Abstract
Reduction of the inappropriate use of antibiotics in clinical practice is one of the main goals of the Società Italiana di Medicina Interna (SIMI) choosing wisely campaign. We conducted a systematic review of secondary studies (systematic reviews and guidelines) to verify what evidence is available on the duration of antibiotic treatment in Pneumonia. A literature systematic search was performed to identify all systematic reviews and the three most cited and recent guidelines that address the duration of antibiotic therapy in pneumonia. Moreover, a meta-analysis of non-duplicate data from randomized controlled trials (RCTs) considered in the enrolled systematic reviews was performed together with a trial sequential analysis to identify the need for further studies. Two systematic reviews on antibiotic duration in community-acquired pneumonia (CAP) for a total of 17 RCTs (2764 patients) were enrolled in our study. Meta-analysis of non-duplicate RCTs show a non-significant difference in rate of treatment failure between short (≤ 7 days) and long (> 7 days) antibiotic treatment course: RR 1.05 (95% CI, 0.82–1.36). The trial sequential analysis suggests that further data would not affect current evidence or become clinically relevant. Selected guidelines suggest consideration of a short course, with a low grade of evidence and without citing the already published systematic reviews. Antibiotic treatment of CAP for ≤ 7 days is not associated with a higher rate of treatment failure than longer courses and should thus be taken in consideration. Guidelines should upgrade the evidence on this topic.
Similar content being viewed by others
Introduction
In 2012, the American Board of Internal Medicine (ABIM) launched the “Choosing Wisely” (CW) campaign. The aim of the campaign is to promote care that is truly necessary, free of harm, supported by evidence and not duplicative of other tests or procedures already performed, involving both patients and clinicians in the identification and implementation of the campaign’s interventions.
So far, more than 70 scientific societies have joined the campaign, and recently also the Italian Society of Internal Medicine (SIMI) has developed its five items on appropriateness of cures [1]. The SIMI has, nevertheless, chosen a unique way to support the CW Campaign. Indeed, the society uses a bottom-up methodology to select the relevant topics involving not only a small group of experts, but all the society members.
One of the five items of the SIMI CW campaign is the reduction of long-term intravenous antibiotics if not indicated.
Overuse of antimicrobial medications is, indeed, directly related to serious consequences in terms of toxicity, selection of resistant bacteria, patient compliance, and indirectly to financial costs. Recently, the WHO in its “Global action plan on antimicrobial resistance” [2] has also identified optimization of antimicrobial use as one of the five essential objectives to pursuit. This issue seems to be even more relevant if we consider the significant high prevalence of antibiotic prescription that can reach up to 50% of all hospitalized patients [3, 4].
Among the causes for antibiotic prescription, community-acquired pneumonia (CAP) and healthcare-associated pneumonia (HAP) are the most frequent. CAP affects, indeed, both in- and out-hospital patients with an incidence of 5–11 per 1000 in the adult population [5], and an annual calculated cost of 8.4 billion$/year in the United States [6].
The objective of our study is thus to summarize available evidence and to identify fields where further data are needed regarding the following topics on CAP and HAP:
-
1.
Comparison of the efficacy of short- and long-course antibiotic therapy.
-
2.
Optimal timing of switch from intravenous to oral antibiotic therapy.
To do so, we compared guidelines and available systematic reviews on these topics.
Methods
To pursue our objectives, we performed a systematic review of secondary studies. We analyzed all systematic reviews and compared the three most cited guidelines published in the last ten years on antibiotic switch from intravenous to oral therapy and duration of antibiotic treatment in CAP and HAP.
Systematic reviews selection and analysis
For the systematic reviews, we searched the PubMed database 22/12/2017 using the keyword “pneumonia” and filters for Meta-analyses and Systematic Reviews; no publication date limit was applied. We limited our search to English written studies. Two authors (RS, LT) independently screened the articles’ titles and abstracts selecting the ones pertinent to our objectives. Only studies on duration of antibiotic treatment in adult patients with CAP or HAP were included. Rate of agreement among the two authors was evaluated with Cohen’s K coefficient. Disagreements were solved through confrontation between the two reviewers and a third author (GC).
Each selected article was fully evaluated and a pre-specified Excel™ table was used for data extraction. For each systematic review, we recorded authors’ conclusions, number, type and title of original reviewed studies, reported information on and number of enrolled patient (i.e., adult, cancer, surgical, etc.), definition of short- and long-term treatment and of all the outcomes evaluated by the included reviews. For each outcome considered by the systematic reviews, we reported the number of events in short- and long-course therapy groups, and the pooled odds ratio (OR), relative risk (RR) and heterogeneity among studies, as reported by the systematic reviews.
