Abstract
Background
Dyskalemia involves critical electrolyte abnormalities and increases mortality risk in patients with acute clinical conditions. However, the association between dyskalemia and adverse outcomes in the general population is less well established.
Objective
To investigate the association of serum potassium levels with mortality and cardiovascular events in the general population and to explore the characteristics of individuals at high risk.
Design
A prospective cohort study.
Participants
A total of 5220 participants aged 50–79 years in the Chinese Multi-provincial Cohort Study.
Main Measures
Serum potassium levels were measured by the ion-selective electrode method. The outcomes were incident cardiovascular disease (CVD), CVD death, non-CVD death, and total death.
Key Results
Of the 5220 participants, 48.2% were men, and the mean age was 62.3 (SD 7.6) years. Hyperkalemia was found in 8.7% of the participants and was significantly associated with total death (hazard ratio [HR], 1.62; 95% confidence interval [CI], 1.18–2.23) and CVD death (HR, 2.12; 95% CI, 1.25–3.61) after adjustment. Furthermore, the HRs (95% CIs) of hyperkalemia combined with 2 and ≥ 3 risk factors were 2.37 (1.50–3.74) and 4.06 (2.37–6.95) for total death and 3.26 (1.56–6.80) and 8.42 (4.06–17.50) for CVD death, respectively. The 10-year cumulative incidence of total death was 17.4% for participants with 2 or more risk factors.
Conclusion
Hyperkalemia is associated with an increased risk of all-cause and CVD death, and this risk is more pronounced in patients with multiple risk factors. Our findings suggest that early identification and management of hyperkalemia in the general population are warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Potassium is the most abundant intracellular cation and plays a major role in maintaining normal functions of nerve and muscle. Dyskalemia involves critical electrolyte abnormalities, which may contribute to development of serious or life-threatening cardiac arrhythmias, including ventricular fibrillation, asystole, and cardiac arrest.1,2 It has already been known that abnormalities of potassium homeostasis are associated with adverse outcomes in patients with heart failure, acute myocardial infarction, or other acute medical conditions.3,4,5,6
However, the association between dyskalemia and adverse outcomes in the general population is less well established. Several previous studies reported that community-dwelling participants with high serum potassium levels had an increased risk of all-cause and cardiovascular disease (CVD) mortality compared with those with serum potassium levels in the normal range,7,8,9 whereas some studies failed to show this association.10,11,12 Moreover, a relationship between serum potassium levels and CVD events was not found in cohort studies in the US general populations.7,10 Therefore, whether dyskalemia is associated with mortality or cardiovascular events in the general population still awaits further investigation. With the fast population aging and the epidemic of hypertension, diabetes, and chronic kidney disease (CKD) which have been reported to relate to serum potassium levels,13 further studies on the risk associated with dyskalemia in the general population are important for early identification and intervention of dyskalemia and prevention of potential risk.
Therefore, we aimed to assess the association between serum potassium levels and adverse outcomes, including mortality and CVD events, using 10-year follow-up data from the population-based Chinese Multi-provincial Cohort Study (CMCS).
METHODS
Study Population
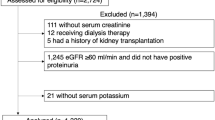
Study participants were recruited from the CMCS,14,15 which is an ongoing prospective, population-based cohort study. In brief, 27,003 participants aged 35 to 64 years were recruited from 11 provinces of China in 1992 and 1993, and 11,387 participants from 6 provinces were invited to a re-examination in 2007 to 2008. A total of 5966 participants took part in the re-examination,15 and 5220 participants with follow-up data till December 31, 2018, were included in this analysis after excluding individuals with established CVD (n = 417) or those with missing values of serum potassium measurement or other covariates at baseline (n = 329) (Supplementary Methods and Supplementary Figure 1). The protocol was approved by the Ethics Committee of Beijing An Zhen Hospital, Capital Medical University. Written informed consent was obtained from all participants.
