Abstract
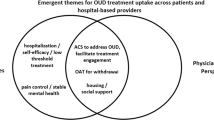
Opioid withdrawal is common among hospitalized patients. Those with substance use disorders exhibit higher rates of patient-directed discharge. The literature lacks information regarding the patient perspective on opioid withdrawal in the hospital setting. In this study, we aimed to capture the patient-reported experience of opioid withdrawal during hospitalization and its impact on the desire to continue treatment for opioid use disorder after discharge. We performed a single-center qualitative study involving semi-structured interviews of hospitalized patients with opioid use disorder (OUD) experiencing opioid withdrawal. Investigators conducted in-person interviews utilizing a combination of open-ended and dichotomous questions. Interview transcripts were then analyzed with open coding for emergent themes. Nineteen interviews were performed. All participants were linked to either buprenorphine (79%) or methadone (21%) at discharge. Eight of nineteen patients (42%) reported a patient-directed discharge during prior hospitalizations. Themes identified from the interviews included: (1) opioid withdrawal was well-managed in the hospital; (2) patients appreciated receiving medication for opioid use disorder (MOUD) for withdrawal symptoms; (3) patients valued and felt cared for by healthcare providers; and (4) most patients had plans to follow-up for opioid use disorder treatment after hospitalization. In this population with historically high rates of patient-directed discharge, patients reported having a positive experience with opioid withdrawal management during hospitalization. Amongst our hospitalized patients, we observed several different individualized MOUD induction strategies. All participants were offered MOUD at discharge and most planned to follow-up for further treatment.

Similar content being viewed by others
Data availability
The authors confirm that the data supporting the findings of this study are available within the article [and/or] its supplementary materials.
References
Weiss AJ, Elixhauser A, Barrett ML, Steiner CA, Bailey MK, O’Malley L (2006) Opioid-Related Inpatient Stays and Emergency Department Visits by State, 2009–2014. 2016 Dec [updated 2017 Jan]. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US). Statistical Brief #219. PMID: 28682575.
Brown AM, White DG, Pharm RB, Adams N, O’Jiaku-Okorie A, Shaikh S, Adegboye A, Lee J, Jackson G, de Frances C (2022) National hospital care survey demonstration projects: characteristics and mortality outcomes of opioid-involved hospital encounters with co-occurring disorders. Nat Health Stat Report 173:1–16
Ronan MV, Herzig SJ (2016) Hospitalizations related to opioid abuse/dependence and associated serious infections increased sharply, 2002–12. Health Aff (Millwood) 35(5):832–837. https://doi.org/10.1377/hlthaff.2015.1424
Peterson C, Xu L, Mikosz CA, Florence C, Mack KA (2018) US hospital discharges documenting patient opioid use disorder without opioid overdose or treatment services, 2011–2015. J Subst Abuse Treat 92:35–39. https://doi.org/10.1016/j.jsat.2018.06.008
Haber PS, Demirkol A, Lange K, Murnion B (2009) Management of injecting drug users admitted to hospital. Lancet 374(9697):1284–1293. https://doi.org/10.1016/s0140-6736(09)61036-9
Ti L, Ti L (2015) Leaving the hospital against medical advice among people who use illicit drugs: a systematic review. Am J Public Health 105(12):e53-59. https://doi.org/10.2105/ajph.2015.302885
Choi M, Kim H, Qian H, Palepu A (2011) Readmission rates of patients discharged against medical advice: a matched cohort study. PLoS ONE 6(9):e24459. https://doi.org/10.1371/journal.pone.0024459
Merchant E, Burke D, Shaw L, Tookes H, Patil D, Barocas JA, Wurcel AG (2020) Hospitalization outcomes of people who use drugs: one size does not fit all. J Subst Abuse Treat 112:23–28. https://doi.org/10.1016/j.jsat.2020.01.010
van Boekel LC, Brouwers EP, van Weeghel J, Garretsen HF (2013) Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend 131(1–2):23–35. https://doi.org/10.1016/j.drugalcdep.2013.02.018
