Abstract
Background
Phase angle (PhA), proposed as an indicator of the number, integrity, and function of cells and evaluated in some clinical situations, decreases after bariatric surgery (BS). In contrast, higher values are found in physically active or exercising individuals. We therefore evaluated the influence of physical activity on PhA after BS.
Methods
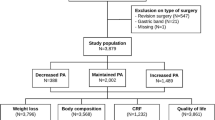
The PhA and body composition (obtained by bioelectrical impedance analysis), physical activity level (obtained by International Physical Activity Questionnaire), and metabolic equivalents (METs) were evaluated in adult women submitted to BS. The PhA and body composition were evaluated at three time points: before and 6 and 12 months after surgery. Physical activity level and METs were measured at the two postoperative time points.
Results
A reduction in PhA was observed 6 (p < 0.01) and 12 months (p < 0.01) after BS, with no significant difference between time points. A moderate or high physical activity level was found in 81% of the volunteers after 6 months and in 65% after 12 months. METs were reduced after 12 months compared to 6 months. A positive correlation (p < 0.05) was observed between PhA and body cell mass after surgery. There was a significant positive correlation (p < 0.01) between PhA and METs after 12 months.
Conclusions
Physical activity may attenuate the PhA reduction that occurs after BS, with this parameter reflecting the engagement of these patients in this type of activity.
Graphical abstract



Similar content being viewed by others
References
Lukaski HC. Evolution of bioimpedance: a circuitous journey from estimation of physiological function to assessment of body composition and a return to clinical research. Eur J Clin Nutr. 2013;67(1):S2–9. https://doi.org/10.1038/ejcn.2012.149.
Bosy-Westphal A, Danielzik S, Dörhöfer RP, et al. Phase angle from bioelectrical impedance analysis: population reference values by age, sex, and body mass index. JPEN J Parenter Enteral Nutr. 2006;30(4):309–16.
Streb AR, Hansen F, Gabiatti MP, et al. Phase angle associated with different indicators of health-related physical fitness in adults with obesity. Physiol Behav. 2020;15(225): 113104. https://doi.org/10.1016/j.physbeh.2020.113104.
Nicoletti CF, Camelo JS Jr, dos Santos JE, et al. Bioelectrical impedance vector analysis in obese women before and after bariatric surgery: changes in body composition. Nutrition. 2014;30(5):569–74. https://doi.org/10.1016/j.nut.2013.10.013.
Vassilev G, Hasenberg T, Krammer J, et al. The phase angle of the bioelectrical impedance analysis as predictor of post-bariatric weight loss outcome. Obes Surg. 2017;27(3):665–9. https://doi.org/10.1007/s11695-016-2315-9.
Koehler KB, Moraes RAG, Rodrigues JB, et al. Bioimpedance phase angle is associated with serum transthyretin but not with prognostic inflammatory and nutritional index during follow-up of women submitted to bariatric surgery. Clin Nutr ESPEN. 2019;33(10):183–7. https://doi.org/10.1016/j.clnesp.2019.05.018.
Di Vincenzo O, Marra M, Sacco AM, et al. Bioelectrical impedance (BIA)-derived phase angle in adults with obesity: a systematic review. Clin Nutr. 2021;40(9):5238–48. https://doi.org/10.1016/j.clnu.2021.07.035.
Bellafronte NT, Serafini RKK, Chiarello PG. Relationship between total physical activity and physical activity domains with body composition and energy expenditure among Brazilian adults. Am J Hum Biol. 2019;31(6): e23317. https://doi.org/10.1002/ajhb.23317.
Ribeiro AS, Avelar A, Dos Santos L, et al. Hypertrophy-type resistance training improves phase angle in young adult men and women. Int J Sports Med. 2017;38(1):35–40. https://doi.org/10.1055/s-0042-102788.
Langer RD, Silva AM, Borges JH, et al. Physical training over 6 months is associated with improved changes in phase angle, body composition, and blood glucose in healthy young males. Am J Hum Biol. 2019;31(5): e23275. https://doi.org/10.1002/ajhb.23275.