Risk Factors
A standardized questionnaire was used to collect information for demographic information, smoking status, personal medical history, and medical therapy. Height, weight, waist circumference, and blood pressure levels were measured during physical examinations. Waist circumference was measured at a level midway between the lower rib margin and the iliac crest, while participants were semi-clothed. Body mass index was calculated as weight in kilograms divided by height in meters squared. Smoking was defined as at least 1 cigarette per day. Hypertension was defined as a systolic blood pressure ≥ 140 mm Hg and/or a diastolic blood pressure ≥ 90 mm Hg, or use of anti-hypertension drugs within 2 weeks. Diabetes was considered if fasting blood glucose levels were at least 7.0 mmol/L or a previously diagnosed diabetes was present. Venous blood samples were collected after at least 8 h of fasting and stored at − 80 °C without repeated freeze–thaw cycles to minimize any degradation. Serum potassium levels were measured by the ion-selective electrode method. Serum potassium levels < 3.5 mmol/L and ≥ 5.0 mmol/L were defined as hypokalemia and hyperkalemia, respectively.7,16 Fasting blood glucose and creatinine levels were measured by enzymatic methods. Low-density lipoprotein cholesterol and high-density lipoprotein cholesterol levels were measured by homogeneous assay. The estimated glomerular filtration rate (eGFR) was calculated using the Chronic Kidney Disease Epidemiology Collaboration equation,17 which is based on serum creatinine and cystatin C.
Outcomes
All participants were followed up for incident CVD, CVD death, non-CVD death, and death from all causes every 1–2 years by active interview, supplemented with linkage to local disease surveillance systems (Supplementary Methods). Diagnostic criteria of CVD events were based on the WHO-MONICA project and were modified following advances in diagnostic methods of myocardial infarction.15,18,19 Non-CVD death was defined as a death that was not related to CVD. All reported events and deaths were adjudicated by a panel of physicians including cardiologists and general physicians.
Statistical Analysis
Continuous variables are expressed as mean (SD) if normally distributed or median (interquartile range) if non-normally distributed. Categorical variables are expressed as frequencies and percentages. The 10-year cumulative incidence of each outcome was calculated using the Kaplan–Meier method by serum potassium levels (< 3.5 mmol/L, 3.5 to < 4.0 mmol/L, 4.0 to < 4.5 mmol/L, 4.5 to < 5.0 mmol/L, and ≥ 5.0 mmol/L). Moreover, the 10-year cumulative incidence of CVD death, non-CVD death, and CVD events was calculated using the Aalen–Johansen estimator considering competing risk. Kaplan–Meier curves were plotted for the 5 serum potassium levels to illustrate the cumulative incidence of total death, CVD death, non-CVD death, and CVD events. Log-rank test was used to test the null hypothesis of no difference overall in survival distributions between the groups. The Cox proportional hazards model was used to calculate the hazard ratios (HRs) and 95% confidence intervals (95% CIs) of total death, CVD death, non-CVD death, and CVD events associated with different serum potassium levels. The model was adjusted for age, sex, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, smoking, hypertension, diabetes, eGFR, use of potassium-altering medications (diuretics, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and β-blockers), and use of statins at baseline. Combining individuals with serum potassium levels of 3.5 to < 4.0 mmol/L, 4.0 to < 4.5 mmol/L, and 4.5 to < 5.0 mmol/L, participants with serum potassium levels of 3.5 to < 5.0 mmol/L were considered as a reference post hoc in the models. By examining plots of Schoenfeld residuals, the proportionality of the hazards assumptions was tested and fulfilled. Sensitivity analyses were conducted a priori in participants who were not on potassium-altering drugs including diuretics, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and β-blockers at baseline (n = 4225). Additionally, we performed the Fine and Gray competing risk regression analysis to consider competing risk. Furthermore, the 10-year cumulative incidence of CVD event and mortality was assessed a priori in participants with hyperkalemia combined with different numbers of risk factors, including age ≥ 60 years, eGFR < 60 mL/min/1.73 m2, diabetes, and hypertension, using the Kaplan–Meier method. The Cox proportional hazards model was used to estimate the HRs and 95% CIs of adverse outcomes associated with hyperkalemia combined with different numbers of risk factors after adjustment for other covariates. Sensitivity analyses were conducted after taking competing risk into consideration. All statistical tests were two-sided, and P < 0.05 was considered statistically significant for all analyses. Statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC) and the R software (version 4.0.2).
