Abstract
Purpose
Vitamin C (VC) is implicated in many physiological pathways. Vitamin C deficiency (VCD) can compromise the health of patients with metabolic and bariatric surgery (patients). As symptoms of VCD are elusive and data on VCD in patients is scarce, we aim to characterize patients with measured VC levels, investigate the association of VCD with other lab abnormalities, and create predictive models of VCD using machine learning (ML).
Methods
A retrospective chart review of patients seen from 2017 to 2021 at a tertiary care center in Northeastern USA was conducted. A 1:4 case mix of patients with VC measured to a random sample of patients without VC measured was created for comparative purposes. ML models (BayesNet and random forest) were used to create predictive models and estimate the prevalence of VCD patients.
Results
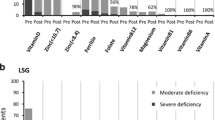
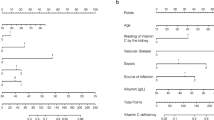
Of 5946 patients reviewed, 187 (3.1%) had VC measures, and 73 (39%) of these patients had VC<23 μmol/L(VCD. When comparing patients with VCD to patients without VCD, the ML algorithms identified a higher risk of VCD in patients deficient in vitamin B1, D, calcium, potassium, iron, and blood indices. ML models reached 70% accuracy. Applied to the testing sample, a “true” VCD prevalence of ~20% was predicted, among whom ~33% had scurvy levels (VC<11 μmol/L).
Conclusion
Our models suggest a much higher level of patients have VCD than is reflected in the literature. This indicates a high proportion of patients remain potentially undiagnosed for VCD and are thus at risk for postoperative morbidity and mortality.
Graphical abstract





Similar content being viewed by others
References
Johnson LE. Vitamin C Deficiency. Merck & Co., Inc. 2022; [cited 2022 Oct 9]. Available from: https://www.merckmanuals.com/professional/nutritional-disorders/vitamin-deficiency,-dependency,-and-toxicity/vitamin-c-deficiency.
Nosewicz J, Spaccarelli N, Roberts KM, et al. The epidemiology, impact, and diagnosis of micronutrient nutritional dermatoses part 1: Zinc, selenium, copper, vitamin A, and vitamin C. J Am Acad Dermatol. 2022;86(2):267–78.
Hansen EP, Metzsche C, Henningsen E, Toft P. Severe scurvy after gastric bypass surgery and a poor postoperative diet. J Clin Med Res. 2012;4(2):135.
Riess KP, Farnen JP, Lambert PJ, Mathiason MA, Kothari SN. Ascorbic acid deficiency in bariatric surgical population. Surg Obes Relat Dis. 2009;5(1):81–6.
Padayatty SJ, Levine M. Vitamin C: the known and the unknown and Goldilocks. Oral Dis. 2016;22(6):463–93.
Spoelstra-de Man A, Oudemans-van Straaten H, Elbers P. Vitamin C and thiamine in critical illness. BJA Education. 2019;19(9):290.
Rowe S, Carr AC. Global vitamin C status and prevalence of deficiency: a cause for concern? Nutrients. 2020;12(7).
Khalife R, Grieco A, Khamisa K, Tinmouh A, McCudden C, Saidenberg E. Scurvy, an old story in a new time: the hematologist’s experience. Blood Cells Mol Dis. 2019;76:40–4.
Hemila H, Chalker E. Vitamin C can shorten the length of stay in the ICU: a meta-analysis. Nutrients. 2019;11(4):708.
Carr AC, Rowe S. The emerging role of vitamin C in the prevention and treatment of COVID-19. Nutrients. 2020;12(11).
Carr Ac MC. The role of vitamin C in the treatment of pain: new insights. J Transl Med. 2017;15(1):77.
Carr AC, Cook J. Intravenous vitamin C for cancer therapy - identifying the current gaps in our knowledge. Front Physiol. 2018;9:1182.
D'Aniello C, Cermola F, Patriarca EJ, Minchiotti G. Vitamin C in stem cell biology: impact on extracellular matrix homeostasis and epigenetics. Stem Cells Int. 2017;2017:8936156.
Dosedel M, Jirkovsky E, Macakova K, et al. Vitamin C-sources, physiological role, kinetics, deficiency, use, toxicity, and determination. Nutrients. 2021;13(2):615.
Maxfield L, Crane JS. Vitamin C deficiency. In: StatPearls [Internet]. Treasure Island (FL): StatPearls; 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK493187/.
Crandon JH, Landau B, Mikal S, Balmanno J, Jefferson M, Mahoney N. Ascorbic acid economy in surgical patients as indicated by blood ascorbic acid levels. N Engl J Med. 1958;258(3):105–13.
Lewis CA, de Jersey S, Hopkins G, Hickman I, Osland E. Does bariatric surgery cause vitamin A, B1, C or E deficiency? A systematic review. Obes Surg. 2018;28:3640–57.
Hujoel PP, Hujoel MLA. Vitamin C and scar strength: analysis of a historical trial and implications for collagen-related pathologies. Am J Clin Nutr. 2022;115(1):8–17.
Travica N, Ried K, Hudson I, Scholey A, Pipingas A, Sali A. The effects of surgery on plasma/serum vitamin C concentrations: a systematic review and meta-analysis. Br J Nutr. 2020;4:1–39.
Boulesteix AL, Schmid M. Machine learning versus statistical modeling. Biom J. 2014;56(4):588–93.
Lalehzarian SP, Gowd AK, Liu JN. Machine learning in orthopaedic surgery. World J Orthop. 2021;12(9):685.
