewed medical records of 125 patients aged > 80 years who underwent surgical intervention for aortic aneurysm between 2008 and 2016. Of these, 60 underwent conventional TAR (43 men; age, 82 ± 2.2 years) and 65 underwent d-TEVAR (49 men; age, 84 ± 3.4 years).
Results
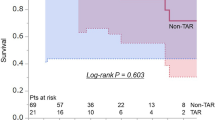
Freedom from all causes of mortality at 2 and 4 years was similar (80 and 66% in TAR, 80 and 51% in d-TEVAR, p = 0.17). Freedom from aortic death at 2 and 4 years was similar (88 and 88% in TAR, 87 and 76% in d-TEVAR, p = 0.86). Using Cox regression analysis, chronic obstructive pulmonary disease (COPD) [hazard ratio (HR), 6.0; p = 0.008], malignancy (HR, 8.8; p = 0.004), previous cardiac and thoracic aortic surgery (required median sternotomy) (HR, 65.9; p = 0.012), perioperative stroke (HR, 12.6; p = 0.012), and postoperative pneumonia (HR, 5.8; p = 0.026) were identified as independent positive predictors of overall postoperative mortality for TAR, whereas neurological dysfunction (HR, 3.0; p = 0.016) and perioperative stroke (HR, 12.1; p = 0.023) were identified for d-TEVAR.
Conclusions
TAR in octogenarians with COPD and/or malignancy showed higher mortality rates; d-TEVAR is more appropriate in these situations. The prevention of perioperative stroke, which is related with poor prognosis in both the groups, is critical.

Similar content being viewed by others
References
Cronenwett JL. Endovascular aneurysm repair: important mid-term results. Lancet. 2005;365:2156–8.
Kazui T, Washiyama N, Muhammad BA, Terada H, Yamashita K, Takinami M, et al. Total arch replacement using aortic arch branched grafts with the aid of antegrade selective cerebral perfusion. Ann Thorac Surg. 2000;70:3–8.
Czerny M, Fleck T, Zimpfer D, Dworschak M, Hofmann W, Hutschala D, et al. Risk factors of mortality and permanent neurologic injury in patients undergoing ascending aortic and arch repair. J Thorac Cardiovasc Surg. 2003;126:1296–1301.
Ferrero E, Ferri M, Viazzo A, Robaldo A, Zingarelli E, Sansone F, et al. Is total debranching a safe procedure for extensive aortic-arch disease? A single experience of 27 cases. Eur J Cardiothorac Surg. 2012;41:177–182.
Murashita T, Matsuda H, Domae K, Iba Y, Tanaka H, Sasaki H, et al. Less invasive surgical treatment for aortic arch aneurysms in high-risk patients: a comparative study of hybrid thoracic endovascular aortic repair and conventional total arch replacement. J Thorac Cardiovasc Surg. 2012;143:1007–13.
Patel RP, Katsargyris A, Verhoeven EL, Adam DJ, Hardman JA. Endovascular aortic aneurysm repair with chimney and snorkel grafts: indications, techniques and results. Cardiovasc Intervent Radiol. 2013;36:1443–51.
Ishimaru S. Endografting of the aortic arch. J Endovasc Ther. 2004;11(Suppl 2):II62-71.
Nashef SA, Roques F, Sharples LD, Nilsson J, Smith C, Goldstone AR, et al. EuroSCORE II. Eur J Cardiothorac Surg. 2012;41:734–44.
Ogino H, Sasaki H, Minatoya K, Matsuda H, Tanaka H, Watanuki H, et al. Evolving arch surgery using integrated antegrade selective cerebral perfusion: impact of axillary artery perfusion. J Thorac Cardiovasc Surg. 2008;136:641–8.
Minatoya K, Ogino H, Matsuda H, Sasaki H, Tanaka H, Kobayashi J, et al. Evolving selective cerebral perfusion for aortic arch replacement: high flow rate with moderate hypothermic circulatory arrest. Ann Thorac Surg. 2008;86:1827–32.
Ogino H, Ando M, Sasaki H, Minatoya K. Total arch replacement using a stepwise distal anastomosis for arch aneurysms with distal extension. Eur J CardiothoracSurg. 2006;29:255–7.
Inoue Y, Matsuda H, Fukuda T, Sanda Y, Morita Y, Oda T, et al. Utility of chimney Stentgraft technique for patients with short zone 1. Ann Vasc Dis. 2015;8:302–6.
Kato M, Kagaya H, Kubo Y, Banno H, Ohkubo N. Real chimney technique for total debranching of supra-aortic trunks. J Vasc Surg. 2015;61:542–5.
Milewski RK, Szeto WY, Pochettino A, Moser GW, Moeller P, Bavaria JE. Have hybrid procedures replaced open aortic arch reconstruction in high-risk patients? A comparative study of elective open arch debranching with endovascular stent graft placement and conventional elective open total and distal aortic arch reconstruction. J Thorac Cardiovasc Surg. 2010;140:590–7.
Pecoraro F, Lachat M, Hofmann M, Cayne NS, Chaykovska L, Rancic Z, et al. Mid-term results of zone 0 thoracic endovascular aneurysm repair after ascending aorta wrapping and supra-aortic debranching in high-risk patients. Interact Cardiovasc Thorac Surg. 2017;24:882–9.
Kurazumi H, Mikamo A, Kudo T, Suzuki R, Takahashi M, Shirasawa B, et al. Aortic arch surgery in octogenarians: is it justified? Eur J Cardiothorac Surg. 2014;46:672–7.
Pacini D, Di Marco L, Leone A, Di Bartolomeo R, Sodeck G, Englberger L, et al. Antegrade selective cerebral perfusion and moderate hypothermia in aortic arch surgery: clinical outcomes in elderly patients. Eur J Cardiothorac Surg. 2012;42:249–53.
Tanaka K, Yoshitaka H, Chikazawa G, Sakaguchi T, Totsugawa T, Tamura K. Investigation of the surgical complications during thoracic endovascular aortic repair: experiences with 148 consecutive cases treated at a single institution in Japan. Surg Today. 2015;45:22–8.
Miyahara S, Miyata H, Motomura N, Takamoto S, Okita Y, Japan Cardiovascular Surgery Database Organization. Clinical significance of chronic obstructive pulmonary disease in patients undergoing elective total arch replacement: analysis based on the Japan Adult Cardiovascular Surgery Database. Eur J Cardiothorac Surg. 2017; 51:761–6.
Cornell TT, Sun L, Hall MW, Gurney JG, Ashbrook MJ, Ohye RG, et al. Clinical implications and molecular mechanisms of immunoparalysis after cardiopulmonary bypass. J Thorac Cardiovasc Surg. 2012;143:1160–6.
Hiraoka K, Kawatsu S, Mori E, Saiki Y. Total aortic arch replacement using hypothermic circulatory arrest with antegrade selective cerebral perfusion: are there cerebral deficits other than frank stroke? Gen Thorac Cardiovasc Surg. 2012;60:345–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflict of interest.
Rights and permissions
About this article
Cite this article
Seike, Y., Matsuda, H., Fukuda, T. et al. Total arch replacement versus debranching thoracic endovascular aortic repair for aortic arch aneurysm: what indicates a high-risk patient for arch repair in octogenarians?. Gen Thorac Cardiovasc Surg 66, 263–269 (2018). https://doi.org/10.1007/s11748-018-0894-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-018-0894-1