Abstract
Background
Morbid obesity, compromising cardiovascular and respiratory function, may increase the risk of anesthesia and was initially considered a contraindication to laparoscopy. The aim of this study was to investigate hemodynamic effects induced by pneumoperitoneum in superobese patients, assessed by arterial pulse contour method.
Methods
We prospectively studied 10 obese patients (BMI 53 ± 9 kg/m2), scheduled for laparoscopic gastric bypass. After anesthesia induction, patients were intubated and mechanically ventilated. A radial artery was cannulated to obtain hemodynamic data implemented by means of a new pulse contour analysis method—the pressure recording analytical method (PRAM). Data were recorded after anesthesia induction (Tbas), at peritoneal insufflation (T0), at 1, 3, 5, 10, 30, and 60 min after pneumoperitoneum induction (T1, T3, T5, T10, T15, T30, T60), at abdominal desufflation (Tdef) and 5 min after desufflation (T5def).
Results
MAP increased after pneumoperitoneum, returning to its baseline after deflation (79 ± 7 Tbas, 81 ± 6 mmHg T5def). HR remained unchanged. Systemic vascular resistance index (SVRI) increased after pneumoperitoneum induction and progressively returned to baseline (3,903 ± 330 Tbas, 4,596 ± 148 T1, and 3,786 ± 202 dyn s m2 cm−5 T5def). Stroke volume index (SVI) and cardiac index (CI) increased after pneumoperitoneum and remained elevated. Stroke volume variation (SVV) decreased after insufflation remaining lower than the basal value (28 ± 4% Tbas, 15 ± 5% T5des). Cardiac Cycle Efficiency (CCE) transient decreased after insufflation and subsequently increased (0.029 ± 0.146 Tbas, 0.008 ± 0.178 T5def). Aortic dP/dt max increased after insufflation, returning to baseline only after desufflation (0.68 ± 0.07 Tbas, 0.94 ± 0.08 T30 and 0.86 ± 0.06 mmHg s−1 T5def).
Conclusion
As assessed by PRAM, this study showed no deterioration in hemodynamic indices or ventricular performance during laparoscopic gastric bypass.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Morbid obesity, increasing the risk of anesthesia and surgery, was initially considered a relative contraindication to laparoscopy. Studies of laparoscopic cholecystectomy in morbidly obese patients have shown similar surgical results to nonobese patients, and some authors propose laparoscopy as the technique of choice. Laparoscopy offers many advantages in comparison to open surgery, such as minimal tissue trauma, less postoperative pain, reduced postoperative complications, early mobilization, and rehabilitation [1, 2].
However, pneumoperitoneum, which is associated with increased abdominal pressure and CO2 absorption, and Trendelenburg position, which is required for certain types of surgery, may cause deterioration of the cardiovascular and respiratory functions in morbidly obese individuals. The increased blood pressure associated with pneumoperitoneum induces increased afterload, causing impairment of left ventricular function and reduction of cardiac output [3, 4].
Previous hemodynamic studies in the morbidly obese, performed during laparoscopic surgery, show that the laparoscopic technique can be performed safely [5, 6]. However, these high-risk patients may benefit from invasive hemodynamic monitoring [7–10].
The aim of this study was to investigate hemodynamic changes during laparoscopic gastric bypass in superobese patients, using an arterial pulse contour analysis based on the pressure recording analytical method (PRAM).
Materials and Methods
After obtaining informed consent, 10 obese patients scheduled for laparoscopic gastric bypass over a 5-month period, between March 2006 and July 2006, were prospectively studied.
Patients who had previous gastric and bladder surgery, a large abdominal ventral hernia, or a history of severe cardiovascular disease were excluded from the investigation.
Each patient underwent a preoperative evaluation, including echocardiographic assessment, blood gases analysis, and pulmonary function tests.
