Abstract
Background
The patient-centered medical home (PCMH) is a primary care delivery model predicated on shared responsibility for patient care among members of an interprofessional team. Effective task sharing may reduce burnout among primary care providers (PCPs). However, little is known about the extent to which PCPs share these responsibilities, and which, if any, of the primary care tasks performed independently by the PCPs (vs. shared with the team) are particularly associated with PCP burnout. A better understanding of the relationship between these tasks and their effects on PCP burnout may help guide focused efforts aimed at reducing burnout.
Objective
To investigate (1) the extent to which PCPs share responsibility for 14 discrete primary care tasks with other team members, and (2) which, if any, of the primary care tasks performed by the PCPs (without reliance on team members) are associated with PCP burnout.
Design
Secondary data analysis of Veterans Health Administration (VHA) survey data from two time periods.
Participants
327 providers from 23 VA primary care practices within one VHA regional network.
Main Measures
The dependent variable was PCP report of burnout. Independent variables included PCP report of the extent to which they performed 14 discrete primary care tasks without reliance on team members; team functioning; and PCP-, clinic-, and system-level variables.
Key Results
In adjusted models, PCP reports of intervening on patient lifestyle factors and educating patients about disease-specific self-care activities, without reliance on their teams, were significantly associated with burnout (intervening on lifestyle: b = 4.11, 95% CI = 0.39, 7.83, p = 0.03; educating patients: b = 3.83, 95% CI = 0.33, 7.32, p = 0.03).
Conclusions
Performing behavioral counseling and self-management education tasks without relying on other team members for assistance was associated with PCP burnout. Expanding the roles of nurses and other healthcare professionals to assume responsibility for these tasks may ease PCP burden and reduce burnout.
Similar content being viewed by others
INTRODUCTION
In response to growing demands for increased access and improved care management in primary care settings, patient care has shifted away from a provider-centric approach, toward a team-based model of care delivery, where physicians work in collaboration with other members of an interprofessional team to deliver longitudinal, coordinated patient care.1 This team-based approach is a key aspect of the patient-centered medical home (PCMH) model of care.2,3, – 4
While the concept of the PCMH has been around since the 1960s, there has been a recent increase in adoption and implementation of this model in primary care settings, especially after the passage of the Affordable Care Act (ACA), which included several provisions promoting the PCMH. Early implementation studies have been promising, with reports of positive patient experiences, reduced emergency room visits and hospital utilization, and improved clinical outcomes.1 , 5,6,7, – 8 However, multiple challenges associated with transitioning to a team-based model of care may have led to the unintended consequence of creating new stresses for PCPs, resulting in burnout.3 – 5 , 9 Understanding the relationship between PCMH implementation and provider burnout is critical, as provider burnout has been linked to lower quality of care,10 , 11 increased medical errors,11 , 12 poorer patient health outcomes,13,14, – 15 lower patient satisfaction,14 , 16 and overuse of resources/increased healthcare costs.17 , 18
A number of recent studies have investigated the effect of PCMH implementation on levels of burnout among PCPs and interprofessional team members.3 – 6 , 9 Some studies found that the pressure for constant change associated with PCMH implementation and maintenance increased PCP burnout,5 , 9 while other studies reported that various elements of the PCMH model, such as self-efficacy for PCMH changes, participatory decision making,3 , 4 appropriate staffing,3 , 6 and practicing at top levels of competence,3 helped to mitigate burnout among PCPs and team members.
Previous works have posited that effective task sharing between PCMH team members may help to reduce PCP and staff burnout;2 , 19,20,21, – 22 however, few studies have empirically investigated this relationship. One study tested the relationship between a group of primary care tasks (e.g., patient care, patient assessment, responding to messages) and PCP and staff burnout, but the results were inconclusive.3 The present study investigates (1) the extent to which PCPs share responsibility for 14 discrete primary care tasks with other team members, and (2) which, if any, of the primary care tasks performed by the PCPs (without reliance on team members) are associated with PCP burnout.