To completely assess the actual evidences on the optimal length of antibiotic treatment, we then considered only the outcome “clinical failure.” We built a two-by-two table for each single trial enrolled in the selected systematic reviews considering the data reported in the descriptive tables of the systematic reviews. We then calculated the risk ratio for the outcome “clinical failure,”, defined as the failure to achieve clinical improvement, and performed a meta-analysis with the data of all non-duplicated RCTs considered in the selected systematic reviews. We took into consideration only the data reported in the systematic reviews, and did not review the original studies.
Results were reported as risk ratio (RR) with 95% confidence interval (CI). A fixed or random effect model was used for analysis as appropriate. Heterogeneity among studies was evaluated with the Cochran’s Q and I2 statistics.
Ultimately, considering the outcome “clinical failure,” we performed a trial sequential analysis (TSA) to properly control the risk of random errors (type I and type II), and to calculate the corresponding required information size (number of participants needed in a meta‐analysis to detect an anticipated treatment effect) [7]. We assumed 8.5% of failure to achieve clinical improvement in the short-course group. This corresponds to the rate of clinical failure observed in our meta-analysis for the short-course treatment group. The required information size was calculated assuming a clinically relevant relative risk reduction of 30%, a risk of type I error of 5% and a risk of type II error of 80%. According to these assumptions, 3894 patients were required for our primary analysis.
Review Manager version 5.3® and the TSA software (Copenhagen Trial Unit Centre for Clinical Intervention Research, Rigshospitalet, Copenhagen, Denmark) were used for performing the meta-analysis and the trial sequential analysis, respectively.
Guidelines selection and analysis
To select the most relevant guidelines, we performed a second search with PubMed using “pneumonia” as keywords and “guidelines” as filter. To include the most updated data, we limited our search between the 12/12/2007 and the 22/12/2017. Two authors (LT, RS) independently screened the studies to include only guidelines on CAP and HAP in adult patients. We also included guidelines on infective diseases that assessed antibiotic treatment in CAP or HAP. Guidelines on the therapy in Ventilator-Associated Pneumonia (VAP) were excluded. Analyses were performed separately for CAP and HAP.
To identify the most relevant guidelines, for each article, we considered a citation-per-year rate that was calculated dividing the guideline’s total number of citations by the difference between the year of our search (i.e., 2017) and the year of the guideline’s publication. The number of citations was obtained from Scopus or Google Scholar considering the highest one among the two databases.
The three guidelines with the highest citation-per-year rate were then enrolled separately for CAP and HAP. Rate of agreement on articles’ selection among the two authors was evaluated with Cohen’s K coefficient. Disagreement among the two reviewers was solved through consultation with a third author (GC).
Consultation with an expert was done before final enrollment to assure that all significant guidelines had been considered.
Both for duration of antibiotic treatment and switch to oral therapy, we compared the three selected guidelines on the recommendations given, the evidence grading system used and the studies cited to support recommendations. If present, we compared evidence among specific subgroups of patients (i.e., hospitalized vs ambulatory ones, different grades of severity).
We finally rated the recommendations given by each guideline with the GRADE system [8] and used this parameter to evaluate the agreement among the different guidelines.
Each analysis was done separately for HAP and CAP.j
Results
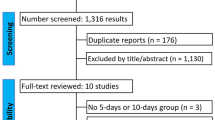
Through bibliographic search in PubMed, we identified 3021 systematic reviews and 2549 guidelines (Appendix Figs. 3 and 4).
Systematic reviews
All abstract and titles of the studies were screened, and six systematic reviews were finally included (Appendix Fig. 3). The two review authors were concordant on the inclusion of 5/6 studies (k = 0.86, very good strength of agreement [8]), the study on which they were discordant was finally included after consultation with a third author. After fully evaluating the articles, only two systematic reviews with meta-analysis on duration of antibiotic treatment in CAP were identified [9, 10] (Table 1). We could not identify any study on the switch to oral therapy in CAP. After evaluation of the full text articles, we could not identify systematic reviews specifically assessing duration of antibiotic treatment and oral switch in HAP. Indeed, all systematic reviews initially included had enrolled only RCTs on VAP, and were thus excluded.
The two selected systematic reviews on CAP considered only RCTs and were performed in in-patients and out-patients.
Dimopoulos et al. [9] enrolled studies on patients with CAP of any severity, either in- or out-patients, of any age (including neonates), and assessing the same antibiotic treatment prescribed for different duration in the two treatment groups. A short course was defined as less than 7 days of antibiotic therapy, while a long course had to be at least two days longer than a short course. The systematic review enrolled five studies on adults [11,12,13,14,15] and two on children [16, 17]. Most enrolled RCTs excluded severe CAP. Antibiotic treatment was given through the oral route in two studies [12, 14], through an intravenous route in one study [11] and initially an intravenous route and then orally in two studies [13, 15]. The short-course treatment ranged between 3 days [13] to a maximum of 7 days [15], while the long-course treatment ranged between 7 [12, 14] and 10 days [11]. The minimum difference between short- and long-course treatment was 2 days in the studies by File et al. [14] and Tellier et al. [12], while 5 days was the longest difference, in the studies by Leophonte [11] and El Moussaoui [13]. Cephalosporins, penicillins or fluoroquinolones were the antibiotics used in the enrolled RCTs, and the same antibiotic had to be used in both treatment groups. Outcomes evaluated were clinical success at the end of therapy (primary outcome), clinical success at follow-up, microbiological success at end of therapy and late follow-up, mortality (secondary outcomes) and total number of adverse events and withdrawals due to adverse events (safety outcomes). Outcomes data were recorded with a per-protocol analysis.