Balch JA, Delitto D, Tighe PJ, et al. Machine learning applications in solid organ transplantation and related complications. Front Immunol. 2021;3707:739728.
Hashimoto DA, Rosman G, Rus D, Meireles OR. Artificial intelligence in surgery: promises and perils. Annals of Surgery. 2018;268(1):70–6.
Peloso A, Moeckli B, Delaune V, Oldani G, Andres A, Compagnon P. Artificial intelligence: present and future potential for solid organ transplantation. Transpl Int. 2022;35:10640.
Olier I, Ortega-Martorell S, Pieroni M, Lip GY. How machine learning is impacting research in atrial fibrillation: implications for risk prediction and future management. Cardiovasc Res. 2021;117(7):1700–17.
Collins GS, Reitsma JB, Altman DG, Moons KG. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD Statement. BMC Med. 2015;6(13):1.
Parrott J, Frank L, Rabena R, Craggs-Dino L, Isom KA, Greiman L. American Society for Metabolic and Bariatric Surgery Integrated Health Nutritional Guidelines for the Surgical Weight Loss Patient 2016 Update: micronutrients. Surg Obes Relat Dis. 2017;13(5):727–41.
Camaschella C, Girelli D. The changing landscape of iron deficiency. Mol Aspects Med. 2020;75:100861.
Cappellini MD, Comin-Colet J, de Francisco A, Dignass A, Doehner W, Lam CS, et al. Iron deficiency across chronic inflammatory conditions: international expert opinion on definition, diagnosis, and management. Am J Hematol. 2017;92(10):1068–78.
Cappellini MD, Musallam KM, Taher AT. Iron deficiency anaemia revisited. J Intern Med. 2020;287(2):153–70.
Benotti PN, Wood GC, Dove JT, et al. Iron deficiency is highly prevalent among candidates for metabolic surgery and may affect perioperative outcomes. Surg Obes Relat Dis. 2021;17:1692–9.
Fertrin KY. Diagnosis and management of iron deficiency in chronic inflammatory conditions (CIC): is too little iron making your patient sick? Hematology Am Soc Hematol Educ Program. 2020;2020(1):478–86.
Galar M, Fernandez A, Barrenechea E, Bustince H, Herrera F. A review on ensembles for the class imbalance problem: bagging-, boosting-, and hybrid-based approaches. IEEE Transactions on Systems, Man, and Cybernetics, Part C (Applications and Reviews). 2011;42(4):463–84.
Cooper GF, Herskovits E. A Bayesian method for the induction of probabilistic networks from data. Mach Learn. 1992;9(4):309–47.
Breiman L. Random forests. Mach Learn. 2001;45(1):5–32.
Rodriguez JD, Perez A, Lozano JA. Sensitivity analysis of k-fold cross validation in prediction error estimation. IEEE Trans Pattern Anal Mach Intell. 2009;32(3):569–75.
Ian H. Witten EF, Mark A Hall. Christopher J. Pal Weka 3: machine learning software in Java. 2017. In: Data mining: practical machine learning tools and techniques [Internet]. Cambridge, MA 02139: Morgan Kaufmann. fourth. [654]. Available from: https://www.cs.waikato.ac.nz/ml/weka/.
Baynes JW. Aging of complex systems. Medical Biochemistry E-Book. 2018:416.
Zughaier SM, Alvarez JA, Sloan JH, Konrad RJ, Tangpricha V. The role of vitamin D in regulating the iron-hepcidin-ferroportin axis in monocytes. J Clin Transl Endocrinol. 2014;1(1):e19–25.
Zofkova I, Davis M, Blahos J. Trace elements have beneficial, as well as detrimental effects on bone homeostasis. Physiol Res. 2017;66(3):391.
Toxqui L, Vaquero MP. Chronic iron deficiency as an emerging risk factor for osteoporosis: a hypothesis. Nutrients. 2015;7(4):2324–44.
Gaffney-Stomberg E. The impact of trace minerals on bone metabolism. Biol Trace Elem Res. 2019;188(1):26–34.
Balogh E, Paragh G, Jeney V. Influence of iron on bone homeostasis. Pharmaceuticals. 2018;11(4):107.
Tian T, Shao J, Shen Z, et al. Association of serum vitamin C with all-cause and cause-specific death: data from National Health and Nutrition Examination Survey (NHANES 2003-2006). Nutrition. 2022;101:111696.
Carr AC, Pullar JM, Bozonet SM, Vissers MC. Marginal ascorbate status (Hypovitaminosis C) results in an attenuated response to vitamin C supplementation. Nutrients. 2016;8(6):341.
Berger MM, Shenkin A, Schweinlin A, et al. ESPEN micronutrient guideline. Clin Nutr. 2022;41(6):1357–424.
Vitamin C, Committee SotAFF. Medical Research Council. Vitamin C requirement of human adults. Lmcet; 1948.
Acknowledgements
We thank Evan M. Parrott for his graphic arts expertise, which greatly assisted the presentation at IFSO 2022 and this publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
IRB # 834987.
Consent to Participate
For this type of study, formal consent is not required.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• VCD is harmful to numerous physiological pathways and disrupts human health.
• Vitamin B1, D, calcium, potassium, and iron deficiencies are associated with VCD.
• ML models predict a higher prevalence of VCD than previously considered in patients with MBS.
• Deficient lab indices may distinguish patients with MBS at risk for VCD.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Parrott, J.M., Parrott, A.J., Rouhi, A.D. et al. What We Are Missing: Using Machine Learning Models to Predict Vitamin C Deficiency in Patients with Metabolic and Bariatric Surgery. OBES SURG 33, 1710–1719 (2023). https://doi.org/10.1007/s11695-023-06571-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-023-06571-w