METHODS
Study Setting and Participants
In 2010, the Veteran Health Administration (VHA) implemented a program featuring Patient-Aligned Care Teams (PACT), a PCMH model of patient care delivery in primary care settings. PACT “teamlets” are comprised of a PCP (i.e., physician, nurse practitioner, or physician assistant) and three supporting team members: a registered nurse (RN) care manager, a licensed vocational/practical nurse (LVN/LPN), and a medical assistant or clerical staff.23,24,25,26, – 27The teamlets are supported by extended team members from other disciplines, including pharmacists, nutritionists/dieticians, and social workers.
The Veterans Assessment and Improvement Laboratory (VAIL) examined the implementation of PACT across one Veterans Integrated Service Network (VISN), which consisted of 23 primary care clinics in five healthcare systems. The VAIL-Patient Centered Care (PCC) Clinician Survey was developed as part of the VAIL evaluation. This web-based survey, administered by the RAND Corporation, included approximately 130 items assessing PCP experiences with PACT implementation, including their perceptions of PACT and factors that enabled or hindered implementation. Both the VHA and RAND institutional review boards approved this study.4
The secondary data analysis presented here explores the relationship between task reliance and PCP burnout using responses from the VAIL-PCC Clinician Survey. Our analysis includes combined data collected in wave 1 (November 2011 to March 2012) and wave 2 (August 2013 to January 2014). The total participants included 327 PCPs (n = 191, response rate = 54% in wave 1; n = 136, response rate = 39% in wave 2), among whom 69 participated in both waves.
Dependent Variable: Emotional Exhaustion Scale of Burnout
PCP burnout was measured using the emotional exhaustion subscale of the Maslach Burnout Inventory,28 which has demonstrated high reliability (α = 0.92).4 Items included statements such as “I feel emotionally drained from my work” and “I feel burned out from my work.” Response options for each of the nine items ranged from “never” (0) to “every day” (6). Scale scores ranged from 0 to 54.
Key Independent Variables
PCP Report of Performing Tasks Without Reliance on Team Members
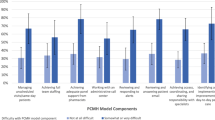
The VAIL-PCC Clinician Survey includes questions about 14 primary care tasks representing four general categories: (1) patient assessment and treatment decisions; (2) patient counseling and self-management education; (3) following up with other clinician requests; and (4) following up with patient requests (Table 1). The 14 tasks were chosen by the study team based on the literature and clinical experience.24 Survey items were intentionally worded in a discipline-neutral manner, as some aspects of each task could potentially be performed within their scope of practice by various members of the PCMH team. Survey items were pilot-tested with a group of PCPs and primary care staff, and refined based on feedback.4
In this study, we measured PCP reports of the extent to which each of the 14 discrete primary care tasks were performed by the PCP without reliance on team members, using the following response options: (a) “I typically do this on my own without help,” or “I most often rely on help from (b) my teamlet members, (c) my colleagues outside the team, but at my local site, (d) my colleagues outside my local site.” In an effort to capture tasks performed independently by the PCPs versus tasks for which PCPs relied on immediate members of their assigned teams, we dichotomized the responses, with “1” indicating that they performed the task without reliance on teamlet members, and “0” indicating that they most often relied on help from their teamlet members. We excluded responses (c) and (d) from the analysis, which combined represented less than 5%.
Covariates
PCP Report of Team Function
Because previous studies have shown that team functioning is correlated with burnout,3 , 29 , 30 we included three measures of team functioning: (1) team communication, (2) team knowledge and skills, and (3) satisfaction with their teamlet, to control for the effect on PCP reports of burnout.
Team communication was measured using a four-item scale (α = 0.84) derived from the Survey of Organizational Attributes for Primary Care.31 The scale includes statements such as, “In this clinic, co-workers from different clinical or administrative backgrounds frequently interact to solve quality of care problems.” Response options for each item ranged from “strongly disagree” (0) to “strongly agree” (5). Total scores ranged from 0 to 20. This measure was dichotomized into low versus high team communication by dividing at the median score of 13.
Team knowledge and skills were measured by a six-item scale (α = 0.75)4 from the Team Diagnostic Survey developed by Wageman and colleagues.32 Items included statements such as “Everyone in this team has the special skills that are needed for team work.” Response options for each item ranged from “strongly disagree” (0) to “strongly agree” (5). The total score ranged from 0 to 30. This measure was dichotomized into low and high team knowledge and skills by dividing at the median score of 21.