Mundstock E, Amaral MA, Baptista RR, et al. Association between phase angle from bioelectrical impedance analysis and level of physical activity: systematic review and meta-analysis. Clin Nutr. 2019;38(4):1504–10. https://doi.org/10.1016/j.clnu.2018.08.031.
Jungblut SA, Frickmann H, Zimmermann B, et al. Die Auswirkungen von Sport auf die Körperzusammensetzung von COPD-Patienten [The effects of physical training on the body composition of patients with COPD]. Pneumologie. 2009;63(7):374–9. https://doi.org/10.1055/s-0029-1214713.
Cupisti A, Capitanini A, Betti G, et al. Assessment of habitual physical activity and energy expenditure in dialysis patients and relationships to nutritional parameters. Clin Nephrol. 2011;75(3):218–25. https://doi.org/10.5414/cnp75218.
Wilms B, Frick J, Ernst B, et al. Whole body vibration added to endurance training in obese women - a pilot study. Int J Sports Med. 2012;33(9):740–3. https://doi.org/10.1055/s-0032-1306284.
Kyle UG, Bosaeus I, De Lorenzo AD, et al. ; ESPEN. Bioelectrical impedance analysis-part II: utilization in clinical practice. Clin Nutr. 2004;23(6):1430–53. https://doi.org/10.1016/j.clnu.2004.09.012.
Lohman TG, Roche AF. Anthropometric standardization reference manual. Champaing, IL: Human Kinetics Books; 1988.
Jensen MD, Ryan DH, Apovian CM, et al. Guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation. 2014;129(25):S102–38. https://doi.org/10.1161/01.cir.0000437739.71477.ee.
Maïmoun L, Lefebvre P, Jaussent A, et al. Body composition changes in the first month after sleeve gastrectomy based on gender and anatomic site. Surg Obes Relat Dis. 2017;13(5):780–7. https://doi.org/10.1016/j.soard.2017.01.017.
Sherf Dagan S, Tovim TB, Keidar A, et al. Inadequate protein intake after laparoscopic sleeve gastrectomy surgery is associated with a greater fat free mass loss. Surg Obes Relat Dis. 2017;13(1):101–9. https://doi.org/10.1016/j.soard.2016.05.026.
Craig CL, Marshall AL, Sjöström M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–95. https://doi.org/10.1249/01.MSS.0000078924.61453.FB.
Matsudo S, Araujo T, Matsudo V, et al. Questionário internacional de atividade física (IPAQ): estudo de validade e reprodutibilidade no brasil. Rev. Bras. Atividade física e saúde. 2001;6(2):5–18. https://doi.org/10.12820/rbafs.v.6n2p5-18.
Pinto SL, Juvanhol LL, Bressan J. Weight loss after RYGB is associated with an increase in serum vitamin D in a population with low prevalence of hypovitaminosis D at low latitude. Obes Surg. 2020;30(11):4187–91. https://doi.org/10.1007/s11695-020-04780-1.
Shi X, Karmali S, Sharma AM, et al. A review of laparoscopic sleeve gastrectomy for morbid obesity. Obes Surg. 2010;20(8):1171–7. https://doi.org/10.1007/s11695-010-0145-8.
Magro DO, Geloneze B, Delfini R, et al. Long-term weight regain after gastric bypass: a 5-year prospective study. Obes Surg. 2008;18(6):648–51. https://doi.org/10.1007/s11695-007-9265-1.
Turchi MJ, Kingma F, Laborda N, et al. Roux-en-Y gastric bypass in the elderly: is age a determining factor in our outcomes? Surg Obes Relat Dis. 2020;16(10):1514–20. https://doi.org/10.1016/j.soard.2020.05.015.
Wolfe BM, Kvach E, Eckel RH. Treatment of obesity: weight loss and bariatric surgery. Circ Res. 2016;118(11):1844–55. https://doi.org/10.1161/CIRCRESAHA.116.307591.