Body mass was evaluated using the body mass index (BMI): weight (kg)/height (m2). Body surface area (BSA) was calculated using the Mosteller formula:
General anesthesia was induced with i.v. propofol (2 mg kg−1), fentanyl (2 mcg kg−1), and cisatracurium besilate (0.1 mg kg−1) and maintained with sevofluorane (end-tidal concentration: 1.5–2%). Repeated doses of fentanyl (1 mcg kg−1) were administered during surgery as necessary, based on clinical signs (heart rate, blood pressure, pupil size, and diaphoresis).
After orotracheal intubation, the patients’ lungs were ventilated with oxygen and air, in a pressure-controlled ventilation mode (Datex-Ohmeda ventilator device) to maintain end-tidal CO2 between 35 and 45 mmHg, airway pressure under 35 cmH2O and pulse oximetry saturation (SpO2) > 95%.
All patients received a basal i.v. infusion of lactate Ringer’s solution (7 ml kg−1 h−1). In addition to standard monitoring (three-lead ECG, pulse oximeter, urinary volume, noninvasive arterial blood pressure) after anesthesia induction, a radial artery catheter was placed for hemodynamic monitoring, using a variation of arterial pulse contour analysis (pressure recording analytical method, PRAM).
The patients were studied only during reverse Trendelenburg position (30° head-up), both before and after abdominal insufflation. Pneumoperitoneum was established by the introduction of a Verres’ needle. Mean intraabdominal pressure (IAP) was maintained between 14 and 17 mmHg during the entire surgical procedure.
Hemodynamic data were collected 10 times during general anesthesia: at 5 min after anesthesia induction (Tbas), at CO2 peritoneal insufflation (T0), at 1, 3, 5, 10, 30, 60 min after insufflation (T1, T3, T5, T10, T15, T30, and T60, respectively), at pneumoperitoneum deflation (Tdef) and 5 min after deflation (T5def).
Data are expressed as mean ± standard deviation.
Hemodynamic data were compared using Wilcoxon’s test. A p value less than 0.05 was considered significant. Statistical evaluations were carried out using software Statview 5.0 for Windows.
Hemodynamic Recordings and PRAM: Theoretical Background and Description
Mini-invasive hemodynamic monitoring was performed by MostCare™ device, based on “pressure recording analytical method” (PRAM). PRAM is based on the beat-by-beat analysis of the arterial waveform and does not require calibration or precalculated parameters [11–14]. The changes in volume that occur in all arterial vessels are caused by arterial wall expansion in response to blood pressure changes. This depends on various physical factors, such as the force of cardiac contraction and vascular factors, which are the arterial impedance, compliance, and peripheral resistance. With PRAM, the area under the pressure curve is measured during each cardiac cycle. Simultaneously, the impedance (Z) is obtained from morphologic analysis of both the pulsatile and the continuous components of the pressure waveform: Z = (P/t) k and stroke volume (SV) is calculated as SV = A/[(P/t) k], where A is the area under systolic portion of the pressure curve; P/t is a description of pressure wave profile expressed as the variation pressure (P) over time (t); k is a factor inversely related to the instantaneous acceleration of the vessel cross-sectional area [15]. Cardiac output is calculated as heart rate × SV [12].
Mean arterial pressure (MAP), heart rate (HR), systemic vascular resistance index (SVRI), stroke volume index (SVI), and cardiac index (CI) were measured continuously during the procedure. Additionally, PRAM provides us with new parameters: the cardiac cycle efficiency (CCE), aortic dP/dt max and stroke volume variation (SVV). SVV is the percent difference between the maximal and minimal stroke volume during a single respiratory cycle, divided by the mean stroke volume value. The rationale behind the SVV is that the alternating intrathoracic pressure, during each mechanical breath, induces transient changes in cardiac preload, which lead to variations in stroke volume, according to the Frank-Starling mechanism. It has been observed that wide variations in SVV occur when the left ventricle is operating on the steep slope of the Starling curve, whereas the shallow slope of the curve results in narrow undulations with small SVV. Specifically, large SVV resulting from hypovolemia indicates that stroke volume may be improved by fluid loading [16]. Several studies have shown that SVV correctly predicted fluid responsiveness in different groups of patients who underwent brain and cardiac surgery [17–19].