PCPs' satisfaction with their teamlets was measured by a single item: “Overall, I am satisfied with the help I receive from my teamlet.” Response options were “strongly disagree” (0) to “strongly agree” (5). Scores ranged from 0 to 5. This measure was also dichotomized into low and high team satisfaction by dividing at the median score of 4.
PCP-, Clinic-, and System-Level Characteristics
Burnout can also be influenced by PCP-, clinic-, and system-level characteristics.4 Therefore, we also controlled for provider age, gender, race/ethnicity, provider type, and VHA tenure. In addition, we controlled for the location of the clinic and specific healthcare system.
Analyses
The final sample included 327 PCPs; 258 participated in either wave 1 or 2, and 69 PCPs participated in both waves. Analysis of variance analysis (ANOVA) was performed to examine provider responses between waves 1 and 2. No statistically significant differences were found; therefore, to increase statistical power, responses from the two waves were combined. We analyzed the survey data using different methods (e.g., repeated measures and multi-level models) to control for clustering of responses within individuals.
Univariate analysis was performed to describe the level of burnout, task reliance, team functioning, and demographics of the provider, clinic, and healthcare system. We used bivariate analyses to explore the potential relationship between the independent variables and PCP burnout as a strategy for identifying candidate relationships for further exploration. Bonferroni corrections were applied to address possible type 1 errors related to multiple comparisons in the bivariate analysis.
PCP reports of tasks performed independently that had a statistically significant association (p ≤ 0.004) with PCP burnout in the bivariate analysis were included in multivariable linear regression analysis. Separate models were conducted for each PCP report of tasks performed without reliance on the team, controlling for covariates. All multivariate models adjusted for time (wave) and clustering within individuals using Stata version 13.0 software (StataCorp LP, College Station, TX). In addition to the analyses described above, we performed sensitivity analyses by re-running the multivariable linear regressions as multi-level models, adjusting for clustering within individuals (level 1) and healthcare systems (level 2). We also performed sensitivity analyses with non-linear models to assess the robustness of our findings. We ran multi-level logistic regression analysis with the burnout categorized as high versus medium or low burnout, controlling for clustering over time, clinic, and healthcare system. The results were unchanged across analyses.
RESULTS
PCP Burnout, Reports of Performing Tasks on Their Own, and Other Study Variables
Table 2 shows results for burnout levels, PCP reports of the extent to which they performed each task without reliance on the team, and other study variables for the overall sample (n = 327, adjusting for the 69 responses by PCPs who responded in both waves). PCPs reported that they experienced a medium level33 (mean = 23.1; SD = 13.1) of burnout. There was a high degree of variation (28–87%) in PCP reports of performing tasks without reliance on team members. The top three tasks that PCPs reported performing without relying on their teams were evaluating patients and making treatment decisions (87%), tracking patient diagnostic data (80%), and responding to patient diagnostic and treatment data (80%). The middle three tasks that PCPs reported performing independently were intervening on patient lifestyle factors (68%), educating patients about disease-specific self-care activities (65%), and educating patients about medications (65%). The three tasks that PCPs reported performing with some reliance on the team were screening patients for diseases (32%), and receiving (28%) and resolving (43%) messages from patients. Between 50% and 57% of the PCPs reported high team functioning. PCP participants comprised mostly of physicians (69%), non-Hispanic whites (58%), and women (57%). The mean age was 50 years, with a mean of 11 years of VHA tenure. Just under half of the sample (47%) were from community-based outpatient clinics, and 43% of respondents were from one healthcare system.
Bivariate Linear Regression Analysis: Factors Associated with PCP Burnout
Results from the bivariate analysis (Table 3) indicated that PCP burnout was positively associated with PCP reports of performing two discrete tasks without reliance on team members: (1) intervening on patient lifestyle factors (b = 6.00, 95% CI = 2.17, 9.83, p = 0.002) and (2) educating patients about disease-specific self-care activities (b = 6.23, 95% CI = 2.78, 9.67, p < 0.001). Other variables significantly associated with PCP burnout (p ≤ 0.05) included team communication, team knowledge and skills, satisfaction with team, age, female gender, and VHA tenure.
