Abstract
Purpose
Obesity has been reported to be associated with short sleep duration. It follows that patients with a BMI >35kg/m2 could be expected to have the poorest sleep. This poor sleep could be explained by the presence of obstructive sleep apnoea (OSA), although treatment with positive airway pressure (PAP) may modify this. The purpose of this study is to determine if patients attending for bariatric surgery have poor sleep independent of OSA status.
Materials and Methods
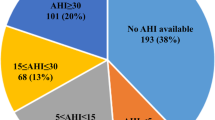
Sleep duration and quality, using the Pittsburgh Sleep Quality Index (PSQI), was analysed in 203 patients undergoing bariatric surgery between June 2016 and May 2019 in a single centre. Anthropometric data on all patients were recorded as well as presence of OSA and PAP usage.
Results
The bariatric population reported an average (standard deviation) sleep duration of 6.5 (1.6) h, and 67.9% of patients had a documented poor sleep quality (PSQI>5). The presence of OSA did not significantly influence either sleep duration (p=0.23) or sleep quality (p=0.5). On logistic regression, there was no significant relationship between sleep duration or sleep quality and the following variables: age, sex, and AHI. There was however a significant association between BMI and sleep quality (p= 0.007). PSQI was inversely associated with BMI. This equated to 1 kg/m2 weight gain being associated with 0.097 decrease in PSQI score.
Conclusions
The presence of OSA does not influence either sleep duration or sleep quality in the bariatric surgical population. This suggests that clinically severe obesity itself may cause poor sleep.
Graphical abstract






Similar content being viewed by others
References
Gangwisch JE, Malaspina D, Boden-Albala B, et al. Inadequate sleep as a risk factor for obesity: analysis of NHANES I. Sleep. 2005;28:1289–96.
Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity. 2008;16:643–53.
Hasler G, Buysse DJ, Klaghofer R, Gamma A, Ajdacic V, Eich D, Rössler W, Angst J. The association between short sleep duration and obesity in young adults: a 13-year prospective study. Sleep. 2004;27(4):661–6. https://doi.org/10.1093/sleep/27.4.661.
Cappuccio FP, Taggart FM, Kandala NB, et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31(5):619–626. https://doi.org/10.1093/sleep/31.5.619.
Häusler N, Heinzer R, Haba-Rubio J, Marques-Vidal P. Does sleep affect weight gain? Assessing subjective sleep and polysomnography measures in a population-based cohort study (CoLaus/HypnoLaus). Sleep. 2019;42(6):zsz077. https://doi.org/10.1093/sleep/zsz077.
Gov.ie. 2020. Healthy Ireland Survey Documents. [online] Available at: https://www.gov.ie/en/collection/231c02-healthy-ireland-survey-wave/. Accessed 4 Nov 2020.
Stegenga H, Haines A, Jones K, et al. Identification, assessment, and management of overweight and obesity: summary of updated NICE guidance. BMJ. 2014;349(nov27 2):g6608.
Toor P, Kim K, Buffington C. Sleep quality and duration before and after bariatric surgery. Obes Surg. 2011;22(6):890–5.
Obstructive sleep apnoea and perioperative complications in bariatric patients. Survey of Anesthesiology. 2011;55(5):240. https://doi.org/10.1097/SA.0b013e3182291ca9.
O'Reilly E, Doherty L, O'Boyle C. How relevant is pre-operative obstructive sleep apnoea in the asymptomatic bariatric surgery patient? Obes Surg. 2020;30(3):969–74.
Nagappa M, Liao P, Wong J, Auckley D, Ramachandran SK, Memtsoudis S, Mokhlesi B, Chung F. Validation of the STOP-bang questionnaire as a screening tool for obstructive sleep apnea among different populations: a systematic review and meta-analysis. PLoS One. 2015;10(12):e0143697. https://doi.org/10.1371/journal.pone.0143697.
Reed K, Pengo MF, Steier J. Screening for sleep-disordered breathing in a bariatric population. J Thorac Dis. 2016;8(2):268–75.
Chung F, Subramanyam R, Liao P, et al. High STOP-Bang score indicates a high probability of obstructive sleep apnoea. Br J Anaesth. 2012;108(5):768–75.
Buysse D, Reynolds C, Monk T, et al. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213.
Xie H, Doherty L, O'Boyle C. The positive impact of bariatric surgery on sleep. Ir Med J. 2016;109(1):328–30.