CCE represents the ratio between the hemodynamic work and the energy cost sustained by the heart. In terms of flow, aortic dP/dt max is the pressure analog of peak aortic blood acceleration (dQ/dt max) and depends on both left ventricular contractility and arterial impedance [20–22].
Results
Ten consecutive patients (four male and six female) were studied. The mean age was 38 ± 1 years, the mean weight was 150 ± 28 kg, and the mean BMI was 53 ± 9 kg/m2.
No patient had significant coexisting cardiopulmonary diseases, as shown by preoperative evaluation (Table 1).
Overall hemodynamic results with p values are reported in Table 2.
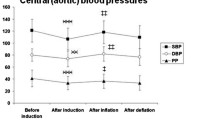
At insufflation, MAP increased significantly and remained elevated for the duration of the pneumoperitoneum (from 79 ± 7 mmHg at Tbas to 103 ± 7 mmHg at T10 and 97 ± 10 mmHg at T30). At desufflation, arterial pressure decreased immediately and returned to baseline values (81 ± 6 mmHg at 5 min after deflation), (Fig. 1).
Hemodynamic variations during laparoscopic surgery in obese patients. Data (means) are the same as those shown in Table 1. *Statistically significant versus baseline values (Tbas); °statistically significant versus insufflation times (T0)
Compared with baseline, HR remained essentially unchanged during the entire insufflation period (from 79 ± 9 bpm at Tbas to 75 ± 9 bpm at T10 and 79 ± 8 bpm at T30), (Fig. 1).
At induction of pneumoperitoneum, SVRI increased significantly, reaching a peak after the first minute (from 3,903 ± 330 dyn s cm−5 m−2 at Tbas to 4,596 ± 148 dyn s cm−5 m−2 at T1), then gradually decreased to a constant value, that was maintained even after desufflation (3,949 ± 146 dynes s cm−5 m−2 and 3,786 ± 202 dyn s cm−5 m−2 at T30 and 5 min after desufflation, respectively) (Fig. 1).
SVI increased significantly after pneumoperitoneum induction, remaining elevated throughout the surgical procedure (from 19.2 ± 3.8 ml m−2 at Tbas to 26.3 ± 1.8 ml m−2 and 25.6 ± 1.9 ml m−2 at T10 and T30, respectively) and after desufflation (T5def: 25.0 ± 1.4 ml m−2) (Fig. 1).
CI increased after insufflation reaching its maximum value at 10 min after pneumoperitoneum induction (from 1.63 ± 0.25 l min−1 m−2 at Tbas to 2.06 ± 0.20 l min−1 m−2 at T10), persisting at values higher than baseline throughout all the operative procedure (1.99 ± 0.26 l min−1 m−2 at T30 and 1.80 ± 0.10 l min−1 m−2 at 5 min after desufflation) and returning to starting point 5 min after desufflation, (Fig. 1).
SVV decreased considerably in the first 10 min (from 28 ± 4% at Tbas to 11 ± 3% at T10) and then it remained unchanged (12 ± 5% at T30 and 15 ± 5% at T5def), (Fig. 1). Induction of pneumoperitoneum caused a transient decrease in CCE that reached its minimum value the first minute after insufflation (from 0.029 ± 0.146 at Tbas to -0.553 ± .104 at T1). Subsequently, CCE increased, remaining constant until procedure termination (0.015 ± 0.133 at T30 and 0.008 ± 0.178 at T5def) (Fig. 1).
Aortic dP/dt max increased significantly after insufflation and remained elevated throughout the duration of pneumoperitoneum (from 0.68 ± 0.07 mmHg s−1 at Tbas to 0.94 ± 0.08 mmHg s−1 at T30). After desufflation, it decreased and returned to values similar to baseline (0.86 ± 0.06 mmHg s−1 at T5def) (Fig. 1).
