Abstract
Purpose
Transportation, access to follow-up care, and association with weight loss are understudied in the bariatric population. The objective of this study was to determine how transportation variables associate with postoperative attendance and weight loss through 24 months.
Materials and Methods
Seven hundred eighty-seven patients (81.3% female; 59.1% White) who had primary surgery (48.6% gastric bypass) from 2015 to 2019 were included. Sidewalk coverage and number of bus stops from patients’ homes, driving distance in miles and minutes from patients’ homes to the nearest bus stop and the clinic were measured. Bivariate analyses were conducted with the transportation variables and attendance and %TWL at 2 or 3, 6, 12, and 24 months. One mixed multilevel model was conducted with dependent variable %TWL over 24 months with visits as the between-subjects factor and covariates: race, insurance, surgical procedure, and driving distance to the clinic in minutes, attendance, and %TWL over 24 months; an interaction between distance, attendance, and visits.
Results
There were no significant differences between the majority of the transportation variables and postoperative attendance or %TWL. Patients who had perfect attendance had improved %TWL at 12 months [t(534)=−1.92, p=0.056] and 24 months [t(393)=−2.69, p=0.008] compared to those who missed at least one appointment. Patients with perfect attendance and who had shorter driving times (under 20 min) to the clinic had greater weight loss through 24 months [F(10, 1607.50)=2.19, p=0.016)].
Conclusions
Overall, transportation factors were not associated with attendance and weight loss, with the exception of the interaction between shorter driving minutes to follow-up and perfect attendance.
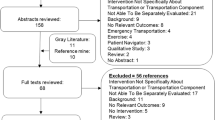
Graphical Abstract

Similar content being viewed by others
References
Spaniolas K, Kasten KR, Celio A, et al. Postoperative follow-up after bariatric surgery: effect on weight loss. Obes Surg. 2016;26(4):900–3. https://doi.org/10.1007/s11695-016-2059-6.
Kim HJ, Madan A, Fenton-Lee D. Does patient compliance with follow-up influence weight loss after gastric bypass surgery? A systematic review and meta-analysis. Obes Surg. 2014;24(4):647–51. https://doi.org/10.1007/s11695-014-1178-1.
Weiner JP, Bandeian S, Hatef E, et al. In-person and telehealth ambulatory contacts and costs in a large US insured cohort before and during the COVID-19 pandemic. JAMA Netw Open. 2021;4(3):e212618. https://doi.org/10.1001/jamanetworkopen.2021.2618.
Liu N, Venkatesh M, Hanlon BM, et al. Association between medicaid status, social determinants of health, and bariatric surgery outcomes. Ann Surg Open. 2021;2(1):e028. https://doi.org/10.1097/AS9.0000000000000028.
Murtha JA, Venkatesh M, Liu N, et al. Association between neighborhood environments and bariatric surgery outcomes. SOARD. 2022;18(12):1357–64. https://doi.org/10.1016/j.soard.2022.08.007.
Reid RE, Carver TE, Reid TG, et al. Effects of neighborhood walkability on physical activity and sedentary behavior long-term post-bariatric surgery. OBES SURG. 2017;27:1589–94. https://doi.org/10.1007/s11695-016-2494-4.
Funk LM, Alagoz E, Murtha JA, et al. Socioeconomic disparities and bariatric surgery outcomes: a qualitative analysis. Am J Surg. 2023;225(4):609–14. https://doi.org/10.1016/j.amjsurg.2022.09.049.
Kurz D, Befort C, Ose J. Travel burden in a rural primary care behavioral weight loss randomized trial: impact on visit attendance and weight loss. J Rural Health. 2022;38:980–5. https://doi.org/10.1111/jrh.12652.
Monfared S, Martin A, Selzer D, et al. Travel distance reduces follow-up compliance but has no effect on long-term weight loss success in bariatric patients. Surg Endosc. 2021;35(4):1579–83. https://doi.org/10.1007/s00464-020-07535-2.
Compher CW, Hanlon A, Kang Y, et al. Attendance at clinical visits predicts weight loss after gastric bypass surgery. Obes Surg. 2012;22(6):927–34. https://doi.org/10.1007/s11695-011-0577-9.
Jennings N, Boyle M, Mahawar K, et al. The relationship of distance from the surgical centre on attendance and weight loss after laparoscopic gastric bypass surgery in the United Kingdom. Clin Obes. 2013;3(6):180–4. https://doi.org/10.1111/cob.12031.
Lujan J, Tuero C, Landecho MF, et al. Impact of routine and long-term follow-up on weight loss after bariatric surgery. Obes Surg. 2020;30(11):4293–9. https://doi.org/10.1007/s11695-020-04788-7.
Martin DJ, Lee CM, Rigas G, Tam CS. Weight loss 2 years after LSG. Asian J Endosc Surg. 2015;8:328–32. https://doi.org/10.1111/ases.12193.
Shilton H, Gao Y, Nerlekar N, Evennett N, Ram R, Beban G. Pre-operative bariatric clinic attendance is a predictor of post-operative clinic attendance and weight loss outcomes. Obes Surg. 2019;29(7):2270–5. https://doi.org/10.1007/s11695-019-03843-2.
Pratt KJ, Hanks AS, Miller HJ, et al. The BARI-hoods Project: neighborhood social determinants of health and postoperative weight loss using integrated electronic health record, census, and county data. SOARD. 2023; https://doi.org/10.1016/j.soard.2022.12.033.
Brethauer SA, Kim J, el Chaar M, et al. ASMBS Clinical Issues Committee. Standardized outcomes reporting in metabolic and bariatric surgery. Surg Obes Relat Dis. 2015;11(3):489–506. https://doi.org/10.1016/j.soard.2015.02.003.
Gunn LD, King TL, Mavoa S, et al. Identifying destination distances that support walking trips in local neighborhoods. J Transp Health. 2017;5:133–41.
Boehmer TK, Hoehner CM, Deshpande AD, et al. Perceived and observed neighborhood indicators of obesity among urban adults. Int J Obes. 2007;31(6):968–77.
Raudenbush SW, Bryk AS. Hierarchical linear models: applications and data analysis methods, vol. 1. California: Sage; 1992.
Vosburg RW, Robinson KA, Gao C, Kim JJ. Patient and provider satisfaction with telemedicine in a comprehensive weight management program. Telemed J E Health. 2022;28(3):384–90. https://doi.org/10.1089/tmj.2021.0077.
Funding
This study was funded by The Ohio State University Center for Clinical and Translational Sciences Artificial Intelligence and Machine Learning in Translational Science and Human Health Pilot Grant. 06/2021-05/2022. Pratt KJ (PI); Co-Is: Focht BC, Hanks A, Noria S, Outrich M. 06/2021-05/2022. Integrating Multiple Data Sources to Identify Bariatric Surgical Disparities in Franklin County.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
For this type of study, formal consent is not required.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• There were no significant differences between the majority of the transportation variables and attendance or %TWL at any of the postoperative assessments.
• Patients who had perfect attendance through 24 months had improved %TWL at 12 months and 24 months compared to those who missed at least one appointment.
• Patients with perfect attendance and who had shorter driving times (under 20 min) to the clinic had greater weight loss through 24 months.
• Future research should consider how telemedicine visits may aid patients with greater travel times and more socioeconomic need.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pratt, K.J., Miller, H.J., Hanks, A.S. et al. Transportation Factors and Postoperative Attendance and Weight Loss Through 24 Months. OBES SURG 34, 114–122 (2024). https://doi.org/10.1007/s11695-023-06906-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-023-06906-7