Multivariable Linear Regression Analysis: Factors Associated with PCP Burnout
The multivariable linear regression analysis results (Table 4) indicate that PCP reports of intervening on patient lifestyle factors and educating patients about disease-specific self-care activities without relying on their teams were positively associated with PCP burnout (intervening on lifestyle: b = 4.11, 95% CI = 0.39, 7.83, p = 0.03; educating patients: b = 3.83, 95% CI = 0.33, 7.32, p = 0.03). In both models, effective team communication was negatively associated (p < 0.001) with PCP burnout. No other measures were associated with burnout.
DISCUSSION
Our study presents novel findings that identify specific primary care tasks that, when performed by PCPs without reliance on their teams, are associated with PCP burnout. Specifically, intervening on patient lifestyle factors and educating patients about disease-specific self-care activities were significantly associated with PCP burnout. These findings expand the current literature by providing evidence linking behavioral counseling and self-management education provided by PCPs with PCP burnout.34,35,36, – 37
In addition to the association with burnout, a variety of barriers to PCP delivery of behavioral counseling and educational interventions have been identified in the existing literature. These include limited time,22 , 34 , 40 , 41 limited availability of patient education materials and resources,38 , 40 low self-efficacy in influencing patient behavioral change,39 , 41 and perceived ineffectiveness of the interventions and skepticism regarding patient adherence to behavior modification.35 The association between these barriers and PCP burnout have not all been empirically tested in previous studies. However, researchers posit that these barriers, compounded by difficult patient encounters,35,36, – 37 can be a major source of frustration and stress, leading to job dissatisfaction and provider burnout.34,35,36, – 37 It is likely that the PCP participants from our study faced similar challenges and barriers that led to PCP burnout. Future research exploring the relationship between PCP delivery of these tasks and PCP burnout should examine the role that these factors play.
A growing body of literature reveals that intervention on patient lifestyle factors and patient education about disease-specific self-care activities by PCPs,34 , 38,39,40,41,42, – 43 as well as by nurses and other healthcare professionals,44 , 45 can improve patient outcomes. One potential strategy for reducing PCP burnout related to performing these tasks is to enable PCPs to share this responsibility with other team members. This transition, supported by adequate staffing, focused training, and standing orders, may lessen PCP burdens,22 , 46 which in turn, may help reduce emotional exhaustion and prevent PCP burnout.2 , 47 However, additional work is needed to evaluate how the sharing of these specific tasks affects PCP burnout, as well as the impact on staff burnout when they assume increased responsibility for such tasks.
Our findings also indicate that team communication has a robust and consistent association with lower PCP burnout. Controlling for team communication did not eliminate the association between certain tasks and burnout; nonetheless, it was negatively associated with PCP burnout. This finding is consistent with prior work documenting that effective team communication was one of several characteristics found in high-functioning primary care practices that mitigated PCP burnout.4 , 47 , 48 As such, this finding suggests another potential opportunity for quality improvement measures to promote teamwork and reduce provider burnout. Quality initiatives aimed at improving team communication through standardized task-sharing processes, workflow mapping, and appropriate staffing;2 , 47 , 49 co-location of team members;47 , 49 and regular huddles and team meetings, as well as, the use of information technology (e.g., instant messaging) for sharing of frequent and timely information, 49 may also improve communication effectiveness and enhance collaboration among PCMH team members, further mitigating PCP burnout. Additional research on primary care team task sharing and burnout should examine team practices used to facilitate team communication.
Finally, our findings provide some supporting evidence that task sharing among PACT members is taking place, 4 years after PACT implementation. Across the 14 tasks, there was a high degree of variation in the extent to which PCPs reported that they performed the tasks independently. For instance, while less than 20% of PCPs reported relying on their teams for certain patient assessment and treatment decision tasks (e.g., tracking and responding to patient diagnostic data), more than 60% of PCPs also reported that they relied on their teams for other tasks within the same category (e.g., screening patients for diseases). With better team communication and improved team function, we expect to see an increase in task sharing among team members over time. Subsequent longitudinal survey data will allow for assessment of such changes over time and will help to build a base of evidence for optimizing teamwork in primary care to support more efficient care delivery, while minimizing strain on PCPs and staff.
