Abstract
Background
Over one in five Medicare patients discharged to skilled nursing facilities (SNFs) are re-hospitalized within 30 days of discharge. Poor communication between the hospital and SNF upon hospital discharge is frequently cited as the most common cause of readmission.
Aim
The goal of this program was to assess the ability of a weekly post-discharge hospitalist led virtual rounding program to augment the written discharge summary sent to SNFs.
Setting
Two academic hospitals and six SNFs in Baltimore, MD.
Participants
Hospitalists and medical directors or directors of nursing from the partner SNF.
Program Description
During weekly encounters, the hospitalist and SNF providers discussed the clinical status, discharge medications, treatment plan, and follow-up care of all discharged patients. The intervention took place from July 2021 to December 2021.
Program Evaluation
During the study, 544 patients were discussed in a post-discharge virtual encounter. After the discussions, hospitalists identified clinically significant errors in 124 discharge summaries. A survey of participating hospitalists and SNF medical and nursing leadership indicated the intervention was thought to improve care transitions.
Discussion
Our innovation was successful in identifying errors in discharge summaries and was thought to improve the transition of care by participating SNF and hospitalist providers.

Similar content being viewed by others
References
Medicare Payment Advisory Committee. Report to congress: Medicare payment policy. 2021.
Krumholz HM, Nuti SV, Downing NS, Normand ST, Wang Y. Mortality, hospitalizations, and expenditures for the medicare population aged 65 years or older, 1999-2013. JAMA. 2015;314(4):355-365.
Burke RE, Whitfield EA, Hittle D, et al. Hospital readmission from post-acute care facilities: Risk factors, timing, and outcomes. J Am Med Dir Assoc. 2016;17(3):249-255.
Mor V, Intrator O, Feng Z, Grabowski DC. The revolving door of rehospitalization from skilled nursing facilities. Health Aff. 2010;29(1):57-64.
Ouslander JG, Lamb G, Perloe M, et al. Potentially avoidable hospitalizations of nursing home residents: Frequency, causes, and costs: [See editorial comments by drs. jean F. wyman and william R. hazzard, pp 760–761]. J Am Geriatr Soc. 2010;58(4):627-635.
Ouslander JG, Naharci I, Engstrom G, et al. Root cause analyses of transfers of skilled nursing facility patients to acute hospitals: Lessons learned for reducing unnecessary hospitalizations. J Am Med Dir Assoc. 2016;17(3):256-262.
Vasilevskis EE, Ouslander JG, Mixon AS, et al. Potentially avoidable readmissions of patients discharged to post‐acute care: Perspectives of hospital and skilled nursing facility staff. J Am Geriatr Soc. 2017;65(2):269-276.
Clark BW, Baron K, Tynan‐McKiernan K, Britton MC, Minges KE, Chaudhry SI. Perspectives of clinicians at skilled nursing facilities on 30‐day hospital readmissions: A qualitative study. J Hosp Med. 2017;12(8):632-638.
Britton MC, Ouellet GM, Minges KE, Gawel M, Hodshon B, Chaudhry SI. Care transitions between hospitals and skilled nursing facilities: Perspectives of sending and receiving providers. Jt Comm J Qual Patient Saf. 2017;43(11):565-572.
Campbell Britton M, Petersen‐Pickett J, Hodshon B, Chaudhry SI. Mapping the care transition from hospital to skilled nursing facility. J Eval Clin Pract. 2020;26(3):786-790.
King BJ, Gilmore‐Bykovskyi AL, Roiland RA, Polnaszek BE, Bowers BJ, Kind AJ. The consequences of poor communication during transitions from hospital to skilled nursing facility: A qualitative study. J Am Geriatr Soc. 2013;61(7):1095-1102.
Gilmore-Bykovskyi AL, Roberts TJ, King BJ, Kennelty KA, Kind AJH. Transitions from hospitals to skilled nursing facilities for persons with dementia: A challenging convergence of patient and system-level needs. Gerontologist. 2017;57(5):867-879.
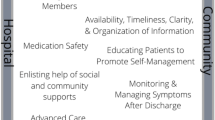
Valverde PA, Ayele R, Leonard C, Cumbler E, Allyn R, Burke RE. Gaps in hospital and skilled nursing facility responsibilities during transitions of care: A comparison of hospital and SNF clinicians’ perspectives. J Gen Intern Med. 2021;36(8):2251-2258.
Popejoy L, Galambos C, Vogelsmeier A. Hospital to nursing home transition challenges: Perceptions of nursing home staff. J Nurs Care Qual. 2014;29(2):103-109.
Krol ML, Allen C, Matters L, Graham AJ, English W, White HK. Health optimization program for elders: Improving the transition from hospital to skilled nursing facility. J Nurs Care Qual. 2019;34(3):217-222.
Moore AB, Krupp JE, Dufour AB, Sircar M, Travison TG, Abrams A, ..., Lipsitz LA. Improving transitions to postacute care for elderly patients using a novel video-conferencing program: ECHOcare transitions. Am J Med. 2017;130(10):1199–1204. https://www.sciencedirect.com/science/article/pii/S0002934317305259
Bellantoni J, Clark E, Wilson J, et al. Implementation of a telehealth videoconference to improve hospital‐to‐skilled nursing care transitions: Preliminary data. J Am Geriatr Soc. 2022.
Chess D, Whitman JJ, Croll D, Stefanacci R. Impact of after-hours telemedicine on hospitalizations in a skilled nursing facility. Am J Manag Care. 2018;24(8):385-388.
Groom LL, McCarthy MM, Stimpfel AW, Brody AA. Telemedicine and telehealth in nursing homes: An integrative review. J Am Med Dir Assoc. 2021;22(9):1784-1801. e7.
Groom LL, McCarthy MM, Stimpfel AW, Brody AA. Telemedicine and telehealth in nursing homes: An integrative review. J Am Med Dir Assoc. 2021;22(9):1784-1801. e7.
Gonzalez MR, Junge‐Maughan L, Lipsitz LA, Moore A. ECHO‐CT: An interdisciplinary videoconference model for identifying potential postdischarge Transition‐of‐Care events. J Hosp Med. 2021;16(2):93-96.
Krickus C, Aysola J, Ryskina K. Disparities in access to specialty care and emergency department use after hospital discharge to skilled nursing facility. J Hosp Med. 2022.
Farris G, Sircar M, Bortinger J, et al. Extension for community healthcare outcomes—care transitions: Enhancing geriatric care transitions through a multidisciplinary videoconference. J Am Geriatr Soc. 2017;65(3):598-602.
Tjia J, Bonner A, Briesacher BA, McGee S, Terrill E, Miller K. Medication discrepancies upon hospital to skilled nursing facility transitions. J Gen Intern Med. 2009;24(5):630-635.
Kerstenetzky L, Birschbach MJ, Beach KF, Hager DR, Kennelty KA. Improving medication information transfer between hospitals, skilled-nursing facilities, and long-term-care pharmacies for hospital discharge transitions of care: A targeted needs assessment using the intervention mapping framework. Res Soc Adm Pharm. 2018;14(2):138-145.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kuye, I.O., Dalal, S., Eid, S. et al. Hospitalists Improving Transitions of Care Through Virtual Collaborative Rounding with Skilled Nursing Facilities—the HiToC SNF Study. J GEN INTERN MED 38, 3628–3632 (2023). https://doi.org/10.1007/s11606-023-08345-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-023-08345-7