The meta-analyses performed on adults included a total of four studies and 1095 patients who were almost equally distributed between in- and out-patients. No significant difference emerges between short- and long-course antibiotic treatment in clinical success at the end of therapy, with an OR 0.92 (95% CI, 0.58–1.47). Neither, is there any difference found in adverse events. No heterogeneity among studies emerges.
The second systematic review enrolled, by Li et al. [10], included studies on adults both in- and out-patients receiving a short-course (< 7 days) or a long-course (≥ 7 days) antibiotic monotherapy. Antibiotics used were macrolides, beta-lactams, fluoroquinolones, and different types of antibiotics were used in the majority of enrolled RCTs in the short- and long-course treatment arms. Duration of the short-course therapy varied among the enrolled studies from 3 days [18,19,20,21,22,23] to 7 days [12, 15, 24], while in the long-course treatment, it was 10 days for all studies except for the study by Kobayashi et al. [18] where patients were treated for 14 days. The shortest difference in days between short and long treatment was 3 days for the study by Leophonte [24], while the longest was 11 days in the study of Kobayashi et al. [18]. No data on route of administration of antibiotics in the different RCTs were available for this systematic review. Primary outcome evaluated was failure to achieve clinical improvement or cure. Time to outcome evaluation varied among the different enrolled studies from 10 to 42 days. Data were evaluated with both per-protocol and intention-to-treat analyses. The meta-analysis was performed on 15 studies [11, 12, 15, 18,19,20,21,22,23,24,25,26,27,28,29] for a total of 2796 patients. No statistically significant difference is found between short and long course in the risk of clinical failure both with intention to treat (RR 0.89, 95% CI 0.78–1.02) and per-protocol (RR 0.94, 95% CI 0.72–1.22) analyses. In the majority of the studies that used macrolides, a short-course treatment lasted for 3 days, and no statistically significant difference emerges with long-course treatment. Nor was any difference found for adverse events.
No heterogeneity is found among studies.
Three studies were enrolled in both systematic reviews [11, 12, 15].
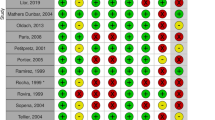
Meta-analysis and trial sequential analysis
For our meta-analysis, we extracted the data of the single RCTs only on adult patients enrolled by the two systematic reviews (Table 2). Considering the enrolled RCTs in the two systematic reviews, our analysis added three further studies [12,13,14], for a total of 917 patients, to the meta-analysis by Li et al. We considered data from 17 RCTs for a total of 2764 patients of whom 1467 were in the short course, and 1297 in the long-course group. Two RCTs had been selected by both studies [11, 15]. Data were analyzed with a per-protocol analysis; since in the study by Dimopoulos, this was the only analysis available. To assess optimal length of antibiotic treatment, we considered as outcome the failure to achieve clinical improvement. We calculated a total of 235 events, 125 in the short-course group and 110 in the long-course group. Meta-analysis on the data from original articles is shown in Fig. 1. No significant difference emerges from short- and long-term antibiotic treatment in risk of clinical failure, with a calculated RR of 1.05 (95% CI, 0.82–1.36). No heterogeneity is found among enrolled studies (I2 = 0%).
As for the TSA, after randomisation of 2764 patients (71% of the required size), the cumulative Z curve lay in the futility area. This means that, in addition to having observed a not statistically significant effect, there is firm evidence that long-course therapy does not reduce the risk for clinical failure by 30%, suggesting that no further trials are needed (Fig. 2).