Simon R, Snow R, Wakeman S (2020) Understanding why patients with substance use disorders leave the hospital against medical advice: a qualitative study. Subst Abus 41(4):519–525. https://doi.org/10.1080/08897077.2019.1671942
Crabtree BF, Miller WL (1992) A template approach to text analysis: developing and using codebooks. Doing qualitative research. Sage Publications, Newbury Park, CA, pp 93–109
Yarborough BJ, Stumbo SP, McCarty D, Mertens J, Weisner C, Green CA (2016) Methadone, buprenorphine and preferences for opioid agonist treatment: a qualitative analysis. Drug Alcohol Depend 160:112–118. https://doi.org/10.1016/j.drugalcdep.2015.12.031
Calcaterra SL, Martin M, Bottner R, Englander H, Weinstein Z, Weimer MB, Lambert E, Herzig SJ (2022) Management of opioid use disorder and associated conditions among hospitalized adults: a consensus statement from the society of hospital medicine. J Hosp Med 17(9):744–756. https://doi.org/10.1002/jhm.12893
Calcaterra SL, Lockhart S, Callister C, Hoover K, Binswanger IA (2022) Opioid use disorder treatment initiation and continuation: a qualitative study of patients who received addiction consultation and hospital-based providers. J Gen Intern Med 37(11):2786–2794. https://doi.org/10.1007/s11606-021-07305-3
Silverstein SM, Daniulaityte R, Martins SS, Miller SC, Carlson RG (2019) “Everything is not right anymore”: buprenorphine experiences in an era of illicit fentanyl. Int J Drug Policy 74:76–83. https://doi.org/10.1016/j.drugpo.2019.09.003
Leen JLS, Juurlink DN (2019) Carfentanil: a narrative review of its pharmacology and public health concerns. Can J Anaesth 66(4):414–421. https://doi.org/10.1007/s12630-019-01294-y(Carfentanil:étudenarrativedesapharmacologieetproblématiquesdesantépublique.)
Buresh M, Nahvi S, Steiger S, Weinstein ZM (2022) Adapting methadone inductions to the fentanyl era. J Subst Abuse Treat 141:108832. https://doi.org/10.1016/j.jsat.2022.108832
Moe J, O’Sullivan F, Hohl CM, Doyle-Waters MM, Ronsley C, Cho R, Liu Q, Azar P (2021) Short communication: systematic review on effectiveness of micro-induction approaches to buprenorphine initiation. Addict Behav 114:106740. https://doi.org/10.1016/j.addbeh.2020.106740
Herring AA, Vosooghi AA, Luftig J, Anderson ES, Zhao X, Dziura J, Hawk KF, McCormack RP, Saxon A, D’Onofrio G (2021) High-dose buprenorphine induction in the emergency department for treatment of opioid use disorder. JAMA Netw Open 4(7):e2117128. https://doi.org/10.1001/jamanetworkopen.2021.17128
Ahmadi J, Jahromi MS, Ghahremani D, London ED (2018) Single high-dose buprenorphine for opioid craving during withdrawal. Trials 19(1):675. https://doi.org/10.1186/s13063-018-3055-z
Bromley L, Kahan M, Regenstreif L, Srivastava A, Wyman J (2021) Methadone treatment for people who use fentanyl: recommendations. https://www.metaphi.ca/wp-content/uploads/Guide_MethadoneForFentanyl.pdf. Accessed 14 Sept 2023
Velez CM, Nicolaidis C, Korthuis PT, Englander H (2017) “It’s been an experience, a life learning experience”: a qualitative study of hospitalized patients with substance use disorders. J Gen Intern Med 32(3):296–303. https://doi.org/10.1007/s11606-016-3919-4
Merrill JO, Rhodes LA, Deyo RA, Marlatt GA, Bradley KA (2002) Mutual mistrust in the medical care of drug users: the keys to the “narc” cabinet. J Gen Intern Med 17(5):327–333. https://doi.org/10.1046/j.1525-1497.2002.10625.x
Pauly BB, McCall J, Browne AJ, Parker J, Mollison A (2015) Toward cultural safety: nurse and patient perceptions of illicit substance use in a hospitalized setting. ANS Adv Nurs Sci 38(2):121–135. https://doi.org/10.1097/ans.0000000000000070
Saitz R (2002) Discharges against medical advice: time to address the causes. CMAJ 167(6):647–648
Naeger S, Mutter R, Ali MM, Mark T, Hughey L (2016) Post-discharge treatment engagement among patients with an opioid-use disorder. J Subst Abuse Treat 69:64–71. https://doi.org/10.1016/j.jsat.2016.07.004
Gryczynski J, Nordeck CD, Welsh C, Mitchell SG, O’Grady KE, Schwartz RP (2021) Preventing hospital readmission for patients with comorbid substance use disorder : a randomized trial. Ann Intern Med 174(7):899–909. https://doi.org/10.7326/m20-5475