Discussion
In this study, we report hemodynamic changes observed in the course of laparoscopic gastric bypass in a series of 10 obese patients. Previous investigations reported that peritoneal insufflation resulted in significant increase in cardiac afterload (MAP and SVR), both in obese and nonobese patients [6, 10, 23]. This effect is caused by compression of the splanchnic vessels by increased abdominal pressure and to neuro-humoral effect of CO2 adsorption, resulting in the release of vasoactive agents [24, 25]. In our obese population, we observed that MAP increased after abdominal insufflation, and remained elevated throughout the procedure, identically as it occurs in normal weight patients [1, 2, 6, 8–10].
Systemic vascular resistance index (SVRI) increased significantly after pneumoperitoneum induction, reaching a peak in the first minute and then returned gradually to baseline value, concordant with previous reports during laparoscopic obesity surgery [6, 10]. This finding demonstrates an important difference from investigations in nonobese patients [26, 27]. Haxby et al. and Girardis et al. reported that in normal weight subjects, peripheral vascular resistances remained higher than basal values throughout the duration of the pneumoperitoneum. This disparity between obese and nonobese patients is probably because of major differences in abdominal wall compliance. This promotes better adaptation to the IAP, thus minimizing the hemodynamic effects of the pneumoperitoneum [5].
In agreement with previous studies, no changes in HR were noted after the induction of pneumoperitoneum in both obese and nonobese patients [10, 23, 27–29].
Analyzing the CI and SVI trends, we observed that they increased significantly after abdominal insufflation, remaining elevated throughout the surgical procedure and after desufflation. These data are similar to those reported by Artuso and Fried in obese patients using pulmonary artery thermodilution [2, 10]. Nguyen and Dumont [5, 6], using the same method, observed that CI transiently decreased after pneumoperitoneum induction and progressively increased above baseline values.
In our opinion, the early increase in CI and SVI, without any modifications of HR, but with enhanced afterload, was probably because of the positive inotropic effect caused both by the sympathic stimulation induced by peritoneal insufflation and CO2 adsorption, and by the increase of cardiac preload, which improves stroke volume through Starling mechanism. Several investigations show that cardiac preload is depressed during pneumoperitoneum because increased IAP impedes central venous return [30–34]. However, the effects of IAP on venous return are more complex. Kashtan et al. studied the hemodynamic effects of IAP in relation to venous return and cardiac output in dogs [23]. They observed that venous return and cardiac output decreased in hypovolemic and normovolemic animals, but increased in hypervolemic dogs when IAP was increased. In the morbidly obese hypervolemic state, the great venous capacitance system is plethoric. Thus, during pneumoperitoneum, the vasoconstriction induced by sympathetic activation and the compression of the inferior vena cava augment venous return to the right atrium (preload), thereby augmenting cardiac output through the Starling mechanism.
In our study, cardiac filling pressures (CVP or PCWP) were not considered proper indicators of preload, as they may be influenced by elevated IAP. This augments pleural and intrathoracic pressure, resulting in cardiac compression with decrease in diastolic ventricular compliance [3, 5]. An impairment of diastolic compliance was also suggested by transesophageal echocardiography (TEE) in nonobese patients during laparoscopy [3, 35]. SVV, which reflects the beat-to-beat variability of stroke volume during the respiratory cycle, could be considered an efficient dynamic indicator of intravascular volume status and fluid responsiveness in mechanically ventilated patients [36]. The oscillating intrathoracic pressure during each mechanical breath induces transient changes in cardiac preload, which lead to variability in stroke volume, again according to the Frank-Starling mechanism. Benkerstadt et al. [17] demonstrated that, in healthy patients undergoing neurosurgery, a SVV value of 9.5% predicts a positive increase (5%) in cardiac output in response to fluid administration (100 ml of plasma expander) with 79% sensitivity and 93% specificity. According to Berkenstadt et al., recent studies confirm that SVV also predicts the fluid responsiveness in cardiac surgery [18, 19]. We postulate that in the normovolemic condition, the cardiac preload during the respiratory cycle is only briefly impaired by positive intrathoracic pressure during mechanical ventilation, thereby generating a SVV less than 15%. Because preload is severely impaired in hypovolemia, this variability during positive pressure ventilation is increased. After the induction of pneumoperitoneum, we observed that SVV decreased significantly from 28% to 11%, suggesting a reduction in fluid responsiveness. This result suggests that elevated IAP during pneumoperitoneum reduces venous capacitance through inferior vena cava compression, inducing a redistribution of intravascular fluid volume to the intrathoracic compartment. This enhances venous return to the right atrium with an increase in intrathoracic and global end-diastolic volume, which improves cardiac contractility and stroke volume by the Starling mechanism. The same effect was previously described by Alfonsi et al. using TEE; they found a progressive increase in superior vena cava (SVC) diameter, which suggested that blood might be forced into the thoracic cavity from the abdominal compartment during pneumoperitoneum [4].