Trial sequential analysis of non-duplicate enrolled RCTs for the outcome “clinical failure.” The cumulative Z curve (blue line) represents the cumulative evidence for the outcome “clinical failure” in the comparison among short- and long-course antibiotic treatment. Trial sequential monitoring boundaries for benefit or harm (red inward sloping lines) represent the lines above and below which sufficient amount of evidence favouring, respectively, short- and long-course antibiotic treatment have been reached, so that further trials are unlikely to change the conclusions. Futility boundaries (red outward sloping lines) represent the lines below and above which sufficient amount of evidence have been reached on no difference among the two treatment courses, so that addition of future trials is unlikely to change the conclusions. Red vertical line at the right end of the figure represents the sample size above which sufficient amount of evidence favour either short or long antibiotic course and further trials are unlikely to modify conclusions. The green lines represent the conventional boundaries of ≥ 5% equal to Z scores of + 1.96 and − 1.96. The required information size was calculated in 3894 patients, assuming 8.5% of failure to achieve clinical improvement in the short-course group, a clinically relevant relative risk reduction of 30%, a risk of type I error of 5% and a risk of type II error of 80%. In our analysis, the cumulative z score lies in between the futility boundaries suggesting that the long-course antibiotic treatment does not reduce the risk of clinical failure and that future RCTs will unlikely affect current evidence (color figure online)
Guidelines
After screening 2549 articles identified in PubMed, 23 guidelines were identified. Of those, 18 were selected by both reviewer authors (Cohen’s K = 0.78, good strength of agreement [8]), 5 were included after confrontation with a third author, and one, the 2007 Infectious Disease Society of America/American Thoracic Society Guidelines on CAP [30], after consultation with an expert due to the international and epidemiological relevance of the document (Fig. 2).
The most common reasons for articles’ exclusions were type of population (pediatric or immunosuppressed) or pneumonia different from CAP or HAP (i.e., viral pneumonia, VAP, etc.).
Enrolled guidelines on CAP [5, 30, 31] with recorded data on recommendations, level of evidence, GRADE level and bibliography are reported in Table 3.
All guidelines selected were concordant in recommending 7–8 days of antibiotic treatment for CAP even if levels of evidence appeared to be weak and citations provided to support recommendations were different between the guidelines.
All guidelines were also concordant on switching from intravenous to oral therapy as soon as possible; nevertheless, no precise timing nor clear indication, expect from clinical judgment, is provided by any of the selected articles, and the grade of evidence appears to be poor.
Selected guidelines for HAP [56,57,58] all recommend 7–8 days of antibiotic treatment (Appendix Table 4). Evidence quality is very poor as well as GRADE rating. Most recommendations are derived from trials on VAP.
Discussion
The main result of our study is that there are no differences in the incidence of treatment failure between a short- and long-course antibiotic treatment in CAP and that further RCTs would probably not influence these findings. Guidelines’ recommendations are in line with our results even if supported by weak evidence that varies from ours.
No systematic review was found on the switch from intravenous to oral therapy in CAP, while all enrolled guidelines recommend switch as soon as possible according to clinical conditions.
No systematic reviews on antibiotic duration or switch to oral therapy were found for HAP. Guidelines’ recommendations on HAP were derived from RCTs on VAP and were concordant on prescribing antibiotics for 7–8 days, while no indication was found on oral switch.
To our knowledge, this is the first study comparing systematic reviews’ evidence and guidelines recommendations on antibiotic treatment duration and switch to oral therapy in CAP and HAP.
We included in our study only secondary data. This is obviously time and money favorable since data are easily accessible. Nevertheless, it also has the advantage of being able to identify what are the deficiencies of primary and secondary studies, in which direction further RCTs should be headed, and what sort of information still needs to be collected.
No systematic reviews on oral switch were identified while only two systematic reviews on duration of antibiotic treatment in CAP were selected. Neither the meta-analyses of the two systematic reviews nor the meta-analysis that we performed show any differences between short and long-course antibiotic treatment in terms of clinical failure. Moreover, the trial sequential analysis supports the hypothesis that no further trial would probably increase the reliability of our results. Selected guidelines’ recommendations on antibiotic duration in CAP are concordant among them, with the selected meta-analyses and with our results.
Selection of a specific duration for short-course treatment is, nevertheless, more challenging. Both meta-analyses selected a cutoff of 5–7 days, but utilized different types of antibiotics, including macrolides, for which even shorter course might be beneficial. Nevertheless, in the majority of RCTs that used macrolides, the short treatment lasted 3 days, and for each study no statistically significant difference emerges in clinical failure with extended course treatment.
In addition, outcomes prevalence in short- and long-course antibiotic treatment seems to be independent from the route of antibiotic administration. Indeed, in the studies enrolled by Dimopoulos et al. [9], the patients received antibiotics both orally or intravenously, but none of the enrolled RCTs shows a significant differences in outcomes in the two treatment groups.
The results obtained by our study are probably extendable to most of the patients with CAP of everyday clinical practice. Indeed, the population of our study includes patients from different countries, with CAP of different severity (mainly moderate) and aetiology, both in- and out-patients who were treated with the most commonly prescribed antibiotics for CAP (i.e., macrolides, beta-lactams and fluoroquinolones). Recommendations on antibiotic duration in CAP are concordant with the three selected guidelines, with the results of the selected meta-analyses and with our meta-analysis. The quality of evidence is rated poor both by the guidelines’ authors and by the application of the GRADE rating system. We chose to apply the GRADE rating system to compare recommendations with the same evidences’ rating system. Also, the GRADE rating system provides a tool that considers not only the validity of cited studies to support evidence, but also their clinically relevance and applicability in clinical practice.