Weinstein ZM, Cheng DM, D’Amico MJ, Forman LS, Regan D, Yurkovic A, Samet JH, Walley AY (2020) Inpatient addiction consultation and post-discharge 30-day acute care utilization. Drug Alcohol Depend 213:108081. https://doi.org/10.1016/j.drugalcdep.2020.108081
Krawczyk N, Rivera BD, Chang JE, Grivel M, Chen YH, Nagappala S, Englander H, McNeely J (2023) Strategies to support substance use disorder care transitions from acute-care to community-based settings: a scoping review and typology. Addict Sci Clin Pract 18(1):67. https://doi.org/10.1186/s13722-023-00422-w
Barocas JA, Gai MJ, Amuchi B, Jawa R, Linas BP (2020) Impact of medications for opioid use disorder among persons hospitalized for drug use-associated skin and soft tissue infections. Drug Alcohol Depend 215:108207. https://doi.org/10.1016/j.drugalcdep.2020.108207
Jo Y, Nosal R, Vittori A, Cordova L, Vandever C, Alvarez C, Bartholomew TS, Tookes HE (2021) Effect of initiation of medications for opioid use disorder on hospitalization outcomes for endocarditis and osteomyelitis in a large private hospital system in the United States, 2014–18. Addiction 116(8):2127–2134. https://doi.org/10.1111/add.15393
Priest KC, Lovejoy TI, Englander H, Shull S, McCarty D (2020) Opioid agonist therapy during hospitalization within the veterans health administration: a pragmatic retrospective cohort analysis. J Gen Intern Med 35(8):2365–2374. https://doi.org/10.1007/s11606-020-05815-0
Liebschutz JM, Crooks D, Herman D, Anderson B, Tsui J, Meshesha LZ, Dossabhoy S, Stein M (2014) Buprenorphine treatment for hospitalized, opioid-dependent patients: a randomized clinical trial. JAMA Intern Med 174(8):1369–1376. https://doi.org/10.1001/jamainternmed.2014.2556
21 CFR 1306.07, 21 CFR 1406.07—Administering or dispensing of narcotic drugs., n.d., Code of Federal Regulations.
Eaton EF, Westfall AO, McClesky B, Paddock CS, Lane PS, Cropsey KL, Lee RA (2020) In-hospital illicit drug use and patient-directed discharge: barriers to care for patients with injection-related infections. Open Forum Infect Dis 7(3):ofaa074. https://doi.org/10.1093/ofid/ofaa074
Fanucchi LC, Lofwall MR, Nuzzo PA, Walsh SL (2018) In-hospital illicit drug use, substance use disorders, and acceptance of residential treatment in a prospective pilot needs assessment of hospitalized adults with severe infections from injecting drugs. J Subst Abuse Treat 92:64–69. https://doi.org/10.1016/j.jsat.2018.06.011
Huskamp HA, Busch AB, Souza J, Uscher-Pines L, Rose S, Wilcock A, Landon BE, Mehrotra A (2018) How is telemedicine being used in opioid and other substance use disorder treatment? Health Aff (Millwood) 37(12):1940–1947. https://doi.org/10.1377/hlthaff.2018.05134
Weintraub E, Seneviratne C, Anane J, Coble K, Magidson J, Kattakuzhy S, Greenblatt A, Welsh C, Pappas A, Ross TL, Belcher AM (2021) Mobile telemedicine for buprenorphine treatment in rural populations with opioid use disorder. JAMA Netw Open 4(8):e2118487. https://doi.org/10.1001/jamanetworkopen.2021.18487
Hammerslag LR, Mack A, Chandler RK, Fanucchi LC, Feaster DJ, LaRochelle MR, Lofwall MR, Nau M, Villani J, Walsh SL, Westgate PM, Slavova S, Talbert JC (2023) Telemedicine buprenorphine initiation and retention in opioid use disorder treatment for medicaid enrollees. JAMA Netw Open 6(10):e2336914. https://doi.org/10.1001/jamanetworkopen.2023.36914
Funding
1. Mancini Grant, Salt Lake City, Utah 2. Utah Quality Advancement Laboratory (UQuAL), University of Utah, Salt Lake City, Utah.
Author information
Authors and Affiliations
Contributions
All authors participated in the research and preparation of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare they have no conflicts of interest.
Patient consent
All patients gave their consent to participate in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Babbel, D.M., Liu, P., Chen, D.R. et al. Inpatient opioid withdrawal: a qualitative study of the patient perspective. Intern Emerg Med (2024). https://doi.org/10.1007/s11739-024-03604-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11739-024-03604-9