Improvement of ventricular contractility might also be assessed by analyzing the trend of the maximal rate of rise in the arterial pressure pulse curve (dP/dt max). Aortic dP/dt max has been widely accepted as an index of the systolic performance of the left ventricle [37], and in our study we observed that dP/dt max increased immediately after peritoneal insufflation and remained elevated beyond desufflation. During the initial phase it could be explained by a chemically mediated positive inotropic effect, in addition to the associated increase of systemic vascular resistance index (SVRI), which raises the arterial impedance. In the ensuing phases, SVRI returned to baseline, whereas dP/dt max remained elevated. This supports the hypothesis that cardiac contractility is increased during pneumoperitoneum.
Beyond SV and CO determination, PRAM can be used for derivation of another useful parameter, the cardiac cycle efficiency index (CCE). CEE expresses cardiac performance in terms of energy expenditure of cardiovascular system [16–18]. In our patients, pneumoperitoneum caused a transient decrease in CCE, which reached a minimum value in the first minute after insufflation. This suggests that this decrease in CCE is caused by the marked increase of SVRI, which represents the afterload against which the left ventricle must pump.
Analyzing trends of CI, dP/dt max and CCE, we demonstrate that our patients had a satisfactory cardiac response to laparoscopic surgery and that prolonged pneumoperitoneum does not significantly depress cardiac function in our morbidly obese patients.
These data agree with results reported by Prior et al. [28], which corroborated the lack of deleterious cardiac effects of pneumoperitoneum on cardiac function in obese patients. Using intraoperative transesophageal echocardiography (TEE), they observed that ejection fraction (EF%), an index of left ventricular systolic function, was unaffected by pneumoperitoneum, confirming previous results [38].
These compensatory hemodynamic responses to the IAP were probably caused by the fact that patients included in our study had no demonstrable evidence or history of cardiovascular disease.
There are some limitations to our study. Baseline measurements were obtained after the induction of anesthesia and Trendelenburg positioning. Therefore, all hemodynamic parameters were influenced by anesthesia, posture on operating room table [39], and mechanical ventilation.
All hemodynamic variations were recorded using the Pressure Recording Analytical Method. Although PRAM has been compared to the direct Fick and thermodilution method in normal weight individuals, this is the first study assessing SV and CO in the morbidly obese [11–15].
In conclusion, this study did not demonstrate deleterious effects in ventricular performance during laparoscopic surgery. Nevertheless, we believe that hemodynamic monitoring may be useful to assess the cardiovascular changes in obese patients during laparoscopy, especially in the event of sudden cardiovascular collapse. Less invasive hemodynamic monitoring, such as PRAM, is preferable to traditional invasive methods, such as pulmonary artery TDCO. Although obviating the risk of increased mortality, PRAM provides us with reliable beat-to-beat continuous monitoring, permitting instantaneous detection of pressure or volume-related alterations of the cardiovascular system. From an operational standpoint, PRAM requires but a peripheral arterial catheter and no external calibrations or preestablished input parameters [15].
References
Sharma KC, Brandstetter RD, Brensilver JM, et al. Cardiopulmonary physiology and pathophysiology as a consequence of laparoscopic surgery. Chest. 1996;110:810–15.