Interestingly, citations provided in the guidelines are completely different between them, and none includes the meta-analyses that we had selected even if these were published before two of the three selected guidelines [5, 30]. Moreover, only 5 of the 17 RCTs evaluated in our cumulative meta-analysis were cited, even if all were published earlier than all the selected guidelines. It seems that the recommendations of the included guidelines are based on weak evidences even if our trial sequential analysis shows that available evidences on the topic are likely to be conclusive. Although the use of guidelines recommendations to support decisions in clinical practice provides a high confidence even in inexpert physicians, several limitations have been highlighted. Indeed, guidelines’ recommendations are often supported by experts’ opinion rather than by evidence [59], and citations to support recommendations vary significantly between different guidelines on the same subject [60]. Moreover, guidelines are also influenced by conflicts of interest [61].
Our study also underlines that data on HAP are inadequate. No systematic review could be identified on both of our questions and recommendations from guidelines on duration of antibiotic treatment that are derived from studies on VAP.
According to our data, we believe that clinicians should be confident in prescribing a short instead of a long-course antibiotic treatment. This would probably be favorable for patients’ compliance, for risk of adverse events related to the treatment, for non-selection of resistant bacteria, and for reducing economical costs. Definition of the specific duration is probably dependent on the type of antibiotic used. In general, our data suggest that antibiotic treatment of less than 7 days is not associated with more clinical failure than extended treatment, for macrolides shorter courses of even 3 days might be sufficient for resolution of pneumonia.
Our data also suggest that future studies should be directed to the identification of the correct duration of antibiotic treatment and switch to oral therapy in HAP.
Limitations
Study on secondary data has some innate limits. First, data are usually collected in different settings and for different purposes so that bias in selection is amplified at final analysis.
Some of the RCTs included in our meta-analysis used different routes of antibiotic administration. It might be interesting to separate intravenous from oral route of administration in the analysis. This subgroup analysis was not feasible since no data on root of antibiotic administration in the single RCTs were available in the study by Li et al. and we did not review the single RCTs, but only considered the data reported in the selected systematic reviews. Nevertheless, as for clinical failure, our meta-analysis shows no significant heterogeneity among studies, so that inclusion of different types and duration of antibiotic are unlikely to have affected studies results.
One of the main limits of our study is that the included systematic reviews had enrolled studies with different definition and time of evaluation of outcomes. This limit is common to all meta-analyses and systematic reviews. Anyway, none of the RCTs shows statistically significant difference between the two treatments independent of the definition of outcome.
Moreover, in some RCTs, the diagnosis of CAP was made clinically, while in others it needed microbiological and radiological confirmation. However, diagnosis of CAP is usually based on the different combination of a variety of clinical, radiological and microbiological criteria so that inclusion in our study of heterogeneous definitions of CAP might make results more valid for everyday clinical practice.
The most recent systematic review enrolled in our study was published in 2008, so it is possible that, since then, other RCTs have been published on the duration of antibiotic treatment in CAP. Nevertheless, the results of TSA show that no further trials are needed.
Conclusions
In the treatment of CAP, antibiotic therapy for seven or less days is not associated with higher rates of treatment failure than longer courses. Future trials on this topic would probably not affect present evidence. Guidelines on antibiotic duration in CAP are concordant with these findings but supported by weaker evidence and should thus be updated.
Current main guidelines support the switch from intravenous to oral treatment as soon as possible but no clear indication, or strong evidence is yet available.
Nor are clear data available on the optimal duration of antibiotic treatment and timing to oral switch in HAP. Future studies might address these issues.
