Background
The study presents red blood cell (RBC) aggregability and deformability among obese patients qualified for bariatric surgery and its correlation with plasma lipid concentration.
Methods
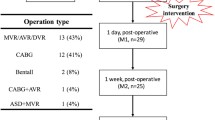
We studied 40 morbidly obese patients who were qualified for bariatric surgery: mean age was 43.5 ± 11.3 years, and mean body mass index (BMI) was 48.9 ± 7.7 kg/m2.The RBC deformability and aggregation parameters: aggregation index (AI), syllectogram amplitude (AMP) and aggregation half-time (t1/2) were measured by Laser-assisted Optical Rotational Cell Analyser - LORCA.
Results
Elongation index of RBC was significantly lower in obese patients than in the control group (P < 0.001) in 3.16–60.03 Pa shear stresses. Correlations between elongation index and triglyceride levels ranged between 0.42 to 0.44 (P < 0.05). AI was significantly higher in the obese patients (P < 0.001), t1/2 and the AMP were decreased (P < 0.001) compared to the control group. The RBC aggregation index correlated positively with total cholesterol level (r = 0.61, P < 0.05), non-HDL cholesterol level (r = 0.54, P < 0.05) and BMI (r = 0.48, P < 0.05). Negative correlation presented t1/2 with total cholesterol (r = −0.64, P < 0.05), non-HDL cholesterol (r = −0.51, P < 0.05) and BMI (r= −0.59, P < 0.05).
Conclusion
Obesity is associated with RBC rheological disturbances expressed by a decrease in RBC deformability, increased total aggregation extent and the alteration of kinetics of RBC aggregation. These results may suggest the necessity of introducing treatment forms to correct erythrocyte rheological properties, which may improve the blood-flow condition in the microcirculation and prevent postoperative complications after bariatric surgery.
Similar content being viewed by others
References
Silventoinen K, Sanas S, Tolonen H et al. WHO MONICA Project. Trends in obesity and energy supply in the WHO MONICA Project. Int J Obes 2004; 28: 710–8.
Milewicz A, Jedrzejuk D, Lwow F et al. Prevalence of obesity in Poland. Obes Rev 2005; 6: 113–4.
David BA, Fontaine KR. Annual deaths attributable to obesity in the United States. JAMA 1999; 282: 1530–8.
Pi-Sunyer FX. The medical risk of obesity. Obes Surg 2002; 12 (Suppl 1): S6–S11.
Sugerman HJ, Sugerman EL, Wolfe L et al. Risks and benefits of gastric bypass in morbidly obese patients with severe venous stasis disease. Ann Surg 2001; 234: 41–6.
Wu EC, Barba CA. Current practices in the prophylaxis of venous thromboembolism in bariatric surgery. Obes Surg 2000; 10: 7–12.
Hernandez GN, Lais C, Rasia ML. Effects of food restriction on hemorheological variables in a rat model of spontaneus hypertriglyceridemic obesity and diabetes. Clin Hemorheol Microcirc 2004; 31: 81–7.
Durussel JJ, Berthault MF, Guiffant G et al. Effects of red blood cell on the rat microcirculation blood flow. Acta Physiol Scand 1998; 163: 25–32.
Cabel M, Meiselman HJ, Popel AS et al. Contribution of red blood cell aggregation to venous vascular resistance in skeletal muscle. Am J Physiol 1997; 272: H1020–32.
Chabanel A, Zuccarelli F, Samama MM. Red cell aggregability increases with the severity of venous insufficiency. Int Angiol 1995; 14: 69–73.
Chabanel A, Horellou MH, Conard J et al. Red blood cell aggregability in patients with a history of leg vein thrombosis: influence of post-thrombotic treatment. Br J Hematol 1994; 88: 174–9.
Hardeman MR, Goedhart PT, Dobbe JGG et al. Laserassisted Optical Rotational Cell Analyser (LORCA); I. A new instrument for measurement of various structural hemorheological parameters. Clin Hemorheol 1994; 14: 605–18.
McHedlishvili G. Basic factors determining the hemorheological disorders in the microcirculation. Clin Hemorheol Microcirc 2004; 30: 179–80.
LeDevehat C, Khodabandehlou T, Dougny M. Études des paramètres hémorhélogiques dans l’obésité isolée. Diabete Metab 1992; 18: 43–7.
Valensi P, Smagghue O, Pariès J et al. Impairment of skin vasoconstrictive response to sympathetic activation in obese patients: influence of rheological disorders. Metabolism 2000; 49: 600–6.
Hardeman MR, Dobbe JGG, Ince C. The Laser-assisted Optical Rotational Cell Analyser (LORCA) as red blood cell aggregometer. Clin Hemorheol Microcirc 2001; 25: 1–11.
Sola E, Vaya A, Contreras T et al. Rheological profile in severe and morbid obesity. Preliminary study. Clin Hemorrheol Microcirc 2004; 30: 415–8.
Valensi P, Paries J, Maheo P et al. Erythrocyte rheological changes in obese patients: influence of hyperinsulinism. Int J Obes 1996; 20: 814–19.
Chien S, Usami S, Dellenbac RJ et al. Shear-dependent interaction of plasma proteins with erythrocytes in blood rheology. Am J Pysiol 1970; 219: 143–53.
Samocha-Bonet D, Ben-Ami R, Shapira I et al. Flow-resistant red blood cell aggregation in morbid obesity. Int J Obese 2004; 28: 1528–34.
Cicha I, Suzuki Y, Tateishi N et al. Effects of dietary triglycerides on rheological properties of human red blood cells. Clin Hemorheol Microcirc 2004; 30: 301–5.
Cignarelli M, Blonda M, Cospite MR et al. Alterations of erythrocyte lipid pattern and of some membrane related function as a consequence of plasma lipid disorder in diabetes mellitus. Diab Metab 1983; 9: 272–6.
Garnier M, Attali JR, Valensi P et al. Erythrocyte deformability in diabetes and erythrocyte membrane lipid composition. Metabolism 1990; 39: 794–8.
Yoshida H, Takamatsu S, Satoh K et al. Participation of serum albumin and LDL-cholesterol in impaired blood cell-filterability affected by white blood cells in patients with cerebral thrombosis. Scand J Clin Lab Invest 1992; 52: 641–6.
Uzun H, Zengin K, Taskin M et al. Changes in leptin, plasminogen activator factor and oxidative stress in morbidly obese patients following open and laparoscopic Swedish adjustable gastric banding. Obes Surg 2004; 14: 659–65.
Chiu D, Kuypers F, Lubin B. Lipid peroxidation in human red cells. Sem Hemat 1989; 26: 257–76.
Lubin C, Chiu D. Properties of vitamin E-deficient erythrocytes following peroxidant injury. Pediatr Res 1982; 16: 928–32.
Caimi G, Lo Presti R. Red cell Ca content (cytostolic and total) and erythrocyte membrane fluidity in vascular atheroslerotic disease. Clin Hemorheol 1991; 11: 617–21.
Klimes I, Nagulesparan M, Unger RH et al. Reduced Na, KATPase activity in intact red cells and isolated membranes from obese men. J Clin Endocrinol Metab 1982; 54: 721–24.
Levy Y, Elias N, Cogan U et al. Abnormal erythrocyte rheology in patients with morbid obesity. Angiology 1993; 44: 713–7.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wiewiora, M., Sosada, K., Wylezol, M. et al. Red Blood Cell Aggregation and Deformability among Patients Qualified for Bariatric Surgery. OBES SURG 17, 365–371 (2007). https://doi.org/10.1007/s11695-007-9066-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-007-9066-6