Results
Study Population and Baseline Characteristics
During the follow-up period (median, 10.5 years; 51,541.8 person-years), there were 352 deaths, including 97 CVD deaths and 255 non-CVD deaths. When CVD deaths and nonfatal CVD events were combined, there were 519 CVD events during the follow-up (Supplementary Figure 1). The mean age of the participants was 62.3 (SD 7.6, range 50–79) years and 48.2% were men. Overall, 1.5% of the participants had hypokalemia and 8.7% had hyperkalemia. At baseline, 14.9% of the participants had diabetes, 55.7% had hypertension, and 19.1% were on drugs that may alter serum potassium levels. Participants with hypokalemia were older and more likely to be men. Levels of fasting blood glucose, total cholesterol, low-density lipoprotein cholesterol, and diastolic blood pressure and the prevalence of diabetes tended to increase with serum potassium. Participants with either hypokalemia or hyperkalemia had a lower eGFR level but higher level of systolic blood pressure and rates of smoking and hypertension, compared with those with serum potassium levels at 3.5 to < 5.0 mmol/L (Table 1).
Serum Potassium Levels, Mortality, and Cardiovascular Incidence
Participants with either hypokalemia or hyperkalemia had a higher 10-year cumulative incidence of all-cause mortality, non-CVD mortality, and CVD events (Fig. 1). Such a U-shaped relationship with serum potassium was not found for CVD death because no CVD death occurred in participants with hypokalemia. The results were similar after considering competing risk (Supplementary Figure 2). Kaplan–Meier curves showed significant differences among participants in the 5 serum potassium categories for total mortality, CVD mortality, and non-CVD mortality. The survival curves of all-cause and non-CVD mortality diverged right after 1 year for participants with hypokalemia, and the curves of all-cause and CVD mortality diverged after 3.5 years for those with hyperkalemia. The difference in the incidence of CVD was not statistically significance (P = 0.36) (Fig. 2).
No significantly higher risk of mortality or incident CVD events was found for participants with hypokalemia after adjusting for covariates compared with those with normokalemia (Fig. 3). However, participants with hyperkalemia were associated with a significantly higher risk of total death (HR, 1.62; 95% CI, 1.18–2.23) and CVD death (HR, 2.12; 95% CI, 1.25–3.61). These associations were not significant between hyperkalemia and non-CVD death (HR, 1.39; 95% CI, 0.93–2.09) or incidence of CVD (HR, 1.13; 95% CI, 0.84–1.51). Contribution of the covariates in models is listed in Supplementary Table 1. Similar associations were found in participants not using potassium-altering drugs at baseline, except that the association between hyperkalemia and total death became non-significant (HR, 1.43; 95% CI, 0.98–2.10; P = 0.007) (Supplementary Figure 3), and after considering the competing risk (Supplementary Figure 4).
Risk of Mortality and Cardiovascular Events Associated with Hyperkalemia Combined with Other Risk Factors
The association of hyperkalemia with the incidence of CVD and total mortality was further assessed taking into account the number of combined risk factors (age ≥ 60 years, diabetes, hypertension, and eGFR < 60 mL/min/1.73·m2). Among participants with hyperkalemia, 82.0% had at least 1 of the 4 risk factors, and 45.3% had multiple risk factors. No death or CVD event occurred in hyperkalemia patients without any of the 4 risk factors, whereas the absolute risk of all outcomes was significantly increased in those with hyperkalemia combined with 2 or more risk factors compared with participants with normokalemia (Table 2). The 10-year cumulative incidence of total death, CVD death, non-CVD death, and CVD events was significantly increased with the number of risk factors. The 10-year cumulative incidence was 17.4% for total death, 9.0% for CVD death, 9.3% for non-CVD death, and 19.3% for CVD events in participants with hyperkalemia and 2 or more risk factors. Among those with hyperkalemia and 3 or more risk factors, the 10-year cumulative incidence of total death was 24.4%. After adjusting for other covariates in the Cox proportional hazards regression model, the HRs (95% CIs) of hyperkalemia combined with 2 and ≥ 3 risk factors were 2.37 (1.50–3.74) and 4.06 (2.37–6.95) for total death and 3.26 (1.56–6.80) and 8.42 (4.06–17.50) for CVD death, respectively (Table 2). Results did not alter much after considering competing risks (Supplementary Table 2).