References
Montano N, Costantino G, Casazza G et al (2016) The Italian Society of Internal Medicine choosing wisely campaign. Intern Emerg Med 11:1125–1130
World Health Organization (2015) Global action plan on antimicrobial resistance. WHO Press, Geneva, pp 1–28
Magill SS, Edwards JR, Beldavs ZG et al (2014) Prevalence of antimicrobial use in US acute care hospitals, May–September 2011. JAMA 312:1438
Fridkin S, Baggs J, Fagan R et al (2014) Vital signs: improving antibiotic use among hospitalized patients. MMWR Morb Mortal Wkly Rep 63:194–200
Lim W, Baudouin S, George R et al (2009) BTS guidelines for the management of community acquired pneumonia in adults: update 2009. Thorax 64:iii1
Niederman MS, McCombs JS, Unger AN et al (1998) The cost of treating community-acquired pneumonia. Clin Ther 20:820–837
Wetterslev J, Jakobsen JC, Gluud C (2017) trial sequential analysis in systematic reviews with meta-analysis. BMC Med Res Methodol 17:39
Altman D (1991) Practical statistics for medical research. Chapman and Hall, Boca Raton
Dimopoulos G, Matthaiou DK, Karageorgopoulos DE et al (2008) Short- versus long-course antibacterial therapy for community-acquired pneumonia: a meta-analysis. Drugs 68:1841–1854
Li JZ, Winston LG, Moore DH, Bent S (2007) Efficacy of short-course antibiotic regimens for community-acquired pneumonia: a meta-analysis. Am J Med 120:783–790
Leophonte P, Choutet P, Gaillat J et al (2002) Efficacy of a ten day course of ceftriaxone compared to shortened five day course in the treatment of community-acquired pneumonia in hospitalised adults with risk factors. Med Mal, Infect, p 32
Tellier G, Niederman MS, Nusrat R et al (2004) Clinical and bacteriological efficacy and safety of 5 and 7 day regimens of telithromycin once daily compared with a 10 day regimen of clarithromycin twice daily in patients with mild to moderate community-acquired pneumonia. J Antimicrob Chemother 54:515–523
el Moussaoui R, de Borgie CAJM, van den Broek P et al (2006) Effectiveness of discontinuing antibiotic treatment after three days versus eight days in mild to moderate-severe community acquired pneumonia: randomised, double blind study. BMJ 332:1355
File TM, Mandell LA, Tillotson G et al (2007) Gemifloxacin once daily for 5 days versus 7 days for the treatment of community-acquired pneumonia: a randomized, multicentre, double-blind study. J Antimicrob Chemother 60:112–120
Siegel RE, Alicea M, Lee A, Blaiklock R (1999) Comparison of 7 versus 10 days of antibiotic therapy for hospitalized patients with uncomplicated community-acquired pneumonia: a prospective, randomized, double-blind study. Am J Ther 6:217–222
Pakistan Multicentre Amoxycillin Short Course Therapy (MASCOT) pneumonia study group (2002) Clinical efficacy of 3 days versus 5 days of oral amoxicillin for treatment of childhood pneumonia: a multicentre double-blind trial. Lancet 360:835–841
Agarwal G, Awasthi S, Kabra SK et al (2004) Three day versus five day treatment with amoxicillin for non-severe pneumonia in young children: a multicentre randomised controlled trial. BMJ 328:791
Kobayashi H (1995) Clarithromycin-controlled randomized double-Blind studies of azithromycin for treatment of pneumonia. Jpn J Chemother 43:757–774
O’Doherty B, Muller O (1998) Randomized, multicentre study of the efficacy and tolerance of azithromycin versus clarithromycin in the treatment of adults with mild to moderate community-acquired pneumonia. Azithromycin Study Group. Eur J Clin Microbiol Infect Dis 17:828–833
Rahav G, Fidel J, Gibor Y, Shapiro M (2004) Azithromycin versus comparative therapy for the treatment of community acquired pneumonia. Int J Antimicrob Agents 24:181–184
Rizzato G, Montemurro L, Fraioli P et al (1995) Efficacy of a three day course of azithromycin in moderately severe community-acquired pneumonia. Eur Respir J 8:398–402
Schönwald S, Barsić B, Klinar I, Gunjaca M (1994) Three-day azithromycin compared with ten-day roxithromycin treatment of atypical pneumonia. Scand J Infect Dis 26:706–710
Sopena N, Martínez-Vázquez C, Rodríguez-Suárez JR et al (2004) Comparative study of the efficacy and tolerance of azithromycin versus clarithromycin in the treatment of community-acquired pneumonia in adults. J Chemother 16:102–103
Léophonte P, File T, Feldman C (2004) Gemifloxacin once daily for 7 days compared to amoxicillin/clavulanic acid thrice daily for 10 days for the treatment of community-acquired pneumonia of suspected pneumococcal origin. Respir Med 98:708–720
Bohte R, van’t Wout JW, Lobatto S et al (1995) Efficacy and safety of azithromycin versus benzylpenicillin or erythromycin in community-acquired pneumonia. Eur J Clin Microbiol Infect Dis 14:182–187
Aprim Brion JP, Sedallian A et al (1990) Azithromycin versus josamycin: treatment of 89 cases of acute pneumonia. Pathol Biol 38:521–525