Fried M, Krska Z, Danzig V. Does the laparoscopic approach significantly affect cardiac functions in laparoscopic surgery? Pilot study in non obese and morbidly obese patients. Obes Surg. 2001;11:293–96.
Harris S, Ballantyne G, Luther M, et al. Alteration of cardiovascular performance during laparoscopic colectomy: a combined hemodynamic and echocardiographic analysis. Anesth Analg. 1996;83:482–7.
Alfonsi P, Vieillard-Baron A, Coggia M, et al. Cardiac function during intraperitoneal CO2 insufflation for aortic surgery: a transesophageal echocardiographic study. Anesth Analg. 2006;102:1304–10.
Dumont L, Mattys M, Massaut J, et al. Hemodynamic changes during laparoscopic gastroplasty in morbidly obese patients. Obes Surg. 1997;7:326–31.
Nguyen N, Fleming NW, Ho HS, et al. Cardiac function during laparoscopic vs open gastric bypass. Surg Endosc. 2002;16:78–83.
Westerband A, Van De Water J, Amzallag M, et al. Cardiovascular changes during laparoscopic cholecystectomy. Surg Gynecol Obstet. 1992;175:535–38.
Portera CA, Compton RP, Walters DN, et al. Benefit of pulmonary artery catheter and transesophageal echocardiographic monitoring in laparoscopic cholecystectomy patients with cardiac disease. Am J Surg. 1995;169:202–7.
Volpino P, Cangemi V, D’Andrea N, et al. Hemodynamic and pulmonary changes during and after laparoscopic cholecystectomy: a comparison with traditional surgery. Surg Endosc. 1998;12:119–23.
Artuso D, Wayne M, Cassaro S, et al. Hemodynamic changes during laparoscopic gastric bypass procedures. Arch Surg. 2005;140:289–92.
Scolletta S, Romano SM, Biagioli B, et al. Pressure recording analytical method (PRAM) for measurement of cardiac output during various hemodynamic states. Br J Anaesth. 2005;95:159–65.
Romano SM, Pistolesi M. Assessment of cardiac output from systemic arterial pressure in humans. Crit Care Med. 2002;30:1834–41.
Giomarelli P, Scolletta S, Biagioli B. Cardiac output monitoring by pressure recording analytical method in cardiac surgery. Eur J Cardiothorac Surg. 2004;26:515–20.
Romano SM, Scolletta S, Olivotto I, et al. Systemic arterial waveform analysis and assessment of blood flow during extracorporeal circulation. Perfusion. 2006;21:109–16.
Romano SM, Conti AA, Giglioli C, et al. Blood flow assessment by arterial pressure wave without external calibration. Comput Cardiol. 2006;33:293–6.
Reuter DA, Goetz AE. Arterial pulse contour analysis: applicability to clinical routine. In: Pinsky MR, Payen D, editors. Update in intensive care and emergency medicine. Germany: Springer; 2005. p. 381–95.
Berkenstadt H, Margalit N, Hadani M, et al. Stroke volume variation as a predictor of fluid responsiveness in patients undergoing brain surgery. Anesth Analg. 2001;92:984–89.
Hofer CK, Muller SM, Furre L, et al. Stroke volume and pulse pressure variation for prediction of fluid responsiveness in patients undergoing off-pump coronary artery bypass grafting. Chest. 2005;128:848–54.
Reuter DA, Goepfert MSG, Goresh T, et al. Assessing fluid responsiveness during open chest conditions. Br J Anaesth. 2005;94:318–23.
Romano SM, Olivotto I, Chiostri M, et al. Minimally invasive and noninvasive hemodynamic monitoring of the cardiovascular system: available options and future perspectives. Current Cardiology Reviews. 2006;l4:37–9.
Tulli G, Romano SM, Feminò R. Hemodynamic monitoring of septic patients with pressure recording analytical method (PRAM). In: Gullo A, editor. Anesthesia, pain, intensive care and emergency (APICE). Proceedings of the 20th postgraduate course in critical care medicine Trieste, 18–21, November 2005. Italy:Springer; 2005. Volume 20, p. 323–29.
