Abstract
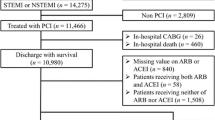
Antiplatelet drugs, statins, angiotensinogen-converting enzyme inhibitors or angiotensin-II receptor blockers, and β-blockers improve survival following myocardial infarction (MI). However, in old age they are under-prescribed, and their effectiveness in combination regimens is unproven. The aim of the study was to evaluate prescription of recommended cardiovascular drug classes and impact of a combination regimen on long-term mortality and hospitalizations. Records of 65+ years MI survivors, discharged from hospitals in four Local Health Units in Italy, were selected from administrative databases and analyzed. All-cause mortality and cardiovascular re-hospitalization in 12 months were compared across participants prescribed 0, 1, 2, 3, or 4 recommended drug classes. Out of 2626 participants (56 % men, 25 % aged 85+ years), 42 % were prescribed all, 14 % none of the recommended drug classes. The prescription rate decreased with advancing age. At all ages, mortality decreased with increasing number of drug classes prescribed: in participants aged 85+ years, adjusted hazard ratios (95 % confidence interval) for death were 0.74 (0.47–1.17), 0.52 (0.33–0.82), 0.30 (1.19–0.48), and 0.33 (0.20–0.53) for 1, 2, 3, and 4 classes prescribed, compared with none. The risk of cardiovascular re-hospitalizations decreased with an increasing number of drug classes prescribed through the age of 84 years. After MI, a combination regimen of recommended drug classes prevents long-term mortality at any age, and cardiovascular re-hospitalizations through the age of 84. Enhancing compliance with treatment guidelines may reduce the burden of mortality and hospitalizations in older MI survivors.

Similar content being viewed by others
References
Ryan TJ, Anderson JL, Antman EM, Braniff BA, Brooks NH, Califf RM et al (1996) ACC/AHA guidelines for the management of patients with acute myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute myocardial infarction). J Am Coll Cardiol 28:1328–1428
Braunwald E, Antman EM, Beasley JW, Califf RM, Cheitlin MD, Hochman JS et al (2002) ACC/AHA 2002 guideline update for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients With Unstable Angina). Circulation 106:1893–1900
Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M et al (2004) ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction; A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of patients with acute myocardial infarction). J Am Coll Cardiol 44:E1–E211
Smith SC Jr, Benjamin EJ, Bonow RO, Braun LT, Creager MA, Franklin BA et al (2011) AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation endorsed by the World Heart Federation and the Preventive Cardiovascular Nurses Association. J Am Coll Cardiol 58:2432–2446
MI—secondary prevention. Secondary prevention in primary and secondary care for patients following a myocardial infarction. Partial update of NICE CG48. National Clinical Guideline Centre, 2013
Amsterdam EA, Wenger NK, Brindis RG, Casey DE Jr, Ganiats TG, Holmes DR Jr et al (2014) 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 64:e139–e228
Setoguchi S, Glynn RJ, Avorn J, Levin R, Winkelmayer WC (2007) Ten-year trends of cardiovascular drug use after myocardial infarction among community-dwelling persons 65 years of age. Am J Cardiol 100:1061–1067
Rasmussen JN, Chong A, Alter DA (2007) Relationship between adherence to evidence-based pharmacotherapy and long-term mortality after acute myocardial infarction. JAMA 297:177–186
Sokol MC, McGuigan KA, Verbrugge RR (2005) Impact of medication adherence on hospitalization risk and healthcare cost. Med Care 43:521–530
Brown TM, Voeks JH, Bittner V, Brenner DA, Cushman M, Goff DC Jr, Glasser S et al (2014) Achievement of optimal medical therapy goals for U.S. adults with coronary artery disease. Results from the REGARDS study. J Am Coll Cardiol 63:1626–1633
Filippi A, D’Ambrosio Giustini SE, Pecchioli S, Mazzaglia G, Cricelli C (2001) Pharmacological treatment after acute myocardial infarction from 2001 to 2006: a survey in Italian primary care. J Cardiovasc Med 2009(10):714–718
Di Bari M, Balzi D, Roberts AT, Barchielli A, Fumagalli S, Ungar A et al (2010) Prognostic stratification of folder persons based on simple administrative data: development and validation of the “Silver Code”, to be used in emergency department triage. J Gerontol A Biol Sci Med 65:159–164
Ministero del Lavoro, della Salute e delle Politiche Sociali. Rapporto annuale sulle attività di ricovero ospedaliero. Anno 2005. http://www.ministerosalute.it/programmazione/sdo/sezDocumenti.jsp?id=148&label=osp. Accessed 24 April 2009