Dunbar LM, Wunderink RG, Habib MP et al (2003) High-dose, short-course levofloxacin for community-acquired pneumonia: a new treatment paradigm. Clin Infect Dis 37:752–760
Kinasewitz G, Wood RG (1991) Azithromycin versus cefaclor in the treatment of acute bacterial pneumonia. Eur J Clin Microbiol Infect Dis 10:872–877
Schönwald S, Gunjaca M, Kolacny-Babić L et al (1990) Comparison of azithromycin and erythromycin in the treatment of atypical pneumonias. J Antimicrob Chemother 25(Suppl A):123–126
Mandell LA, Wunderink RG, Anzueto A et al (2007) Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis 44(Suppl 2):S27–S72
Woodhead M, Blasi F, Ewig S et al (2011) Guidelines for the management of adult lower respiratory tract infections—full version. Clin Microbiol Infect 17:E1–E59
Capelastegui A, España PP, Quintana JM et al (2008) Declining length of hospital stay for pneumonia and postdischarge outcomes. Am J Med 121:845–852
Jasti H, Mortensen EM, Obrosky DS et al (2008) Causes and risk factors for rehospitalization of patients hospitalized with community-acquired pneumonia. Clin Infect Dis 46:550–556
Yende S, D’Angelo G, Kellum JA et al (2008) Inflammatory markers at hospital discharge predict subsequent mortality after pneumonia and sepsis. Am J Respir Crit Care Med 177:1242–1247
Chastre J, Wolff M, Fagon JY et al (2003) Comparison of 8 vs 15 days of antibiotic therapy for ventilator-associated pneumonia in adults: a randomized trial. J Am Med Assoc 290:2588–2598
Christ-Crain M, Stolz D, Bingisser R et al (2006) Procalcitonin guidance of antibiotic therapy in community-acquired pneumonia: a randomized trial. Am J Respir Crit Care Med 174:84–93
Schuetz P, Christ-Crain M, Thomann R et al (2009) Effect of procalcitonin-based guidelines vs standard guidelines on antibiotic use in lower respiratory tract infections: The ProHOSP randomized controlled trial. JAMA-J Am Med Assoc 302:1059–1066
Bouadma L, Luyt CE, Tubach F et al (2010) Use of procalcitonin to reduce patients’ exposure to antibiotics in intensive care units (PRORATA trial): a multicentre randomised controlled trial. Lancet 375:463–474
Schönwald S, Škerk V, Petričevic I et al (1991) Comparison of three-day and five-day courses of azithromycin in the treatment of atypical pneumonia. Eur J Clin Microbiol Infect Dis 10:877–880
Lee RWW, Lindstrom ST (2007) Early switch to oral antibiotics and early discharge guidelines in the management of community-acquired pneumonia. Respirology 12:111–116
Marras TK, Nopmaneejumruslers C, Chan CKN (2004) Efficacy of exclusively oral antibiotic therapy in patients hospitalized with nonsevere community-acquired pneumonia: a retrospective study and meta-analysis. Am J Med 116:385–393
Van Der Eerden MM, De Graaff CS, Vlaspolder F et al (2004) Evaluation of an algorithm for switching from IV to PO therapy in clinical practice in patients with community-acquired pneumonia. Clin Ther 26:294–303
Shindo Y, Sato S, Maruyama E et al (2008) Implication of clinical pathway care for community-acquired pneumonia in a community hospital: early switch from an intravenous beta-lactam plus a macrolide to an oral respiratory fluoroquinolone. Intern Med 47:1865–1874
Nathan RV, Rhew DC, Murray C et al (2006) In-hospital observation after antibiotic switch in pneumonia: a national evaluation. Am J Med 119:512.e1-7
Oosterheert JJ, Bonten MJM, Schneider MME et al (2006) Effectiveness of early switch from intravenous to oral antibiotics in severe community acquired pneumonia: multicentre randomised trial. BMJ 333:1193
Atlas SJ, Benzer TI, Borowsky LH et al (1998) Safely increasing the proportion of patients with community-acquired pneumonia treated as outpatients: An interventional trial. Arch Intern Med 158:1350–1356
Van Den Brande P, Vondra V, Vogel F et al (1997) Sequential therapy with cefuroxime followed by cefuroxime axetil in community-acquired pneumonia. Chest 112:406–415
Ramirez J, Unowsky J, Talbot GH et al (1999) Sparfloxacin versus clarithromycin in the treatment of community- acquired pneumonia. Clin Ther 21:103–117
MacGregor RR, Graziani AL (1997) Oral administration of antibiotics: a rational alternative to the parenteral route. Clin Infect Dis 24:457–467
Mandell LA, Bergeron MG, Gribble MJ et al (1995) Sequential antibiotic therapy: effective cost management and patient care. Can J Infect Dis 6:306–315
Nathwani D (1998) Sequential switch therapy for lower respiratory tract infections: a european perspective. Chest 113:211S–218S
Ramirez JA, Srinath L, Ahkee S et al (1995) Early switch from intravenous to oral cephalosporins in the treatment of hospitalized patients with community-acquired pneumonia. Arch Intern Med 155:1273–1276