Limitations
The study has several limitations. First, this study was based on PCP perceptions rather than direct observations, potentially introducing the bias of self-reports, and thus affecting the reliability of the data. Further studies using other data collection methods, such as direct observation by an observer using a handheld electronic device (e.g., tablet) to document tasks performed, or the use of physiological sensors to detect PCP stress levels, may provide further insight on the relationship between PCP task performance and burnout.
In addition, reverse causality cannot be ruled out with the use of cross-sectional data. As with all cross-sectional studies, we cannot conclude a temporal cause-and effect relationship between the key study variables and PCP burnout. Therefore, a longitudinal study is needed to evaluate the relationship between theses variables and PCP burnout.
Finally, our study sample included primary care clinics within one VHA administrative region; therefore, our findings should be interpreted with some caution when generalizing to primary care clinics in non-VHA healthcare settings. However, previous studies investigating PCMH implementation have found that the challenges associated with PCMH implementation are common across primary care settings, and that the VHA primary care clinics and providers were representative of those from non-VHA primary care settings in other studies.3 , 9 , 24
Conclusions
PCP tasks of intervening on patient lifestyle factors and educating patients about disease-specific self-care activities, performed without reliance on their teams, were associated with PCP burnout. Four years after the implementation of the PCMH, only slightly over 30% of PCPs at the VHA reported relying on their teams for performing these tasks. Therefore, we believe there is an opportunity to reduce PCP burnout and ease the burden on PCPs by expanding the roles of nurses and other healthcare professionals to assume responsibility for these tasks. Findings from our study may guide the implementation of effective strategies aimed at redistributing tasks from PCPs to other members of the PCMH team to mitigate PCP burnout. Improving team communication represents another opportunity for reducing PCP burnout. Investing in resources and strategies aimed at developing and sustaining coherent PCMH teams that communicate well and function collaboratively will allow PCMH teams to fully deliver on the promise of team-based care.50
References
Hoff T, Sutcliffe KM, Young GJ. The Healthcare Professional Workforce: Understanding Human Capital in a Changing Industry. New York: Oxford University Press; 2017.
Ghorob A, Bodenheimer T. Sharing the care to improve access to primary care. N Engl J Med. 2012;366(21):1955–7.
Helfrich CD, Dolan ED, Simonetti J, et al. Elements of team-based care in a patient-centered medical home are associated with lower burnout among VA primary care employees. Gen Intern Med. 2014;29 Suppl 2:S659–66. doi: https://doi.org/10.1007/s11606-013-2702-z.
Meredith LS, Schmidt Hackbarth N, Darling J, et al. Emotional exhaustion in primary care during early implementation of the VA′s medical home transformation: patient aligned care team (PACT). Med Care. 2015; 53(3):253–60.
Lewis SE, Nocon RS, Tang H, et al. Patient-centered medical home characteristics and staff morale in safety net clinics. Arch Intern Med. 2012;172(1):23–31. doi:https://doi.org/10.1001/archinternmed.2011.580.
Reid RJ, Coleman K, Johnson EA, et al. The group health medical home at year two: cost savings, higher patient satisfaction, and less burnout for providers. Health Aff. 2010;29(5):835–43.
Nelson KM, Helfrich C, Sun H, et al. Implementation of the patient-centered medical home in the Veterans Health Administration: associations with patient satisfaction, quality of care, staff burnout, and hospital and emergency department use. JAMA Intern Med. 2014;174(8):1350–8.
Bertakis KD, Azari R. Patient-centered care is associated with decreased health care utilization. J Am Board Fam Med. 2011;24(3):229–39.
Nutting PA, Crabtree BF, Miller WL, Stange KC, Stewart E, Jaén C. Transforming physician practices to patient-centered medical homes: lessons from the national demonstration project. Health Aff. 2011;30(3):439–45.
Lu DW, Dresden S, McCloskey C, Branzetti J, Gisondi MA. Impact of burnout on self-reported patient care among emergency physicians. West J Emerg Med. 2015;16(7):996–1001. doi:https://doi.org/10.5811/westjem.2015.9.27945.