Discussion
In this large cohort of 5220 participants from the general population with longer than 10 years of follow-up, we found that hyperkalemia was associated with a higher risk of all-cause and CVD death. The 10-year cumulative incidence of all-cause death exceeded 10% in individuals with hyperkalemia and 2 or more of the following 4 risk factors: older age, low eGFR, diabetes, and hypertension.
Hyperkalemia is a common electrolyte disorder, which is associated with an increased risk of mortality in patients with high-risk clinical conditions.3,4,5,6 However, the association between high serum potassium levels and all-cause or CVD mortality in the general population is less well established. Several studies related hyperkalemia with total or CVD mortality.7,8,9 However, in the Framingham Offspring Study, a non-significant association between serum potassium levels and CVD mortality was found, possibly owing to relatively few individuals died of CVD during follow-up and limited statistical power.10 In the Copenhagen City Heart Study and a study in elderly Taiwanese, the association between hyperkalemia and mortality was non-significant or borderline significant, possibly due to the lower cut-off value of hyperkalemia (a serum potassium level of 4.5 mmol/L) than most other studies.11,12 Consistent with the majority of previous studies,7,8,9 we observed that hyperkalemia defined as a serum potassium level ≥ 5 mmol/L was significantly associated with mortality. Moreover, most previous studies had baseline potassium measurements conducted in the last century among Western populations.7,8,9,10 For decades, lifestyles have undergone dramatic changes, with a consequent increase in chronic conditions associated with hyperkalemia, such as diabetes, CKD, and hypertension.20,21,22 Our study provides contemporary evidence of the risk associated with high serum potassium levels in the Chinese general population, which has marked differences in lifestyle, particularly the dietary pattern related to potassium levels, compared with Western populations.23,24,25
To the best of our knowledge, only two previous studies have evaluated the association of serum potassium levels with incident CVD events in the general population.7,10 Neither of these reports which were based on the Framingham Offspring Study and the Multi-Ethnic Study of Atherosclerosis and the Cardiovascular Health Study showed a significant association between serum potassium levels and the incidence of CVD in the US population. Our findings from Chinese community-living adults who were free of CVD at baseline are consistent with those from previous studies in the Western population.7,10
The association of serum potassium levels with mortality, particularly CVD mortality, rather than the incidence of CVD, may be mainly explained by the mechanisms of potassium homeostasis. Extracellular potassium levels are strictly controlled to maintain the resting membrane potential of excitable cells. The most plausible mechanism whereby hyperkalemia could cause death is by induction of fatal cardiac arrhythmia.2 It has been reported that hyperkalemia increases the risk of ventricular arrhythmia in patients with acute myocardial infarction.26 This suggests a potential mechanistic explanation for why hyperkalemia is primarily associated with CVD death.
Hyperkalemia is common, particularly in patients with comorbidities. Notably, we found that associations between hyperkalemia and adverse outcomes were consistently of greater magnitude in individuals with hyperkalemia and multiple risk factors, including older age, low eGFR, diabetes, and hypertension. The risk of all-cause and CVD death was 4.06 and 8.42 times higher, respectively, in participants with hyperkalemia and 3 or more risk factors compared with those with normokalemia. Moreover, the 10-year cumulative incidence of total mortality in participants with hyperkalemia reached 17.4% when combined with 2 or more risk factors and reached 24.4% with 3 or more risk factors. The similar but slightly attenuated association between hyperkalemia and total mortality in participants without using of potassium-altering drugs could also be explained by the exclusion of the high-risk individuals who were on drugs, in addition to the smaller sample size. Similarly, a study on an electronic medical record database including 911,698 individuals from a geographically diverse US population showed a mortality rate of 35.7% in those with hyperkalemia and heart failure, CKD, or diabetes.27 In contrast, the death rate was only 2.7% in the control group without known CVD, acute myocardial infraction, hypertension, heart failure, CKD, or diabetes in this previous study. The prevalence of hypertension, diabetes, and CKD is high in the general population, especially in older people. In China, 253 million people are over the age of 60; 245 million adults are estimated to have hypertension, 90 million to have diabetes, and 132 million to have CKD.21,28,29 In fact, 82.0% of the participants with hyperkalemia combined with at least 1 of those factors in our study. Therefore, these findings highlight the importance of early detection and management of hyperkalemia in routine clinical practice. Patients with hyperkalemia warrant close follow-up and management when they have multiple comorbidities.