Sorbara C, Romagnoli S, Rossi A, Romano SM. Circulatory failure: bedside functional haemodynamic monitoring. In: Atlee JL, Gullo A II, editors. Perioperative critical care cardiology. Italy: Springer-Verlag; 2007. p. 89–110.
Kashtan J, Green JF, Parsons EQ, et al. Hemodynamic effects of increased abdominal pressure. J Surg Res. 1981;30:249–55.
Punnonen R. Vasopressin release during laparoscopy: role of increased intra-abdominal pressure. Lancet. 1982;1:175–6.
Odeberg S, Ljungqvist O, Svenberg T, et al. Hemodynamic effects of pneumoperitoneum and the influence of posture during anesthesia for laparoscopic surgery. Acta Anaesthesiol Scand. 1994;38:276–83.
Girardis M, Broi UD, Antonutto G, et al. The effects of laparoscopic cholecystectomy on cardiovascular function and pulmonary gas exchange. Anesth Analg. 1996;83:134–40.
Haxby EJ, Gray MR, Rodriguez C, et al. Assessment of cardiovascular changes during laparoscopic hernia repair using oesophageal Doppler. Br J Anaesth. 1997;78:515–19.
Prior DL, Sprung J, Thomas JD, et al. Echocardiographic and hemodynamic evaluation of cardiovascular performance during laparoscopy of morbidly obese patients. Obes Surg. 2003;13:761–67.
Meininger D, Zwissler B, Byhahn C, et al. Impact of overweight and pneumoperitoneum on hemodynamics and oxygenation during prolonged laparoscopic surgery. World J Surg. 2006;30:520–26.
Joris JL, Noirot D, Legrand M, et al. Hemodynamic changes during laparoscopic cholecystectomy. Anesth Analg. 1993;76:1067–71.
Odeberg-Wernerman S, Sollevi A. Cardiopulmonary aspects of laparoscopic surgery. Curr Opin Anaesthesiol. 1996;9:529–35.
Ivankovitch D, Miletich DJ, Albrecht RF, et al. Cardiovascular effect of intraperitoneal insufflation with carbon dioxide and nitrous oxide in the dog. Anesthesiology. 1975;4:281–7.
Healy M, Strunin L. Anesthesia and laparoscopic cholecystectomy. In: Strunnin L, Thomson S, editors. Clinical anaesthesiology: the liver and anaesthesia. London: Baillière Tindall; 1992, p. 819–41.
Joris J, Lamy M. Modifications hemodinamiques au cours de la coeliochirurgie. In: Schoeffler P, editor. Anestesie pour coeliochirurgie. Paris:Masson; 1993. p. 11–23.
Gannedhal P, Odeberg S, Brodin LA. Effects of posture and pneumoperitoneum during anaesthesia on the indices of left ventricular filling. Acta Anaesthesiol Scand. 1996;40:160–6.
Wiesenack C, Prasser C, Rodig G, et al. Stroke volume variation as an indicator of fluid responsiveness using pulse contour analysis in mechanically ventilated patients. Anesth Analg. 2003;96:1254–7.
Söderström S, Sellgren J, Pontèn J. Aortic and radial pulse contour: different effects of nitroglycerin and prostacyclin. Anesth Analg. 1999;89:566–72.
Cunningham AJ, Turner J, Rosenbaum S, et al. Transoesophageal echocardiographic assessment of hemodynamic function during laparoscopic cholecystectomy. Br J Anaesth. 1993;70:621–5.
Romano SM, Lazzeri C, Chiostri M, et al. Beat to beat analysis of pressure wave morphology for pre-symptomatic detection of orthostatic intolerance during head-up tilt. J Am Coll Cardiol. 2004;44:1891–97.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Balderi, T., Forfori, F., Marra, V. et al. Continuous Hemodynamic Monitoring During Laparoscopic Gastric Bypass in Superobese Patients by Pressure Recording Analytical Method. OBES SURG 18, 1007–1014 (2008). https://doi.org/10.1007/s11695-007-9379-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-007-9379-5