Castro-Guardiola A, Viejo-Rodríguez A-L, Soler-Simon S et al (2001) Efficacy and safety of oral and early-switch therapy for community-acquired pneumonia: a randomized controlled trial. Am J Med 111:367–374
Ramirez JA, Bordon J (2001) Early switch from intravenous to oral antibiotics in hospitalized patients with bacteremic community-acquired Streptococcus pneumoniae pneumonia. Arch Intern Med 161:848–850
Ramirez JA, Vargas S, Ritter GW et al (1999) Early switch from intravenous to oral antibiotics and early hospital discharge: a prospective observational study of 200 consecutive patients with community-acquired pneumonia. Arch Intern Med 159:2449–2454
Rotstein C, Evans G, Born A et al (2008) Clinical practice guidelines for hospital-acquired pneumonia and ventilator-associated pneumonia in adults. Can J Infect Dis Med Microbiol = J Can des Mal Infect la Microbiol médicale/AMMI Canada 19:19–53
Torres A, Niederman MS, Chastre J et al (2017) International ERS/ESICM/ESCMID/ALAT guidelines for the management of hospital-acquired pneumonia and ventilator-associated pneumonia. Eur Respir J 50:1700582
Kalil AC, Metersky ML, Klompas M et al (2016) Management of Adults with hospital-acquired and ventilator-associated pneumonia: 2016 Clinical practice guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis 63:e61–e111
McAlister FA, van Diepen S, Padwal RS et al (2007) How evidence-based are the recommendations in evidence-based guidelines? PLoS Med 4:e250
Burgers JS, Bailey JV, Klazinga NS et al (2002) Inside guidelines: comparative analysis of recommendations and evidence in diabetes guidelines from 13 countries. Diabetes Care 25:1933–1939
Eichacker PQ, Natanson C, Danner RL (2006) Surviving sepsis—practice guidelines, marketing campaigns, and Eli Lilly. N Engl J Med 355:1640–1642
Dennesen PJW, Van der Ven AJAM, Kessels AGH et al (2001) Resolution of infectious parameters after antimicrobial therapy in patients with ventilator-associated pneumonia. Am J Respir Crit Care Med 163:1371–1375
Ibrahim EH, Ward S, Sherman G et al (2001) Experience with a clinical guideline for the treatment of ventilator-associated pneumonia. Crit Care Med 29:1109–1115
Micek ST, Ward S, Fraser VJ, Kollef MH (2004) A randomized controlled trial of an antibiotic discontinuation policy for clinically suspected ventilator-associated pneumonia. Chest 125:1791–1799
Luna CM, Blanzaco D, Niederman MS et al (2003) Resolution of ventilator-associated pneumonia: prospective evaluation of the clinical pulmonary infection score as an early clinical predictor of outcome. Crit Care Med 31:676–682
Dimopoulos G, Poulakou G, Pneumatikos IA et al (2013) Short- vs long-duration antibiotic regimens for ventilator-associated pneumonia: a systematic review and meta-analysis. Chest 144:1759–1767
Pugh R, Grant C, Cooke RP et al (2015) Short-course versus prolonged-course antibiotic therapy for hospital-acquired pneumonia in critically ill adults. Cochrane Database Syst Rev 8:CD007577
Capellier G, Mockly H, Charpentier C et al (2012) Early-onset ventilator-associated pneumonia in adults randomized clinical trial: comparison of 8 versus 15 days of antibiotic treatment. PLoS One 7:e41290
Fekih Hassen M, Ayed S, Ben Sik Ali H et al (2009) Durée de l’antibiothérapie lors du traitement des pneumopathies acquises sous ventilation mécanique : comparaison entre sept jours et dix jours. Étude pilote. Ann Fr Anesth Reanim 28:16–23
Kollef MH, Sherman G, Ward S, Fraser VJ (1999) Inadequate antimicrobial treatment of infections: a risk factor for hospital mortality among critically ill patients. Chest 115:462–74
Medina JC, Perez Protto SE, Paciel D et al (2007) Antibiotic treatment for the ventilator-associated pneumonia: 8 vs.12 days randomized trial preliminary data. Annual Interscience Conference on Antimicrobial Agents and Chemotherapy, Chicago, IL, 2007
Singh N, Rogers P, Atwood CW et al (2000) Short-course empiric antibiotic therapy for patients with pulmonary infiltrates in the intensive care unit: a proposed solution for indiscriminate antibiotic prescription. Am J Respir Crit Care Med 162:505–511
Acknowledgments
We would like to thank all the members of the SIMI Choosing Wisely Group for their help in the writing of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human and animal rights
This article does not contain any study with human participants or animals performed by any of the authors.
Informed Consent
No informed consent was required for the study.
Rights and permissions
About this article
Cite this article
Furlan, L., Erba, L., Trombetta, L. et al. Short- vs long-course antibiotic therapy for pneumonia: a comparison of systematic reviews and guidelines for the SIMI Choosing Wisely Campaign. Intern Emerg Med 14, 377–394 (2019). https://doi.org/10.1007/s11739-018-1955-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-018-1955-2