Although studies have shown that hypokalemia is associated with adverse outcomes in patients with comorbidities, such as heart or renal failure,30,31 the results from studies in the general population are controversial. In most previous studies, an association between hypokalemia and mortality or the incidence CVD was not found after full adjustment of covariates.7,8,9,10 Our study showed a higher 10-year risk of all-cause mortality, non-CVD mortality, and incident CVD event in the hypokalemia group than in the normokalemia group. Unlike the higher risk of all-cause mortality that may be driven by both CVD and non-CVD mortality in patients with hyperkalemia, the higher risk of all-cause mortality could be merely driven by the non-CVD mortality in patients with hypokalemia, as there was no CVD mortality in this group. However, consistent with most previous studies,7,8,9,10 no significant associations were found between hypokalemia and these outcomes after adjusting for confounding factors. These negative findings may have been caused by a relatively small number of participants in the hypokalemia group.10 Another interpretation is that the risk associated with hypokalemia may be largely explained by other risk factors, such as older age, a higher prevalence of hypertension, and the use of diuretics.7,8,9 In contrast, two previous studies also showed that hypokalemia was significantly associated with an increased risk of all-cause or CVD death among community-dwelling individuals.11,12 Therefore, future studies with a larger sample size of participants with hypokalemia are required to further assess its associated risk.
Although our data are observational and cannot demonstrate causality, our results may be of great value in preventing the risk associated with hyperkalemia. The prevalence of hyperkalemia has been increasing owing to the increase in risk factors associated with hyperkalemia, such as population aging, CKD, diabetes, hypertension, and wide use of renin–angiotensin–aldosterone system inhibitors.13 The prevalence of hyperkalemia defined as the serum potassium level ≥ 5.5 mEq/L was reported to be 2.7% in Chinese older adults, while this rate increased to 9.1%, 5.4%, and 3.4% in those with CKD, diabetes, and hypertension, respectively.13 Despite the potential risk of hyperkalemia, there are few standard treatment paradigms for outpatients. A low potassium diet is restrictive and deprives patients of many healthy food choices. Among patients who are receiving drugs that may raise serum potassium levels, such as renin–angiotensin–aldosterone system inhibitors, hyperkalemia may affect adherence to treatment of these drugs. Therefore, identifying patients with hyperkalemia and multiple risk factors and initiating early intervention that reduces potassium levels safely and effectively are essential.32,33,34,35
The strengths of this study include its long-term follow-up, the standardized procedures for data collection, and adjudication of suspected CVD using detailed evaluation criteria in the CMCS. However, several limitations in our study need to be considered. First, the analysis on the association between hypokalemia and clinical outcomes may have been underpowered because there were only 76 participants with serum potassium levels < 3.5 mmol/L. Second, no death or CVD event occurred in patients with hyperkalemia with none of the 4 risk factors, which precluded us from evaluating the risk associated with hyperkalemia alone. Third, levels of risk factors and serum potassium may change during the long-term follow-up, and the definition of dyskalemia based on a one-time measurement of serum potassium level may subject to misclassification. Additionally, owing to the observational design, residual confounding might have contributed to the findings.
Conclusion
In summary, in this large, long-term cohort study in the general population, hyperkalemia was associated with an increased risk of all-cause and CVD mortality, and this risk was particularly high in those with multiple risk factors. Our study provides evidence for identifying individuals with a hyperkalemia-related higher risk of all-cause and CVD mortality.
