Abstract
Background and Aims
Bariatric surgery provides a useful opportunity to perform intraoperative liver biopsy to screen for non-alcoholic steatohepatitis (NASH). There is currently no consensus on whether intraoperative liver biopsy should be systematically performed. The aim of this study was to develop and validate a decision tree to guide that choice.
Approach and Results
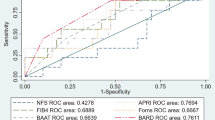
This prospective study included 102 consecutive patients from the severe obesity outcome network (SOON) cohort in whom liver biopsy was systematically performed during bariatric surgery. A classification and regression tree (CART) was created to identify the nodes that best classified patients with and without NASH. External validation was performed. Seventy-one biopsies were of sufficient quality for analysis (median body mass index 43.3 [40.7; 48.0] kg/m2). NASH was diagnosed in 32.4% of cases. None of the patients with no steatosis on ultrasound had NASH. The only CART node that differentiated between a “high-risk” and a “low-risk” of NASH was alanine aminotransferase (ALT). ALT>53IU/L predicted NASH with a positive predictive value (PPV) of 68% and a negative predictive value (NPP) of 89%, a sensitivity of 77%, and a specificity of 84%. In the external cohort (n=258), PPV was 68%, NPV was 62%, sensitivity was 27%, and specificity was 90%.
Conclusions
The present work supports intraoperative liver biopsy to screen for NASH in patients with ALT>53IU/L; however, patients with no steatosis on ultrasound should not undergo biopsy. The CART failed to identify an algorithm with a good sensitivity to screen for NASH in patients with ultrasonography-proven steatosis and ALT≤53IU/L.


Similar content being viewed by others
References
Goh GB, McCullough AJ. Natural history of nonalcoholic fatty liver disease. Dig Dis Sci. 2016;61:1226–33.
Dulai PS, Singh S, Patel J, et al. Increased risk of mortality by fibrosis stage in nonalcoholic fatty liver disease: systematic review and meta-analysis. Hepatology. 2017;65:1557–65.
Shah AG, Lydecker A, Murray K, et al. Comparison of noninvasive markers of fibrosis in patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2009;7:1104–12.
Castera L, Friedrich-Rust M, Loomba R. Noninvasive assessment of liver disease in patients with nonalcoholic fatty liver disease. Gastroenterology. 2019;156:1264–81. e4
European Association for the Study of the L, European Association for the Study of D, European Association for the Study of O. EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J Hepatol. 2016;64:1388–402.
Mahawar KK, Parmar C, Graham Y, et al. Routine liver biopsy during bariatric surgery: an analysis of evidence base. Obes Surg. 2016;26:177–81.
Barbois S, Arvieux C, Leroy V, et al. Benefit-risk of intraoperative liver biopsy during bariatric surgery: review and perspectives. Surg Obes Relat Dis. 2017;13:1780–6.
Ooi GJ, Burton PR, Earnest A, et al. Visual liver score to stratify non-alcoholic steatohepatitis risk and determine selective intraoperative liver biopsy in obesity. Obes Surg. 2018;28:427–36.
Spengler EK, Loomba R. Recommendations for diagnosis, referral for liver biopsy, and treatment of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. Mayo Clin Proc. 2015;90:1233–46.
Fried M, Yumuk V, Oppert JM, et al. Interdisciplinary European Guidelines on metabolic and bariatric surgery. Obes Facts. 2013;6:449–68.
Bedossa P, Tordjman J, Aron-Wisnewsky J, et al. Systematic review of bariatric surgery liver biopsies clarifies the natural history of liver disease in patients with severe obesity. Gut. 2017;66:1688–96.
Debedat J, Sokolovska N, Coupaye M, et al. Long-term relapse of type 2 diabetes after Roux-en-Y gastric bypass: prediction and clinical relevance. Diabetes Care. 2018;41:2086–95.
Bedossa P, Poitou C, Veyrie N, et al. Histopathological algorithm and scoring system for evaluation of liver lesions in morbidly obese patients. Hepatology. 2012;56:1751–9.
Brunt EM, Kleiner DE, Wilson LA, et al. Nonalcoholic fatty liver disease (NAFLD) activity score and the histopathologic diagnosis in NAFLD: distinct clinicopathologic meanings. Hepatology. 2011;53:810–20.
Eddowes PJ, Sasso M, Allison M, et al. Accuracy of FibroScan controlled attenuation parameter and liver stiffness measurement in assessing steatosis and fibrosis in patients with nonalcoholic fatty liver disease. Gastroenterology. 2019;156:1717–30.
Polyzos SA, Kountouras J, Mantzoros CS. Obesity and nonalcoholic fatty liver disease: from pathophysiology to therapeutics. Metabolism. 2019;92:82–97.