Williams ES, Manwell LB, Konrad TR, Linzer M. The relationship of organizational culture, stress, satisfaction, and burnout with physician-reported error and suboptimal patient care: results from the MEMO study. Health Care Manage Rev. 2007;32(3):203–12.
Shanafelt TD, Balch CM, Bechamps G, et al. Burnout and medical errors among American surgeons. Ann Surg. 2010;251(6):995–1000.
DiMatteo MR, Sherbourne CD, Hays RD, et al. Physicians' characteristics influence patients' adherence to medical treatment: results from the Medical Outcomes Study. Health Psychol. 1993;12(2):93.
Halbesleben JR, Rathert C. Linking physician burnout and patient outcomes: exploring the dyadic relationship between physicians and patients. Health Care Manage Rev. 2008;33(1):29–39.
Hojat M, Louis DZ, Markham FW, Wender R, Rabinowitz C, Gonnella JS. Physicians' empathy and clinical outcomes for diabetic patients. Acad Med. 2011;86(3):359–64.
Haas JS, Cook EF, Puopolo AL, Burstin HR, Cleary PD, Brennan TA. Is the professional satisfaction of general internists associated with patient satisfaction? J Gen Intern Med. 2000;15(2):122–8.
Kushnir T, Greenberg D, Madjar N, Hadari I, Yermiahu Y, Bachner YG. Is burnout associated with referral rates among primary care physicians in community clinics? Fam Pract. 2013;31(1):44–50.
Sirovich BE, Woloshin S, Schwartz LM. Too little? Too much? Primary care physicians' views on US health care: a brief report. Arch Intern Med. 2011;171(17):1582–5.
Altschuler J, Margolius D, Bodenheimer T, Grumbach K. Estimating a reasonable patient panel size for primary care physicians with team-based task delegation. Ann Fam Med. 2012;10(5):396–400.
Green LV, Savin S, Lu Y. Primary care physician shortages could be eliminated through use of teams, nonphysicians, and electronic communication. Health Aff. 2013;32(1):11–9.
Grumbach K, Bodenheimer T. Can health care teams improve primary care practice? JAMA. 2004;291(10):1246–51.
Yalnall KS, Ostbye T, Krause KM, Pollak KI, Gradison M, Michener JL. Family physicians as team leaders: “time” to share the care. Prev Chronic Dis. 2009;6:2.
Helfrich CD, Dolan ED, Fihn SD, et al. Association of medical home team-based care functions and perceived improvements in patient-centered care at VHA primary care clinics. Healthcare. 2014;2(4):238–44.
Edwards ST, Rubenstein LV, Meredith LS, et al. Who is responsible for what tasks within primary care: perceived task allocation among primary care providers and interdisciplinary team members. Healthcare. 2015; 3(3):142–9. https://doi.org/10.1016/j.hjdsi.2015.05.002.
Giannitrapani KF, Soban L, Hamilton AB, et al. Role expansion on interprofessional primary care teams: barriers of role self-efficacy among clinical associates. Healthcare. 2016. https://doi.org/10.1016/j.hjdsi.2016.03.004.
Rosland AM, Nelson K. Patient-centered medical home in the Veterans Health Administration. Am J Manag Care. 2013;19(7):e263–72.
U.S. Department of Veteran Affairs, Veteran Health Administration (VHA). VHA Handbook 1101.10, Patient Aligned Care Team. 2014. Available at: http://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=2977. Accessed July 13, 2016.
Maslach C, Jackson SE. The Maslach Burnout Inventory. 3rd ed. Palo Alto, CA: Consulting Psychologists Press; 1996
Willard-Grace R, Hessler D, Rogers E, Dubé K, Bodenheimer T, Grumbach K. Team structure and culture are associated with lower burnout in primary care. J Am Board Fam Med. 2014;27(2):229–38.
Welp A, Meier LL, Manser T. The interplay between teamwork, clinicians’ emotional exhaustion, and clinician-rated patient safety: a longitudinal study. Crit Care. 2016;20(1):110.
Ohman-Strickland PA, John Orzano A, Nutting PA, et al. Measuring organizational attributes of primary care practices: development of a new instrument. Health Serv Res. 2007;42(pt 1):1257–73.