References
Mattsson N, Sadjadieh G, Kumarathurai P, Nielsen OW, Kober L, Sajadieh A. Ambulatory cardiac arrhythmias in relation to mild hypokalaemia and prognosis in community dwelling middle-aged and elderly subjects. Europace. 2016;18(4):585-591.
Patel RB, Tannenbaum S, Viana-Tejedor A, et al. Serum potassium levels, cardiac arrhythmias, and mortality following non-ST-elevation myocardial infarction or unstable angina: insights from MERLIN-TIMI 36. Eur Heart J Acute Cardiovasc Care. 2017;6(1):18-25.
Ferreira JP, Mogensen UM, Jhund PS, et al. Serum potassium in the PARADIGM-HF trial. Eur J Heart Fail. 2020;22(11):2056-2064.
Goyal A, Spertus JA, Gosch K, et al. Serum potassium levels and mortality in acute myocardial infarction. JAMA. 2012;307(2):157-164.
Krogager ML, Eggers-Kaas L, Aasbjerg K, et al. Short-term mortality risk of serum potassium levels in acute heart failure following myocardial infarction. Eur Heart J Cardiovasc Pharmacother. 2015;1(4):245-251.
Yusuf AA, Hu Y, Singh B, Menoyo JA, Wetmore JB. Serum potassium levels and mortality in hemodialysis patients: a retrospective cohort study. Am J Nephrol. 2016;44(3):179-186.
Hughes-Austin JM, Rifkin DE, Beben T, et al. The relation of serum potassium concentration with cardiovascular events and mortality in community-living individuals. Clin J Am Soc Nephrol. 2017;12(2):245-252.
Chen Y, Chang AR, McAdams DeMarco MA, et al. Serum potassium, mortality, and kidney outcomes in the atherosclerosis risk in communities study. Mayo Clin Proc. 2016;91(10):1403-1412.
Fang J, Madhavan S, Cohen H, Alderman MH. Serum potassium and cardiovascular mortality. J Gen Intern Med. 2000;15(12):885-890.
Walsh CR, Larson MG, Leip EP, Vasan RS, Levy D. Serum potassium and risk of cardiovascular disease: the Framingham Heart Study. Arch Intern Med. 2002;162(9):1007-1012.
Lai YH, Leu HB, Yeh WT, Chang HY, Pan WH. Low-normal serum potassium is associated with an increased risk of cardiovascular and all-cause death in community-based elderly. J Formos Med Assoc. 2015;114(6):517-525.
Mattsson N, Nielsen OW, Johnson L, et al. Prognostic impact of mild hypokalemia in terms of death and stroke in the general population-a prospective population study. Am J Med. 2018;131(3):318.e9-318.e19.
Jin A, Zhao M, Sun Y, et al. Normal range of serum potassium, prevalence of dyskalaemia and associated factors in Chinese older adults: a cross-sectional study. BMJ Open. 2020;10(10):e039472.
Liu J, Hong Y, D’Agostino RB, Sr., et al. Predictive value for the Chinese population of the Framingham CHD risk assessment tool compared with the Chinese Multi-Provincial Cohort Study. JAMA. 2004;291(21):2591-2599.
Qi Y, Han X, Zhao D, et al. Long-term cardiovascular risk associated with stage 1 hypertension defined by the 2017 ACC/AHA Hypertension Guideline. J Am Coll Cardiol. 2018;72(11):1201-1210.
Nunez J, Bayes-Genis A, Zannad F, et al. Long-term potassium monitoring and dynamics in heart failure and risk of mortality. Circulation. 2018;137(13):1320-1330.
Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604-612.
Wu Z, Yao C, Zhao D, et al. Sino-MONICA project: a collaborative study on trends and determinants in cardiovascular diseases in China, part I: morbidity and mortality monitoring. Circulation. 2001;103(3):462-468.
Luepker RV, Apple FS, Christenson RH, et al. Case definitions for acute coronary heart disease in epidemiology and clinical research studies: a statement from the AHA Council on Epidemiology and Prevention; AHA Statistics Committee; World Heart Federation Council on Epidemiology and Prevention; the European Society of Cardiology Working Group on Epidemiology and Prevention; Centers for Disease Control and Prevention; and the National Heart, Lung, and Blood Institute. Circulation. 2003;108(20):2543-2549.