Lassailly G, Caiazzo R, Buob D, et al. Bariatric surgery reduces features of nonalcoholic steatohepatitis in morbidly obese patients. Gastroenterology. 2015;149:379–88. quiz e15-6
Caiazzo R, Lassailly G, Leteurtre E, et al. Roux-en-Y gastric bypass versus adjustable gastric banding to reduce nonalcoholic fatty liver disease: a 5-year controlled longitudinal study. Ann Surg. 2014;260:893–8. discussion 898-9
Xiao G, Zhu S, Xiao X, et al. Comparison of laboratory tests, ultrasound, or magnetic resonance elastography to detect fibrosis in patients with nonalcoholic fatty liver disease: a meta-analysis. Hepatology. 2017;66:1486–501.
Tapper EB, Challies T, Nasser I, et al. The performance of vibration controlled transient elastography in a US cohort of patients with nonalcoholic fatty liver disease. Am J Gastroenterol. 2016;111:677–84.
Petta S, Wong VW, Camma C, et al. Serial combination of non-invasive tools improves the diagnostic accuracy of severe liver fibrosis in patients with NAFLD. Aliment Pharmacol Ther. 2017;46:617–27.
Praveenraj P, Gomes RM, Kumar S, et al. Prevalence and predictors of non-alcoholic fatty liver disease in morbidly obese south Indian patients undergoing bariatric surgery. Obes Surg. 2015;25:2078–87.
Teixeira AR, Bellodi-Privato M, Carvalheira JB, et al. The incapacity of the surgeon to identify NASH in bariatric surgery makes biopsy mandatory. Obes Surg. 2009;19:1678–84.
Dolce CJ, Russo M, Keller JE, et al. Does liver appearance predict histopathologic findings: prospective analysis of routine liver biopsies during bariatric surgery. Surg Obes Relat Dis. 2009;5:323–8.
Petrick A, Benotti P, Wood GC, et al. Utility of ultrasound, transaminases, and visual inspection to assess nonalcoholic fatty liver disease in bariatric surgery patients. Obes Surg. 2015;25:2368–75.
Dallal RM, Samuel G, Lord JL, et al. Hemobilia: a rare complication after routine liver biopsy during gastric bypass. Surg Obes Relat Dis. 2007;3:91–3.
Padoin AV, Mottin CC, Moretto M, et al. A comparison of wedge and needle hepatic biopsy in open bariatric surgery. Obes Surg. 2006;16:178–82.
Acknowledgements
We wish to thank Stephane Ruckly (ICUREsearch®, Paris, France), professional statistician who performed statistical analyses, and M’Barka Daoukhi, clinical research assistant for the SOON cohort. The authors also thank Valentine Lemoine (Institute of Cardiometabolism and Nutrition) for patient follow-up, Dr. Florence Marchelli (Centre de Recherche en Nutrition Humaine, Ile-de-France, France) for data management, and Rohia Alili (Centre de Recherche en Nutrition Humaine, Ile-de-France, France) for her contribution to biobanking.
Funding
The SOON cohort is supported by the foundation “Agir pour les maladies chronique,” the “Agence Régionale pour la Santé Auvergne-Rhône-Alpes,” France, and the “Direction de la recherche clinique et de l’innovation” of the “Centre Hospitalier Universitaire Grenoble Alpes,” France. BARICAN clinical study was supported by the Assistance Publique Hôpitaux de Paris and the Centre de Recherche Clinique (CRC) for clinical investigation (CRC P050318 to C.P., PHRC 02076 to K.C., and CRC-FIBROTA to K.C. and J.A.-W. and RC BDD 2017 to JAW). L’Agence Nationale de la Recherche supported the clinical study (ANR Adipofib, and the national program “Investissements d’Avenir” with the reference ANR-10-IAHU-05).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
S. Barbois has no conflict of interest to declare for the present study.
N. Stürm has no conflict of interest to declare for the present study.
J. Aron-Wisnewsky has no conflict of interest to declare for the present study.
K. Clément has no conflict of interest to declare for the present study.
P. Bedossa has no conflict of interest to declare for the present study.
L. Genser has no conflict of interest to declare for the present study
M. N. Hilleret has no conflict of interest to declare for the present study.
C. Costentin received fees for expert work by InterceptTM.
F. Reche has no conflict of interest to declare for the present study.
C. Arvieux has no conflict of interest to declare for the present study.
AL. Borel has no conflict of interest to declare for the present study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Barbois, S., Stürm, N., Aron-Wisnewsky, J. et al. Decision Tree for the Performance of Intraoperative Liver Biopsy During Bariatric Surgery. OBES SURG 31, 2641–2648 (2021). https://doi.org/10.1007/s11695-021-05309-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-021-05309-w