Wageman R, Hackman JR, Lehman E. Team diagnostic survey development of an instrument. J Appl Behav Sci. 2005;41(4):373–98.
Doulougeri K, Georganta K, Montgomery A. “Diagnosing” burnout among healthcare professionals: can we find consensus? Cogent Med. 2016;3(1):1.
Whitlock EP, Orleans CT, Pender N, Allan J. Evaluating primary care behavioral counseling interventions: An evidence-based approach. Am J Prevent Med. 2002;22(4):267–84.
An PG, Rabatin JS, Manwell LB, Linzer M, Brown RL, Schwartz MD. Burden of difficult encounters in primary care: data from the minimizing error, maximizing outcomes study. Arch Intern Med. 2009;169(4):410–4.
Elder N, Ricer R, Tobias B. How respected family physicians manage difficult patient encounters. J Am Board Fam Med. 2006;19(6):533–41.
Lorenzetti RC, Jacques CM, Donovan C, Cottrell S, Buck J. Managing difficult encounters: understanding physician, patient, and situational factors. Am Fam Physician. 2013;87(6):419–25.
Ashenden R, Silagy C, Weller D. A systematic review of the effectiveness of promoting lifestyle change in general practice. Fam Pract. 1997;14(2):160–76.
Bao Y, Duan N, Fox SA. Is some provider advice on smoking cessation better than no advice? an instrumental variable analysis of the 2001 National Health Interview Survey. Health Serv Res. 2006;41(6):2114–35.
Bock C, Diehl K, Schneider S, Diehm C, Litaker D. Behavioral counseling for cardiovascular disease prevention in primary care settings: a systematic review of practice and associated factors. Med Care Res Rev. 2012;69(5):495–518.
Greiner KA, Born W, Hall S, Hou Q, Kimminau KS, Ahluwalia JS. Discussing weight with obese primary care patients: physician and patient perceptions. J Gen Intern Med. 2008;23(5):581–7.
Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient Self-management of Chronic Disease in Primary Care. JAMA. 2002;288(19):2469–75.
Lorig KR, Holman HR. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26(1):1–7.
Goldstein MG, Whitlock EP, DePue J. Multiple behavioral risk factor interventions in primary care: summary of research evidence. Am J Prevent Med. 2004;27(2):61–79.
Lin JS, O’Connor E, Whitlock EP, Beil TL. Behavioral counseling to promote physical activity and a healthful diet to prevent cardiovascular disease in adults: a systematic review for the US Preventive Services Task Force. Ann Intern Med. 2010;153(11):736–50.
Wagner EH. The role of patient care teams in chronic disease management. BMJ. 2000;320(7234):569.
Bodenheimer T, Sinsky C. From Triple to Quadruple Aim: Care of the Patient Requires Care of the Provider. Ann Fam Med. 2014;12(6):573–6. doi:https://doi.org/10.1370/afm.1713.
Leiter MP, Maslach C. The impact of interpersonal environment on burnout and organizational commitment. J Organ Behav. 1988;9:297–308.
Sinsky CA, Willard-Grace R, Schutzbank AM, Sinsky TA, Margolius D, Bodenheimer T. In search of joy in practice: a report of 23 high-functioning primary care practices. Ann Fam Med. 2013;11(3):272–8.
Schottenfeld L, Petersen D, Peikes D, et al. Creating patient-centered team-based primary care. Rockville: Agency for Healthcare Research and Quality. 2016.
Acknowledgements
Funding: Funding for this project was supported through a grant from the VA Veterans Assessment and Improvement Laboratory for Patient-Centered Care (VAIL-PCC) Patient Aligned Care Team (PACT) Demonstration Lab (no. XVA 65-018). Dr. Kim’s effort was supported through a grant from the Agency for Healthcare Research and Quality (#T32HS00046) and salary support from the Quality Scholars Program funded by the VA Office of Academic Affiliations (no. TQS 65-000). The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Rights and permissions
About this article
Cite this article
Kim, L.Y., Rose, D.E., Soban, L.M. et al. Primary Care Tasks Associated with Provider Burnout: Findings from a Veterans Health Administration Survey. J GEN INTERN MED 33, 50–56 (2018). https://doi.org/10.1007/s11606-017-4188-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-017-4188-6