Zeymer U, James S, Berkenboom G, Mohacsi A, Iñiguez A, Coufal Z et al (2013) Differences in the use of guideline-recommended therapies among 14 European countries in patients with acute coronary syndromes undergoing PCI. Eur J Prev Cardiol 20:218–228
Tay EL, Chan M, Tan V, Sim LL, Tan HC, Cheng YT (2008) Impact of combination evidence-based medical therapy on mortality following myocardial infarction in elderly patients. Am J Geriatr Cardiol 17:21–26
Lee HY, Cooke CE, Robertson TA (2008) Use of secondary prevention drug therapy in patients with acute coronary syndrome after hospital discharge. J Manag Care Pharm 14(3):271–280
Hamood H, Hamood R, Green MS, Almog R (2015) Determinants of adherence to evidence-based therapy after acute myocardial infarction. Eur J Prev Cardiol (epub ahead of print)
Lee PY, Alexander KP, Hammill BG, Pasquali SK, Peterson ED (2001) Representation of elderly persons and women in published randomized trials of acute coronary syndromes. JAMA 286:708–713
Dodd KS, Saczynski JS, Zhao Y, Goldberg RJ, Gurwitz JH (2011) Exclusion of older adults and women from recent trials of acute coronary syndromes. J Am Geriatr Soc 59:506–511
Di Bari M, Pahor M, Franse L, Shorr RI, Wan JY, Ferrucci L et al (2001) Dementia and disability outcomes in large hypertension trials: lessons learned from the systolic hypertension in the elderly program (SHEP) trial. Am J Epidemiol 153:73–78
Cherubini A, Del Signore S, Ouslander J, Semla T, Michel JP (2010) Fighting against age discrimination in clinical trials. J Am Geriatr Soc 58:1791–1796
Pinnarelli L, Mayer F, Bauleo L, Agabiti N, Kirchmayer U, Belleudi V et al (2015) Adherence to antiplatelet therapy after percutaneous coronary intervention: a population study in a region of Italy. J Cardiovasc Med 16:230–237
Black N (1996) Why we need observational studies to evaluate the effectiveness of health care. BMJ 312:1215–1218
Pereira M, Araújo C, Dias P, Lunet N, Subirana I, Marrugat J et al (2014) Age and sex inequalities in the prescription of evidence-based pharmacological therapy following an acute coronary syndrome in Portugal: the EURHOBOP study. Eur J Prev Cardiol 21:1401–1408
Nauta ST, Deckers JW, Akkerhuis KM. Age-dependent care and long-term (20-year) mortality of 14,434 myocardial infarction patients: Changes from 1985 to 2008. Int J Cardiol 167:693–7
Alexander KP, Roe MT, Chen AY, Lytle BL, Pollack CV Jr, Foody JM, CRUSADE Investigators et al (2005) Evolution in cardiovascular care for elderly patients with non-ST-segment elevation acute coronary syndromes: results from the CRUSADE national quality improvement initiative. J Am Coll Cardiol 46:1479–1487
Bernat JL (2005) Medical futility: definition, determination, and disputes in critical care. Neurocrit Care 2:198–205
Wirth R, Sieber CC (2012) Health care professionals underestimate the mean life expectancy of older people. Gerontology 58:56–59
Di Bari M, Balzi D, Fracchia S, Barchielli A, Orso F, Sori A et al (2014) Decreased utilization and increased effectiveness of percutaneous coronary intervention in complex older patients with acute coronary syndromes. Heart. doi:10.1136/heartjnl-2013-305445
Butler RN (1982) The triumph of age: science, gerontology, and ageism. Bull N Y Acad Med 58:347–361
Onder G, Bonassi S, Abbatecola AM, Folino-Gallo P, Lapi F, Marchionni N et al (2014) Geriatrics working group of the Italian medicines agency (AIFA). High prevalence of poor quality drug prescribing in older individuals: a nationwide report from the Italian medicines agency (AIFA). J Gerontol A Biol Sci Med Sci 69:430–437
Degli Esposti L, Saragoni S, Benemei S, Batacchi P, Geppetti P, Di Bari M et al (2011) Adherence to antihypertensive medications and health outcomes among newly treated hypertensive patients. ClinicoEcon Outcomes Res 3:47–54
Acknoweldgements
Funding
This study is supported by an unrestricted grant by the non-profit Sanofi Aventis Foundation (Milan, Italy). The sponsor played no role in the design of the study, analysis or interpretation of findings, nor in the preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
MS is General Director of the non-profit Sanofi Aventis Foundation (Milan, Italy). All the other authors have no competing interests that relate to this manuscript.
Statement of human and animal rights
The study was approved by local ethics committees
Informed consent
According to Italian laws, informed consent was not required, as the study was based upon administrative, anonymized data.
Rights and permissions
About this article
Cite this article
Di Bari, M., Esposti, L.D., Veronesi, C. et al. Combination evidence-based therapy is effective in the oldest ‘old patients’ following myocardial infarction. The “Salute e Benessere nell’Anziano” (SeBA) observational study. Intern Emerg Med 11, 677–685 (2016). https://doi.org/10.1007/s11739-016-1391-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-016-1391-0