Vaurs C, Diméglio C, Charras L, et al. Determinants of changes in muscle mass after bariatric surgery. Diabetes Metab. 2015;41(5):416–21. https://doi.org/10.1016/j.diabet.2015.04.003.
Correa-Rodríguez M, Rueda-Medina B, González-Jiménez E, et al. Associations between body composition, nutrition, and physical activity in young adults. Am J Hum Biol. 2017;29(1). https://doi.org/10.1002/ajhb.22903.
Otto M, Färber J, Haneder S, et al. Postoperative changes in body composition–comparison of bioelectrical impedance analysis and magnetic resonance imaging in bariatric patients. Obes Surg. 2015;25(2):302–9. https://doi.org/10.1007/s11695-014-1382-z.
Golzarand M, Toolabi K, Djafarian K. Changes in body composition, dietary intake, and substrate oxidation in patients underwent laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy: a comparative prospective study. Obes Surg. 2019;29(2):406–43. https://doi.org/10.1007/s11695-018-3528-x.
Gonzalez MC, Barbosa-Silva TG, Bielemann RM, et al. Phase angle and its determinants in healthy subjects: influence of body composition. Am J Clin Nutr. 2016;103(3):712–6. https://doi.org/10.3945/ajcn.115.116772.
Ko SJ, Cho J, Choi SM, et al. Phase angle and frailty are important prognostic factors in critically ill medical patients: a prospective cohort study. J Nutr Health Aging. 2021;25(2):218–23. https://doi.org/10.1007/s12603-020-1487-0.
do Amaral Paes TC, de Oliveira KCC, de Carvalho Padilha P, et al. Phase angle assessment in critically ill cancer patients: Relationship with the nutritional status, prognostic factors and death. J Crit Care. 2018;44(4):430–35. https://doi.org/10.1016/j.jcrc.2018.01.006.
Sardinha LB. Physiology of exercise and phase angle: another look at BIA. Eur J Clin Nutr. 2018;72(9):1323–7. https://doi.org/10.1038/s41430-018-0215-x.
Friedrich AE, Damms-Machado A, Meile T, et al. Laparoscopic sleeve gastrectomy compared to a multidisciplinary weight loss program for obesity–effects on body composition and protein status. Obes Surg. 2013;23(12):1957–65. https://doi.org/10.1007/s11695-013-1036-6.
Rinaldi S, Gilliland J, O’Connor C, et al. Is phase angle an appropriate indicator of malnutrition in different disease states? Syst Rev Clin Nutr ESPEN. 2019;29:1–14. https://doi.org/10.1016/j.clnesp.2018.10.010.
Funding
We thank the Foundation for the Support of Research and Innovation of Espirito Santo (FAPES) scholarship granted to R.M. This work was supported by the FAPES (grant #85198560) and the Coordination for the Improvement of Higher Education Personnel (CAPES).
Author information
Authors and Affiliations
Contributions
RM, FAV, GPSM, FKH and RGP participated in the conception and design of the study. RM and FAV participated in the collection of data. RM, FAV, GPSM, FKH and RGP participated in the analysis and interpretations of data. RM and RGP wrote the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
The study was approved by the local ethics committees (#51519115.7.0000.5071) and performed in accord with the ethical standards of the Declaration of Helsinki.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Phase angle is a novel marker for outcomes following bariatric surgery.
• Physical activity can attenuate the phase angle reduction after bariatric surgery.
• The phase angle can suggest the level of physical activity and vice versa.
• Future studies could consider physical activity in determining the phase angle.
Rights and permissions
About this article
Cite this article
Manoel, R., Venâncio, F.A., Miguel, G.P.S. et al. A Higher Phase Angle Is Associated with Greater Metabolic Equivalents in Women 1 Year After Bariatric Surgery. OBES SURG 32, 2003–2009 (2022). https://doi.org/10.1007/s11695-022-06050-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-022-06050-8