Hu C, Jia W. Diabetes in China: Epidemiology and Genetic Risk Factors and Their Clinical Utility in Personalized Medication. Diabetes. 2018;67(1):3-11.
Collaboration GBDCKD. Global, regional, and national burden of chronic kidney disease, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2020;395(10225):709-733.
Collaborators GBDRF. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223-1249.
Du S, Batis C, Wang H, Zhang B, Zhang J, Popkin BM. Understanding the patterns and trends of sodium intake, potassium intake, and sodium to potassium ratio and their effect on hypertension in China. Am J Clin Nutr. 2014;99(2):334-343.
Whelton PK. Sodium and potassium intake in US adults. Circulation. 2018;137(3):247-249.
Saje SM, Endris BS, Nagasa B, Ashebir G, Gebreyesus SH. Dietary sodium and potassium intake: knowledge, attitude and behaviour towards dietary salt intake among adults in Addis Ababa, Ethiopia. Public Health Nutr. 2020:1-9.
Hoppe LK, Muhlack DC, Koenig W, Carr PR, Brenner H, Schottker B. Association of abnormal serum potassium levels with arrhythmias and cardiovascular mortality: a systematic review and meta-analysis of observational studies. Cardiovasc Drugs Ther. 2018;32(2):197-212.
Collins AJ, Pitt B, Reaven N, et al. Association of serum potassium with all-cause mortality in patients with and without heart failure, chronic kidney disease, and/or diabetes. Am J Nephrol. 2017;46(3):213-221.
Wang Z, Chen Z, Zhang L, et al. Status of hypertension in China: results from the China Hypertension Survey, 2012-2015. Circulation. 2018;137(22):2344-2356.
Liu M, Liu SW, Wang LJ, et al. Burden of diabetes, hyperglycaemia in China from to 2016: Findings from the 1990 to 2016, global burden of disease study. Diabetes Metab. 2019;45(3):286-293.
Bowling CB, Pitt B, Ahmed MI, et al. Hypokalemia and outcomes in patients with chronic heart failure and chronic kidney disease: findings from propensity-matched studies. Circ Heart Fail. 2010;3(2):253-260.
Ohnishi T, Kimachi M, Fukuma S, Akizawa T, Fukuhara S. Postdialysis hypokalemia and all-cause mortality in patients undergoing maintenance hemodialysis. Clin J Am Soc Nephrol. 2019;14(6):873-881.
Chang AR, Sang Y, Leddy J, et al. Antihypertensive medications and the prevalence of hyperkalemia in a large health system. Hypertension. 2016;67(6):1181-1188.
Lepage L, Dufour AC, Doiron J, et al. Randomized clinical trial of sodium polystyrene sulfonate for the treatment of mild hyperkalemia in CKD. Clin J Am Soc Nephrol. 2015;10(12):2136-2142.
Packham DK, Rasmussen HS, Lavin PT, et al. Sodium zirconium cyclosilicate in hyperkalemia. N Engl J Med. 2015;372(3):222-231.
Weir MR, Bakris GL, Bushinsky DA, et al. Patiromer in patients with kidney disease and hyperkalemia receiving RAAS inhibitors. N Engl J Med. 2015;372(3):211-221.
Acknowledgements
The authors are grateful to all the investigators from participating centers in CMCS study for providing data collection.
Funding
This work was supported by the National Key Research and Development Program of China (2016YFC0900902), the National Natural Science Foundation of China (82073635), and the Beijing Nova Programme Interdisciplinary Cooperation Project (Z191100001119017).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily reflect the position or policy of Duke University, the US Department of Veterans Affairs, or the US government.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 484 kb)
Rights and permissions
About this article
Cite this article
Liu, S., Zhao, D., Wang, M. et al. Association of Serum Potassium Levels with Mortality and Cardiovascular Events: Findings from the Chinese Multi-provincial Cohort Study. J GEN INTERN MED 37, 2446–2453 (2022). https://doi.org/10.1007/s11606-021-07111-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-021-07111-x