Beck S, Schwartz A, Towsley G, et al. Psychometric evaluation of the Pittsburgh sleep quality index in cancer patients. J Pain Symptom Manag. 2004;27(2):140–8.
Hinz A, Glaesmer H, Brähler E, et al. Sleep quality in the general population: psychometric properties of the Pittsburgh Sleep Quality Index, derived from a German community sample of 9284 people. Sleep Med. 2017;30:57–63.
Pinto T, de Bruin P, de Bruin V, et al. Obesity, Hypersomnolence, and Quality of Sleep: the Impact of Bariatric Surgery. Obes Surg. 2017;27(7):1775–9.
Araghi M, Jagielski A, Neira I, et al. The complex associations among sleep quality, anxiety-depression, and quality of life in patients with extreme obesity. Sleep. 2013;36(12):1859–65.
Chaput JP, Després JP, Bouchard C, Tremblay A. Short sleep duration is associated with reduced leptin levels and increased adiposity: Results from the Quebec family study. Obesity (Silver Spring). 2007;15(1):253–61. https://doi.org/10.1038/oby.2007.512.
Taheri S, Lin L, Austin D, et al. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;1:210–21.
Kushida CA (Ed). Sleep deprivation: basic science, physiology and behavior, 1st ed. CRC Press. 2004:294–310. https://doi.org/10.1201/b14428.
Capers PL, Fobian AD, Kaiser KA, et al. A systematic review and meta-analysis of randomized controlled trials of the impact of sleep duration on adiposity and components of energy balance. Obes Rev. 2015;16(9):771–82.
Stern JH, Grant AS, Thomson CA, et al. Short sleep duration is associated with decreased serum leptin, increased energy intake and decreased diet quality in postmenopausal women. Obesity (Silver Spring). 2014;22(5):E55–61.
Li L, Sheehan CM, Thompson MS. Measurement invariance and sleep quality differences between men and women in the Pittsburgh Sleep Quality Index. J Clin Sleep Med. 2019;15(12):1769–76.
O'Brien E, Hart C, Wing RR. Discrepancies between self-reported usual sleep duration and objective measures of total sleep time in treatment-seeking overweight and obese individuals. Behav Sleep Med. 2016;14(5):539–49.
Matthews KA, Patel SR, Pantesco EJ, Buysse DJ, Kamarck TW, Lee L, Hall MH. Similarities and differences in estimates of sleep duration by polysomnography, actigraphy, diary, and self-reported habitual sleep in a community sample. Sleep Health. 2018;4(1):96–103. https://doi.org/10.1016/j.sleh.2017.10.011.
Van Den Berg JF, Van Rooij FJ, Vos H, Tulen JH, Hofman A, Miedema HM, Neven AK, Tiemeier H. Disagreement between subjective and actigraphic measures of sleep duration in a population-based study of elderly persons. J Sleep Res. 2008;17(3):295–302. https://doi.org/10.1111/j.1365-2869.2008.00638.x.
Lauderdale D, Knutson K, Yan L, et al. Self-reported and measured sleep duration. Epidemiology. 2008;19(6):838–45.
Carneiro G, Flório RT, Zanella MT, et al. Is mandatory screening for obstructive sleep apnea with polysomnography in all severely obese patients indicated? Sleep Breath. 2012;16(1):163–8.
Flemons WW, Littner MR, Rowley JA, et al. Home diagnosis of sleep apnea: a systematic review of the literature. An evidence review cosponsored by the American Academy of Sleep Medicine, the American College of Chest Physicians, and the American Thoracic Society. Chest. 2003;124:1543–79.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
This study submission was designed with aid from the STROBE guidelines.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
1.Patients being assessed for bariatric surgery have a short sleep duration and poor sleep quality, but this is not a linear relationship.
2.Sleep duration and quality are independent of the presence or severity of obstructive sleep apnoea.
3.Positive airway pressure therapy did not influence this poor sleep.
Colm O’Boyle and Liam Doherty are co-authors.
Rights and permissions
About this article
Cite this article
O’Halloran, D., O’Boyle, C. & Doherty, L. Poor Sleep Associated with Clinically Severe Obesity Is Independent of OSA Status. OBES SURG 31, 4734–4740 (2021). https://doi.org/10.1007/s11695-021-05588-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-021-05588-3